Panvascular Disease in Familial Hypercholesterolaemia Treated with Endovascular Simultaneous Bilateral Carotid Stenting
Anand Alurkar1, Lakshmi Sudha Prasanna Karanam2, Shripal Shah3, Pandurang Mare4
1 Chief, Department of Neurointervention, King Edward Memorial Hospital, Pune, Maharashtra, India.
2 Consultant, Department of Neurointervention, King Edward Memorial Hospital, Pune, Maharashtra, India.
3 Consultant, Department of Neurointervention, King Edward Memorial Hospital, Pune, Maharashtra, India.
4 Consultant, Department of Neurointervention, King Edward Memorial Hospital, Pune, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Lakshmi Sudha Prasanna Karanam, Department of Neurointervention, KEM Hospital, Rasthapeth, Pune-411011, Maharashtra, India.
E-mail: drklsp@gmail.com
Familial Hypercholesterolaemia (FH) is a monogenic autosomal dominant disorder affecting 1 in 500 individuals. We report a case of 32-year-old female with FH, previously not on any treatment, who presented with recurrent bilateral Middle Cerebral Artery (MCA) territory strokes and dyspnoea on exertion due to severe panvascualar disease involving descending aorta, innominate, subclavian, common carotid, internal carotid and coronary vessels. Her complete clinical work up was done and was started on lipid lowering drug treatment and low calorie diet. She underwent simultaneous bilateral carotid stenting followed by coronary artery bypass surgery at a later date. In the present scenario we want to emphasize the importance of early detection and treatment of individuals with FH, failing of which results in premature and accelerated atherosclerosis causing multisystemic vascular disease with significant morbidity and mortality. Screening of first degree relatives is important owing to the autosomal dominant inheritance pattern of the FH.
Atherosclerosis, Endovascular treatment, Stroke
Case Report
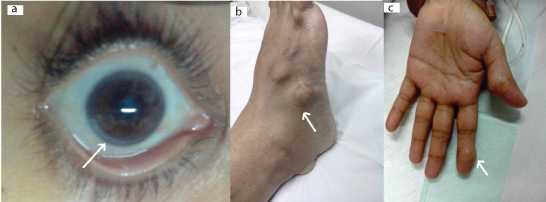
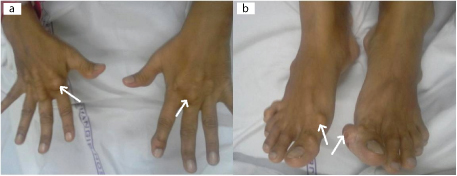
A 32-year-old Asian female presented with complaints of recurrent numbness and paresthesias due to recurrent bilateral Middle Cerebral Artery (MCA) territory Transient Ischemic Attacks (TIA) of one month duration. She also had dyspnoea on exertion since 6 months. Ophthalmological examination showed corneal arcus [Table/Fig-1a]. On clinical examination she had multiple widespread tendon xanthomas on hands and feet [Table/Fig-1b,c]. Electrocardiogram showed changes of ischemic heart disease. Her lipid profile revealed total cholesterol of 711mg/dL, LDL cholesterol of 542mg/dL and triglycerides: 98mg/dL. On further questioning and screening of first degree relatives, it was found that her 12-year-old son has xanthomas on feet and extensor surfaces of dorsum of hand [Table/Fig-2a,b]. His blood investigation showed total cholesterol of 300mg/dL, LDL cholesterol of 210mg/dL, triglycerides of 78mg/dL. Magentic Resonance Imaging (MRI) of her brain did not show any foci of restricted diffusion; however MR angiogram showed severe stenois of bilateral internal carotid arteries [Table/Fig-3a]. She had no history any prior drug treatment for hypercholesterolaemia. She was started on atorvastatin 80mg/day, ezetimibe 10mg/day, ecospirin 150mg/day and clopidogrel 75mg/day.
Clinical photograph showing the arcus (as shown by arrow in a) and xanthomas on feet (arrow in b) and hands (arrow in c).
Clinical photograph of 12-year-old son depicting xanthomas on the extensor surface of hand (arrow in a) and feet (arrow in b).
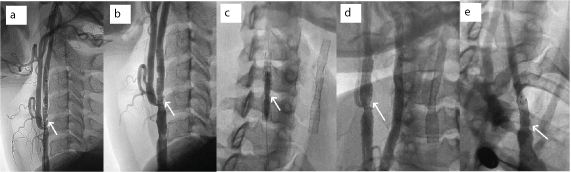
MR angiogram showing severe stenosis of bilateral carotid arteries (arrows in a). Digital subtraction angiogram showing widespread atheromatous disease of descending aorta (arrow in b), origins of right common carotid artery (arrow in c) and bilateral internal carotid arteries (arrows in d and e).
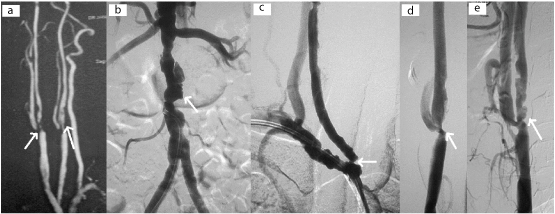
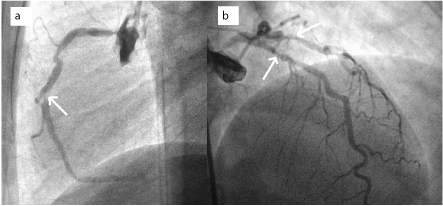
Digital subtraction angiogram done subsequently showed severe atheromatous disease of descending aorta with total occlusion of left subclavian artery [Table/Fig-3b]. Wide spread atheromatous disease was seen involving right subclavian artery, right common carotid artery (CCA), origins of right Internal Carotid Artery (ICA)and left internal carotid artery [Table/Fig-3c]. Significant stenosis of 80% was seen in right CCA origin and left ICA origin. A 95% focal stenotic lesion is seen in right ICA origin [Table/Fig-3d,e]. Intracranial cerebral circulation was normal. Coronary angiogram showed severe triple vessel disease [Table/Fig-4a,b]. In view of recurrent bilateral MCA territory TIA we first decided to treat the carotid artery disease. Simultaneous bilateral carotid stenting was done in the same sitting as described below.
Coronary angiogram showing severe disease of right coronary artery (arrow in a) and left anterior descending and circumflex arteries (arrows in b).
Procedure
An 8 french guide catheter was placed in the left common carotid artery. The stenotic segment was crossed with 0.014 wire and the lesion is stented with 8x6x40mm protégé self expanding stent under road map guidance [Table/Fig-5a]. A 6mm spider distal protection device was used to prevent preiprocedural thrombo embolic events. Thereafter guide catheter was placed in the innominate artery and right ICA lesion stented with 8x6x30mm protégé self expanding [Table/Fig-5b]. Angioguard protection device was used distally on the right side. Right CCA origin was stented with 8x30 mm precise stent [Table/Fig-5c-e]. Patient did not have any adverse effects during the procedure. Post procedure she developed hypotension which was treated with noradrenaline (2-4ug/min) infusion for 28 hours to maintain the Mean Arterial Pressure (MAP) at 80 to 90 mmHg in intensive care unit. She was shifted to ward on 4th postoperative day and subsequently discharged on 7th post procedure day. She did not have further episodes of TIAs after the procedure. Three weeks later she underwent coronary artery bypass surgery for her triple vessel disease which was uneventful. On her three months clinical follow up, she did not have any symptoms and reported no further TIAs. Her neurological examination was normal. Her lipid profile showed total cholesterol of 450mg/dl, LDL of 350mg/dl and TG of 75mg/dl. She was advised to continue the medical treatment with statins and antiplatelets as prescribed earlier.
Left commom carotid artery angiogram showing self expanding stent across the lesion (arrow in a) with good flow across the stented segment after deployment (arrow in b). Fluroscopic image showing the stent in the right internal carotid srtery (arrow in c) with good flow across the stent on contrast injection (arrow in d). The origin of the right common carotid artery is stented with self expanding stent with good antegrade flow (arrow in e).
Discussion
Familial Hypercholesterolaemia (FH) is an autosomal dominant condition affecting 1 in 500 individuals, caused due to mutations in the low density lipoprotein receptor gene located on chromosome 19 [1]. In heterozygous FH patient has one normal allele and one mutated allele. Clinically characteristic features of these patients include xanthomas, xanthelasma and premature arcus senilis [2]. According to simone broome register group, definite FH is defined as TC>290mg/dl,LDL >190mg/dl with presence of tendon xanthomas either in the patient or in first degree relative [3]. Xanthomas develop because of lipid leakage from the vasculature into the surrounding tissues. Our patient had xanthomas from the age of 15 years but she was not any medical treatment until she presented to us.
FH remains seriously underdiagnosed resulting in delayed treatment. It is important to identify FH at an early stage to prevent premature atherosclerosis [4] resulting in panvascualr manifestations as in the present case. Our patient did not had any other risk factors like diabetes mellitus, smoking and hypertension. Cicero et al., found that in females with heterozygous FH, the primary cause of death was thrombotic stroke [5]. The relative risk for death increased from 50 fold for men and 125 fold for women 20 to 39 years of age as per simon broome register [5,6]. When untreated, up to 85% of individuals with heterozygous FH will have a coronary event before the age of 65 years [6]. The high incidence of premature and accelerated athersoclerosis reduces life expectancy causing significant morbitity and mortality in these patients [6]. These patients were exposed to risks of high cholesterol since childhood. Lipid lowering drugs in these patients from an early stage reduced the risk of fatal events in these cases.
Premature coronary disease is a well known complication in these patients [7]. There are few reports in literature reporting increased incidence of stroke with heterozygous familial hypercholesterolaemia [4,8,9]. In the present case we actively intervened in acute event and treated with endovascular method by simultaneous bilateral carotid stenting in order to prevent the occurrence of major stroke, in view of frequent recurrent bilateral MCA territory TIAs. Simultaneous Bilateral Carotid Artery Stenting (SBCAS) is an elegant method of treatment for bilateral carotid artery disease with acceptable risks in select group of patients [10]. The sinus reflux due to baroreceptors, which is anticipated in these patients is well managed with noradrenaline infusion with successful clinical outcome.
Conclusion
Familial hypercholesterolaemia can cause panvascular disease. Accelerated atherosclerosis resulting in coronary and carotid artery disease in these patients is cause of significant morbidity and mortality. Early diagnosis and aggressive treatment with lipid lowering drugs is important and essential in order to decrease the progression of the disease. Screening of first degree relatives is important. This condition remains highly underdiagnosed resulting in delayed presentation as in our case. Knowledge of this condition is very much essential to the physician in clinical practice to detect it in an early stage and start medical management to prevent occurrence of fatal events.
[1]. Nemati MH, Astaneh B, Optimal management of familial hypercholesterolaemia: treatment and management strategiesVascular Health and Risk Management 2010 6(1):1079-88. [Google Scholar]
[2]. Winder AF, On the diagnosis of heterozygous familial hypercholesterolaemiaInt Cardiol 2000 74:13-14. [Google Scholar]
[3]. Rader DJ, Hobbs HH, Disorders of lipoprotein metabolism. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, et al editorsHarrison Principles of Internal Medicine 2008 Vol.217th edNew YorkMc Graw Hill Inc:2416-429. [Google Scholar]
[4]. Huxley RR, Hawkins MH, Humphries SE, Risk of fatal stroke in patients with treated familial hypercholesterolaemia: a prospective registry studyStroke 2003 34:22-25. [Google Scholar]
[5]. Cicero AFG, Braiato A, Dddato S, Sangiorgi Z, Gaddi A, A suggestion of familial hypercholesterolaemia heterozygosity clinical diagnosis based on epidemiological observations in a large Italian populationInt J Cardiol 2000 74:5-11. [Google Scholar]
[6]. Civeira F, Guidelines for the diagnosis and management of heterozygous familial hypercholesterolaemiaAtherosclerosis 2004 173:55-68. [Google Scholar]
[7]. Wittekoek ME, de Groot E, Prins MH, Trip MD, Buller HR, Kastelein JJP, Differences in intima-media thickness in the carotid and femoral arteries in familial hypercholesterolemic heterozygotes with and without clinical manifestations of cardiovascular diseaseAtherosclerosis 1999 146:271-79. [Google Scholar]
[8]. Vaughan CJ, Delanty N, Basson CT, Statin therapy and stroke preventionCurr Opin Cardiol 2001 16:219-24. [Google Scholar]
[9]. Kaste M, Koivisto P, Risk of brain infarction in familial hypercholesterolaemiaStroke 1988 19:1097-100. [Google Scholar]
[10]. Alurkar A, Karanam LP, Nayak S, Oak S, Simultaneous bilateral carotid stenting in a series of 9 patients: A single-center experience with review of literatureJ Clin Imaging Sci 2012 2:72 [Google Scholar]