Congenital inner ear malformations occur as a result of the arrest or aberrance of inner ear development due to the heredity, gene mutation or other factors. The malformations can exist in any part of the inner ear, 20% of which are bony structure malformations. The remaining 80% are membranous malformations which cannot be detected by radiologic diagnostic tools, are hidden inside the bony structure and the pathology lies at the cellular level making diagnosis difficult [1]. However, patients with bony malformations can readily be diagnosed by Computed Tomography (CT) and Magnetic Resonance Imaging (MRI). Diagnosing pathology in a small area of temporal bone where different combination of soft tissues and bone hide vital structure like middle ear, vestibulo-cochlear apparatus, facial nerve etc poses a special challenge to radiologist.
Most of the clinicians in our setting prefer to have both the modalities, keeping in mind, the advantages and disadvantages of each modality. But owing to the high cost of the investigations, need of sedation and ‘acceptable’ level of difference in CT/MRI in finding the pathologies. There is always a question in the mind of radiologist that which of following imaging modality would be best or is there a real need for the use of dual modes investigations. So far both the modes are used clinically hoping it to be complementary.
To compare pre-operative imaging findings of both MRI and HRCT (High Resolution Computed Tomography) temporal bone and to find the best modality of choice in patients with bilateral profound Sensorineural Hearing Loss (SNHL).
Materials and Methods
Study Design: This was a prospective, longitudinal, observational study conducted between June 2010 to November 2012. Total 72 patients (144 temporal bones) included in this study.
All the patients underwent HRCT (16-slice, spiral; Bright speed, GE) and high field MRI study (SIGNA HDx 1.5T Series, GE). HRCT with the following parameters: 0.75-mm collimation, 0.625-mm section thickness, 140 kVp, 120 mAs, pitch of 0.8, a 15-cm Field of View (FOV), and a 512 x 512 matrix. The initial data sets were then reconstructed at 0.1-mm intervals.
MR scanning is performed with following sequences.
3D FIESTA (Fast Imaging Employing Steady-state Acquisition) axial and for better image resolution of nerves oblique parasagittal view (FIESTA) which is perpendicular to the plane of the Internal Auditory Canal (IAC) is taken on both sides. The cochlea can be further evaluated by generating MIP images.
For screening of brain T2W (TE 102.9ms, TR 4780ms) sequence in Axial plane is taken.
Results
A total of 72 patients (a total of 144 temporal bones/cases) were included over 2½ years of time. Each of the temporal bone was analysed separately. There were 45 male patients and 27 female patients. Majority of the patients (60) were mute at the time of attending the ENT surgeon.
All patients were in the age between 6 months to 20 years. Most of the patients belonged to the age group of 1-5 years, 17 patients of which were of 3 years and 14 were of 2 years of age.
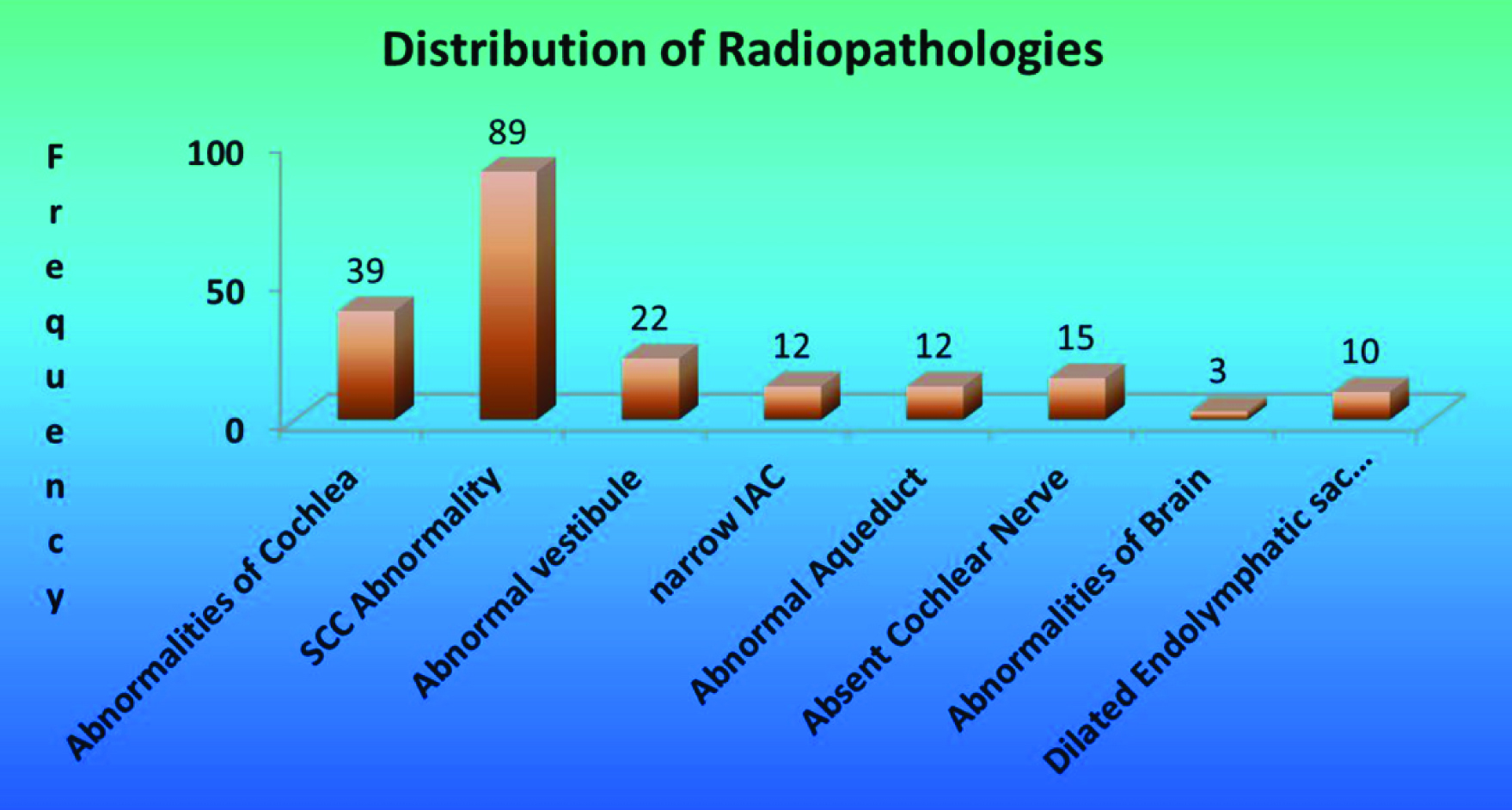
The common pathologies detected in our study were Semicircular Canal (SCC) abnormality (89 cases) followed by abnormalities of cochlea (39 cases) [Table/Fig-1].
Showing distribution of various radio pathologies.
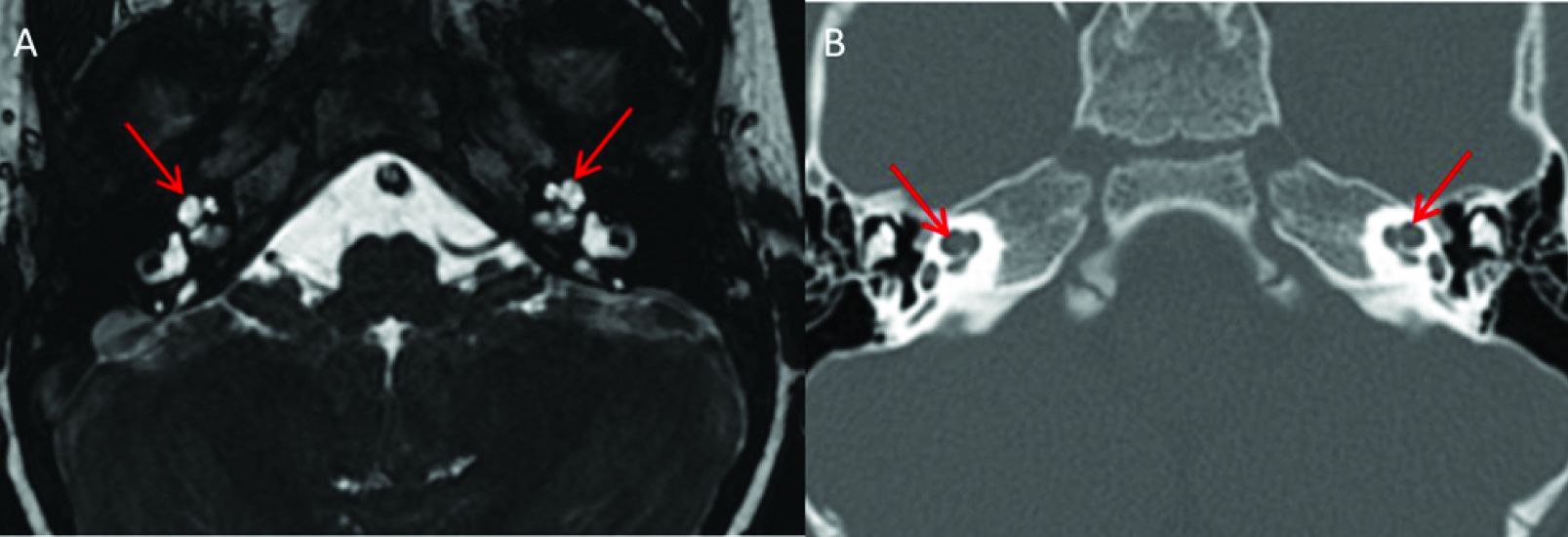
A comparison of pathologies detected by either imaging modality was analysed as represented in the above table [Table/Fig-2]. Most common cochlear abnormality was Mondini’s deformity [Table/Fig-3]. Sclerotic lesions with abnormal hyperdensity and ossified lesions were only detected by CT but not with MRI, whereas only MRI could diagnose focal fibrosis of the cochlea.
Radio-pathology of cochlea with CT/MRI.
| Pathology | CT (N=144) | MRI (N=144) |
|---|
| Normal | 107 | 104 |
| Dysplastic, featureless cochlea in the form of 1 ½ turns with a fusion of apical & middle turns forming cystic apex- incomplete partition type II (Mondini’s deformity) | 14 | 14 |
| Loss of normal internal configuration of cochlea & vestibule- (incomplete partition type I) | 9 | 9 |
| Abnormal hyperdensity with sclerosis | 6 | 0 |
| Cystic cavity representing the cochlea and vestibule, but without showing any differentiation into cochlea and vestibule- (common cavity deformity) | 4 | 4 |
| Complete absence of inner ear structures- (Michel’s deformity) | 2 | 2 |
| Ossified lesions (Labyrinthitis ossificans- late stage) | 2 | 0 |
| Loss of normal SI | 0 | 9 |
| Focal fibrosis at the junction of basal turn of cochlea and vestibule-(Labyrinthitis ossificans- early stage) | 0 | 2 |
Image A: Axial 3D FIESTA image showing Mondini’s deformity on either side in the form of one and half turns (red arrows) and image B, axial CT scan of the same patient showing the similar deformity (red arrows).
Comparison of CT and MRI in Pathologies of Semi-Circular Canals
The observations reported from CT were normal SCC in 61 (42%) temporal bones. The CT evaluation of SCC showed that dysplastic lesions of SCC were commonly seen in 45 (31%) followed by hypo plastic lesions in 15 (10%). There was one case where SCC was not visualized as in CT.
In contrast, the observations reported from the MRI were normal SCC in 55 (38%) temporal bones. The most common pathologies detected were dysplastic lesions of 50 (35%) cases followed by complete/partial absent lesions in 17 (12%) and hypo plastic lesions in 15 (10%). The MR imaging could not diagnose sclerotic lesions of SCC, which was picked up by CT scan in 4 cases. Focal fibrosis and loss of signal intensity was well identified by MRI, which was not similar with CT imaging.
Comparison of CT and MRI in Pathologies of Vestibule
From the study out of 144, 114 (79%) cases were normal in CT, whereas 112 (78%) in MRI. In comparison with cochlea and SCC, vestibular pathologies were less in number. The dilated dysplastic vestibule was found in 7 (5%) cases in CT and 9 (6%) cases in MRI. Dysplastic vestibule is seen in 8 (6%) cases in both CT and MRI. The vestibule was absent in 5 cases in CT scan, 2 cases in MRI.
Vestibular pathologies diagnosed by both modalities were almost similar except for cases like focal fibrosis in 2 temporal bones and loss of normal signal intensity in 3 temporal bones, which were diagnosed only by MRI but not with CT scan. Conversely, only CT scan could diagnose sclerotic lesions of vestibules with complete or partial obliteration.
Vestibulo–Cochlear Nerve (VCN)
Absent VCN was found in 15 cases, which was detected only by MRI. Fusion of superior and inferior vestibular nerve was seen in 11 cases.
Internal Auditory Canal (IAC)
Ten cases of narrowed IAC were seen in our study, which was less than 2mm in diameter. Most of them were associated with absent VCN. Two cases of widened IAC were seen.
Jugular Bulb
High riding jugular bulb was seen in 2 patients.
Screening of Brain (Axial T2)
Conditions like arachnoid cyst, scaphocephaly, leukodystrophy and cystic encephalomalacia each was observed in single patient respectively.
Discussion
Present study illustrates imaging findings in patients with SNHL. The current study focused all anomalies of inner ear including SCC abnormality, vestibular, endolymphatic duct and sac, aberrant vascular loop, mastoid air cells, middle ear, normal anatomic variants apart from cochlear nerve.
The male preponderance in children with SNHL (62.5% in our study) has been commented on by several authors [2,3]. No statistically significant sex differences in terms of either severity of hearing loss or CT findings were found in our study. All the patients were presented with bilateral profound SNHL and maximum number of our patients were mute.
In present study, most common abnormality of cochlea was Mondini’s and Mondini’s variants. Mondini first described this anomaly in 1791 [4]. The difference between incomplete partition (Mondini) and severe incomplete partition (Mondini variant) is of clinical interest because incomplete partition might present with some residual hearing [1]. According to the literature, incomplete partition of the cochlea defined as a cochlea with 1½ turns. In severe incomplete partition, only the basal turn of the cochlea is present [1,5]. Both CT and MRI were able to differentiate these abnormalities.
Johannes P. Westerhof et al., studied congenital malformations of the inner ear and the vestibulo-cochlear nerve in children with SNHL. Twenty one children (42 inner ears) were studied with high resolution MR and helical CT examinations who were candidates for cochlear implants. They identified 99 malformations. Mondini abnormality and Mondini variants (12/42) and fusion of the lateral or superior SCC with the vestibule (12/42) were common imaging findings. Rudimentary or absent vestibulo-cochlear nerve was found in 9 of 21 patients which was demonstrated by MRI [6].
As compared to their study, maximum varieties of malformations were present in our study, possibly due to number of patients (21 patients, 42 inner ears) they studied was less.
In present study, SCC abnormality was most commonly encountered. Dysplasia of SCC is most common and is seen in 28%, hypoplasia of SCC is seen in 10% of cases. Dysplasia and hypoplasia of lateral SCC was most commonly seen. Dysplasia of lateral SCC was most commonly associated with dilated vestibule. SCC and vestibular abnormalities are frequent findings in cases with SNHL [1], while deformed or absent SCC is the hallmark of the CHARGE association [7].
Bamiou DE et al., studied temporal bone computed tomography findings in bilateral SNHL. It was retrospective study. They studied only with CT in contrast to our study, where both CT and MRI were used for evaluation. Dilated vestibular aqueduct was the most common CT abnormality in their series (10 of 116 cases), abnormalities of the SCC were the second commonest abnormality in their series, occurring in 7.75% (9 of 116 cases) [3].
One of the most important findings in our study is that MRI helps full appreciation of the normal anatomy and anomalies of the vestibule-cochlear nerve within the internal auditory canal. For visualization of nerve, 3D FIESTA Axial sequence, oblique parasagittal view was taken using a small FOV. Presence of nerve is very important for cochlear implant candidates. A missing VCN is contraindication for cochlear implant as this nerve is required to conduct the cochlear implant impulses.
Cochlear nerve was absent in 15 cases. Among them 7 cases were of thin dysplastic nerve and 2 cases of thin cochlear nerve. This abnormality was detected only by MRI.
MRI is superior to CT in the evaluation of VCN. Komatsubara et al., examined the dimensions of the Cochlear Nerve Canal (CNC), the structure that runs from the base of the modiolus to the fundus of the Internal Auditory Canal (IAC). They found that in those with CNC measuring <1.5 mm on CT, MRI diagnosed cochlear nerve deficiency with 88.9% sensitivity and specificity [8]. Roche JP et al., also reported normal bony anatomy, including normal-sized IAC and CNC, on CT in cases where MRI revealed a nonexistent or hypoplastic cochlear nerve. The CT imaging alone is not a reliable modality to determine cochlear nerve deficiency [9].
Cochlear Nerve (CN) deficiency is not an uncommon cause of congenital hearing loss as suggested in a study by Adunka OF et al., [10]. They concluded that IAC morphology is an unreliable surrogate marker of CN integrity as most ears with CN deficiency had normal IAC morphology whereas two ears with small IACs had CNs present [10]. This study also shows that high-resolution MRI, rather than CT imaging, should be performed in all cases of profound hearing loss in children. Resolution of MRI currently remains unsatisfactory in ears with small IACs. Mackeith S concluded that patients with cochlear implantation should undergo MRI initially as it detects all abnormalities that are critical to patient management. CT is helpful in patients with a history of meningitis, severe middle ear disease or dysmorphic syndromes. These kinds of patients should undergo both CT and MRI [11].
This study was comparable to present study as CT was helpful in detection of middle ear pathology, status of mastoid air cells, facial nerve canal and MRI was helpful for early fibrosis, VCN.
Bath AP et al., predicted the patency of the cochlea in children undergoing cochlear implantation by using HRCT scans. High degree of accuracy (87%) in predicting a patent cochlea was achieved by CT in patients who had normal inner ears. Degree of ossification was considerably under-estimated (15% of cases) causing major difficulties at the time of surgery. Even though HRCT provides great clarity and fine detail, it has its limitations. Further information may be obtained by MRI [12].
Parry DA et al., studied advantages of MRI over CT in Preoperative Evaluation of Paediatric Cochlear Implant Candidates. Among the 112 temporal bones imaged with MRI, abnormalities in following structures were noted: cochlear turns (32%), abnormal signal in the modiolus (30%), vestibulae (23%), endolymphatic ducts (16%), endolymphatic sacs (15%), cochlear nerves (12%) and brain (29%). HRCT findings were combined with radiologic opinion and compared with MRI findings. The percentages of abnormalities identified by HRCT when compared with MRI are endolymphatic duct 100% (18/18), vestibulae 88% (23/26), cochlea 42% (15/36), modiolus 35% (12/34), and endolymphatic sac 6% (1/17) [13]. They concluded that MRI is more sensitive and specific compared to HRCT in diagnosing soft tissue and nerve abnormalities in the inner ear. The abnormalities detected with MRI are more likely to aid the implantation process. This study was comparable to our study, as MRI detected soft tissue and intracranial abnormalities in our study.
Caye-Thomasen P et al., studied cochlear ossification in patients with profound hearing loss following bacterial meningitis [14]. In this retrospective study they concluded that cochlear ossification occurring after bacterial meningitis is associated with causative pathogen. It is not related to age at disease or time of evaluation. Signs of progressive ossification were found in cases which underwent repeated scans particularly if ossification was present at the first scan.
In present study, 4 cases of labyrinthine ossificans were observed, where only 2 cases were detected by CT and rest of the 2 cases were in early stage, which were only detected by MRI. In our study etiology may be post-inflammatory sequela that is post meningitis.
Bamiou DE et al., recommended that all children with SNHL should undergo imaging studies (CT or MRI) of the temporal bones. The decision to perform CT vs MRI depends on several factors like availability of equipment, expertise, and other management considerations. However, candidates for cochlear implant require both [3].
Seitz and colleagues found that MR imaging provided additional information to CT in 10 (39%) of 26 patients who had both temporal bone CT and MR imaging before cochlear implantation [15].
Sennaroglu et al., used CT as the primary imaging modality for cochlear implant candidates, but they also obtained MR images in the presence of total hearing loss, narrow internal auditory canal, or inner ear malformations to demonstrate the presence of the eighth nerve [16].
Ellul et al., concluded that fast spin-echo MR imaging should be the single imaging study of choice for the preoperative evaluation of most cochlear implant candidates [17]. Other authors have also recommended MR imaging of the brain and temporal bones as part of the evaluation of cochlear implant candidates [15,18].
Westerhof JP et al., suggested the combined use of CT and MR imaging to study cochlear implant candidates [6].
Study conducted by Pooja VD et al., highlights importance of pre-operative evaluation in cochlear implant patients as it provides critical information about cochlear status and rules out other causes where cochlear implantation is not possible or contraindicated [19]. Both CT and MRI modalities were used in their study as they are complementary to each other.
Tougan Taha et al., concluded that combined MDCT/MRI imaging procedure helps the clinician to better selection of the patient, improve their surgical approach and the choice of electrode [20].
Fusion of superior and inferior vestibular nerve was found in 11 cases in our study, however no studies were found related to this condition. These features were not having any significance related to cochlear implant surgery.
Limitation
There were some limitations in our study like, we didn’t correlate our findings with surgical findings and didn’t focus on risk factors for congenital SNHL. Patients with normal study were excluded in our study, so couldn’t correlate with control group.
Conclusion
The ideal imaging algorithm in children with bilateral profound SNHL still appears to be contentious. Neither CT nor MRI of the brain and temporal bones appears to be adequate as the sole imaging modality of choice in all children.
But using both MRI and HRCT modalities judiciously in selected cases can fill each other’s lacunae. The two modalities in combination can provide the cochlear implant surgeon the information which is surgically relevant. Thus, it helps surgeon to choose best ear for cochlear implantation. So based on our study, both modalities are preferred preoperatively in cochlear implant patients rather than single modality.
Imaging of the complex ear involves minute findings and also time consuming. It often influences major and very expensive decisions. Requirement of trained and dedicated radiologists is the need of the hour, who are an integral part of the cochlear implant program. With the high expenses of cochlear implants, the vulnerability of young patients and the high expectations of their parents, every step should be taken to avoid unnecessary operations and to identify patients who will benefit from this surgery.