Accurate measurement of body temperature and its fluctuations may greatly influence the physician’s diagnostic accuracy and therapeutic decisions [1]. Accurate temperature patterns need to be reflected in the temperature chart, if not; it may affect the diagnosis as well as delay the treatment. Conventional temperature recording is one of the oldest clinical methods and is routinely practiced in the clinical setup [2]. It is primarily used to monitor the temperature status of the patient [3]. However, in conventional recording, the peak temperature is significantly under-estimated and often overlooked [4]. This might be because of periodic recording of body temperature every 8-12 hours [4] and it may remain inadequate even with recording of temperature at 6-hour intervals. Continuous temperature recording is an alternative method of temperature monitoring. However, as of now, continuous temperature recording is routinely used during general anaesthesia, open-heart surgery and in Intensive Care Unit (ICU) patients [5–7] and not yet fully practiced in general medical wards.
Axilla and oral sites are convenient for temperature recording while rectal site is generally considered as a reference standard. However, except for the axillary site, these sites are not convenient to measure the temperature by continuous method. The continuous oral and rectal temperature recordings are cumbersome and are generally not well accepted by the patient. Clinical decisions are made based on, mainly core body temperature rather than surface skin temperature. In such cases, temperature measured at axillary site does not reflect the core body temperature [8]. Studies comparing tympanic temperature with oesophageal temperature reported that the tympanic temperature correlates well with the oesophageal temperature and can be considered as an alternative measure of core body temperature [9–11]. Moreover, tympanic membrane is positioned near the carotid artery, which supplies blood to the hypothalamus [9–11]. It can be measured continuously and noninvasively, except in cases of perforation of eardrum and otitis media [12].
Varela et al., reported that continuous tympanic temperature monitoring is feasible and provides more accurate measurement of body temperature than conventional temperature recording at axillary site in patients admitted to general ward [4]. However, the reliability of conventional skin surface temperature recording has not been established in comparison to the continuous tympanic temperature recording method. We hypothesized that 24-hour non-invasive continuous tympanic temperature recording will yield more vital information relevant to the clinical practice by capturing minute to minute temperature fluctuations, which might not have been observed by conventional skin surface temperature recording. The aim of the study was to compare the conventional skin surface temperature versus continuous tympanic temperature recordings in hospitalized patients.
Materials and Methods
A cross-sectional study was conducted at a tertiary care teaching hospital during the period from April 2014 to October 2015. Fifty-five patients with a history of fever (either due to infectious or non-infectious causes) admitted to the general medicine ward were recruited. Sample size calculation was 52; it was done by using OpenEpi software (version 3.01) by keeping 95% confidence interval, 90% power, minimum mean difference of 1 as a clinically relevant difference and standard deviation of 1.40 and 0.70 values of axillary and tympanic temperature. Subjects aged between 18 to 65 years were included, while subjects who were on antipyretics were excluded from the study. Simultaneous body temperature recordings were carried out by conventional and continuous recording methods. Continuous temperature recordings were performed using a tympanic temperature probe placed at external auditory canal. Before starting the continuous temperature recording, ear examination was carried to rule out perforation or discharge in subject’s ear. The tympanic temperature probe (WIT-B-II Adult) consisted of a 400 series thermistor sensor with an accuracy of ±0.1°C at 37°C and ±0.2°C between 25°C to 45°C. The tympanic temperature probe was gently inserted into the external auditory canal projecting towards the tympanic membrane and the other end of the probe was connected to the temperature-monitoring device (TherCom, Innovatecsc®). The tympanic temperature probe contained soft cell memory foam, which covered the ear canal and protected against the influence of ambient air. Tympanic temperatures were recorded for 24 hours at every minute and were stored in the device. The conventional temperatures of the same patients were noted from the temperature charts, which were recorded by nursing staff at specific times, 12:00 noon, 8:00 PM and 5:00 AM. The conventional temperatures were recorded using mercury thermometer in the axilla. The study protocol was approved by the Institutional Ethics Committee. Informed consent was taken from each of these participants after explaining the detailed procedure of the study and risks associated with the experiment and confidentiality of the participants were maintained.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS) version 15, Chicago, IL. Mean and standard deviations of temperature were calculated for both continuous and conventional methods. Peak temperature differences between the two methods were compared by applying Independent sample T-test. Intra-Class Correlation (ICC) test was performed to assess the reliability between the two temperature-monitoring methods and p<0.05 was considered as significant.
Results
The present study included 55 patients with fever. Out of 55 patients, 43 were diagnosed as infectious origin such as tuberculosis (18), bacterial (10), enteric fever (8) and dengue fever (7) and 12 were non-infectious aetiology including systemic lupus erythematous (3), Hodgkin’s lymphoma (2), non-Hodgkin’s lymphoma (2), acute myeloid leukaemia (2) and single cases of stills disease, aortoarteritis and pancreatitis. The mean age of the patients was 41.34 ± 15.53 years.
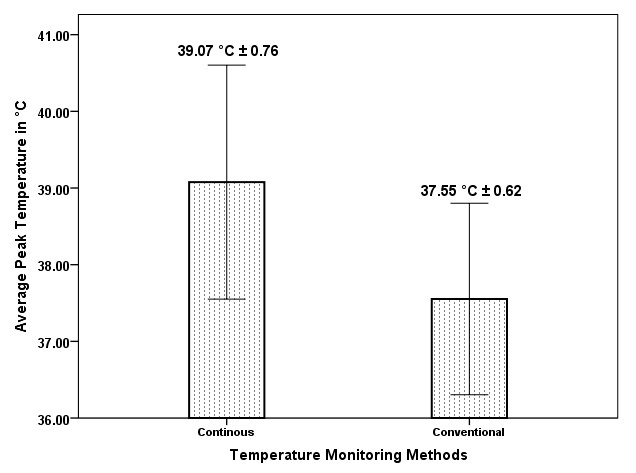
The average peak temperature was 39.07°C ± 0.76°C in the continuous tympanic temperature recording, and 37.55°C ± 0.62°C in the conventional axillary temperature recording [Table/Fig-1]. A statistically significant and clinically relevant difference of 1.52°C [p< 0.001, 95% CI (1.26 -1.78)] was noted between the temperatures recorded by the two different methods.
Average peak temperature difference between continuous and conventional recording methods.
Intraclass Correlation Coefficients (ICCs) between continuous and conventional temperature readings at 12:00 noon was 0.540 [p<0.003, 95% CI (0.213-0.731)] and showed moderate reliability. The coefficients at 8:00 PM and 5:00 AM were 0.425 [p<0.003, 95% CI (0.036-0.677)] and 0.435 with [p<0.013, 95% CI (0.060-0.664)], respectively. However, these coefficients showed poor reliability.
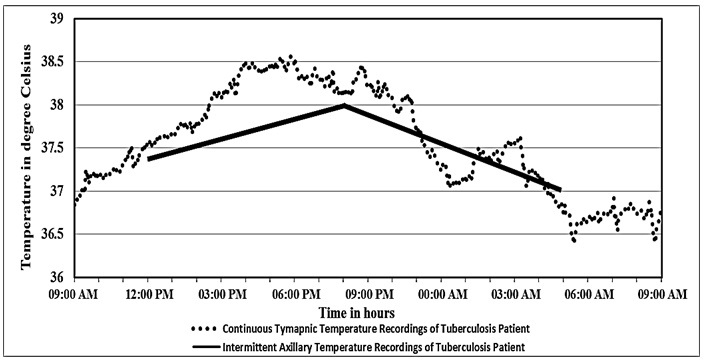
In continuous temperature recordings, 85.45 % of fever patterns were clearly intermittent in nature, whereas in conventional recordings, 56.36% of fever patterns were intermittent in nature and the remaining 29.09% of intermittent fever patterns were not captured by the conventional method. In 85.45% of the patients, an early morning temperature surge was captured by continuous recording method [Table/Fig-2]. However, in conventional recording method, this temperature surge was observed in only 40.00% of the patients.
Comparison of continuous tympanic and axillary temperature recordings of a tuberculosis patient.
Discussion
The peak temperature is not captured by most of the conventional monitoring methods [4]. Moreover, the conventional temperature recordings appear to be unreliable since they do not capture the temperature fluctuations and also underestimated the peak temperature by about 1.52°C in our study, which may have major therapeutic implications. Usually paracetamol is given to patients when body temperature exceeds 38.3°C /101 °F. However, due to the inaccurate conventional temperature monitoring method, paracetamol dose is not provided in a timely manner to patients in need of it.
We also found that there was a poor agreement between continuous tympanic and conventional axillary temperature monitoring methods at specific time intervals. The tympanic temperature recorded by continuous monitoring method appears to be more reliable than axillary temperature by conventional recording and it is not affected by factors such as vasomotor activity and ambient temperature. However, these factors routinely influence the temperature measurement taken by conventional method at axillary site [13].
Further, the conventional recording method did not capture the true temperature pattern whereas the continuous temperature recording does reflect the true temperature pattern. Our study showed that conventional temperature recording failed to identify the true nature of intermittent fever in one-third of the patients who actually had intermittent fever, which was however clearly identified by continuous temperature recording. It suggests the possibility that temperature touching the baseline is more appropriately reflected by continuous method and not by conventional method [Table/Fig-2]. Our observations are consistent with the results of a previous study which reported that conventional temperature recordings overlooked fever spikes which could significantly affect the physician’s diagnostic approach towards the patient [4]. In such cases, the continuous monitoring method may aid in evaluation of fever and appropriate treatment.
The present study compared two simple non-invasive temperature recording methods. Conventional temperature monitoring at axilla is a common method of recording and routinely practised in all healthcare settings [14]. However, continuous temperature monitoring at tympanic site is presently limited to ICU patients and surgical patients, probably because the importance of continuous recording over conventional recording is realised by the physician [15]. Since we wanted to explore utility of continuous temperature recording in routine clinical practices, we opted for the simple non-invasive temperature sites instead of temperature recordings at rectal and oral site. Previous studies have suggested that the possibility of reading errors was higher at rectal and oral sites due to food, fluids and placement of the device [1,2]. Further, rectal temperature recordings are cumbersome, disliked by patients, have chances of perforation, and require frequent sterilization of the device. Moreover, the risk of cross-contamination and infection cannot be ignored [1]. Acceptance of the continuous monitoring method by the patient is generally good, and while many of the patients had minimal irritation, there were no withdrawals from the study.
The continuous monitoring method has many advantages over conventional method. Apart from recording the true temperature fluctuations, the continuous temperature recording method is more practical and needs less nursing assistance [4]. Currently, portable continuous temperature monitoring device (TherCom®) that was used in our study is not available in India. It requires an initial investment for the portable temperature data logger, which costs approximately 30,000 rupees (454 US Dollars). Also, a disposable temperature probe is required, which costs around 75 to 100 rupees (1.13 to 1.5 US Dollars) and this can be used for a single patient during his entire hospital stay. The cost of mercury-in-glass thermometer is about the same as that of the tympanic temperature probe (75-100 rupees or 1.13- 1.5 US Dollars). However, mercury-in-glass thermometer requires special care for disposal, due to the high toxicity of mercury [2]. In fact, the National Accreditation Board for Hospitals and Healthcare Providers of India (NABH) has suggested the replacement of mercury thermometers to avoid risks associated with accidental mercury spills [16]. PortableTherCom® device is feasible to use in inpatient settings to identify fever spikes and in outpatient consultations to notice febrile episodes which are not detected during the physical examination [17].
Advanced technology is constantly improving the feasibility and accuracy of body temperature monitoring. It is possible that the existing continuous monitoring devices would be able to provide real time temperature data on mobile devices and have additional choices of Wi-Fi or bluetooth [4,17]. Availability of wireless data transfer and long lasting durable battery options makes it more convenient to record temperature continuously for long time. This would also allow access to the patient’s centralised temperature data at any time, which improves patient care. In addition, monitoring devices now have the option to set an alarm that beeps when the temperature reaches a particular range. However, the traditional thermometer lacks these options. Generally, patients were quite tolerant to the procedure and were found to have minimal irritation during non-invasive continuous tympanic temperature recording. Furthermore, continuous monitoring did not affect the patient’s sleep which is frequently seen in conventional recording method. In conventional monitoring method, intermittent recordings were performed every 8-12 hours [4]. A single appropriate measurement needs a minimum of 8-10 minutes, which is time consuming and requires frequent nursing assistance [4]. On the other hand, in continuous monitoring method, initial nursing assistance is required for proper placement of probe and is sufficient to obtain accurate temperature readings at every 15 seconds or minute-to-minute interval over 24 to 48 hours [17].
Limitation
A possible limitation of the study was the use of a relatively small sample size. However, we feel that the sample size was adequate to represent various clinical scenarios and other causes of fever. We also need to expand the study of feasibility and diagnostic utility of continuous temperature monitoring method for domiciliary care.
Conclusion
The body temperature is one of the oldest vital signs to be monitored, but technological innovations have not yet translated into a better interpretation of temperature fluctuations. Even now, most of the hospitals depend on mercury thermometers and temperature recording is performed once every 8-12 hours. On the other hand, the use of a non-invasive continuous temperature recording method can capture minute-to-minute temperature fluctuations and actual temperature patterns, which may help clinicians in diagnostic workup of the patients with fever. There is a wide unexplored opportunity for continuous recording of the temperature, which is likely to be as useful as pulse oximeter, holter monitoring of heart rate and Electrocardio Graphic (ECG) changes, and 24 hour ambulatory blood pressure monitoring in routine patient care.
Conflict of Interest: Authors disclosed no conflict of interest.