Skin is an uncommon site for metastasis with only 0.7-9% of all patients with cancer being affected when compared to other organs. Generally, the time lag between the diagnosis of primary malignancy and the recognition of the skin metastases is long, but sometimes these metastases may be the first indication of otherwise clinically silent visceral malignancies as seen in our case. In cholangiocarcinomas, the occurrence of cutaneous metastases is extremely rare. Their most common sites of metastasis are visceral organs i.e., lungs, bones, adrenal glands and brain. The present case is unique and describes a patient with metastatic cutaneous thigh nodule as the first sign of cholangiocarcinoma. The early recognition of skin metastasis of previously undiagnosed cancers is critical for timely intervention as it indicates poor prognosis with overall survival after cutaneous metastasis of only few months. Very few reports of cutaneous metastases from cholangiocarcinomas have been published. Also, most of these were derived from direct tumour seeding by percutaneous procedures whereas our case showed distant metastasis to thigh. Extensive literature search showed ours to be the first case of cholangiocarcinoma presenting as thigh nodule where Fine Needle Aspiration Cytology (FNAC), histopathology and immunohistochemistry helped in clinching an early diagnosis and judicious management of a patient with unsuspecting thigh nodule.
Case Report
A 45-year-old man was admitted to our hospital with complains of weight loss, abdominal distension and a Painless subcutaneous nodule on his left thigh for 2 months. Apart from the presence of ascitis and subcutaneous nodule, the findings of the physical examination were normal. No icterus was present. Laboratory analysis showed the following results: Total Leukocyte count (TLC) 9,500/mm3, haemoglobin 7.6 gms/dL; Liver Function Test (LFT) showed: total bilirubin levels of 0.5 mg/dl, serum aspartate transaminase and alanine aminotransferase levels wee 256IU/L and 280 IU/L, alkaline phosphatase 332 IU/L.
A clinical impression of a soft tissue nodule of thigh was made and an FNAC was requested. The skin lesion on the left thigh was a solitary, firm, fixed, round, painless nodule measuring 3x 2.5x 1.5 cm in size. FNAC yielded a whitish aspirate. Cytology smears showed moderate cellularity with the cells being scattered singly and in small clusters and at places, acinar pattern was seen. The cells were pleomorphic with high nuclear cytoplasmic (N:C) ratio, hyperchromatic nuclei and abundant basophilic cytoplasm along with few multinucleated cells [Table/Fig-1a,b]. Background showed tumour diathesis. The cytological findings were suggestive of an adenocarcinoma, most likely metastatic. However, possibility of a primary adnexal lesion could not be ruled out and biopsy with Immunohistochemistry (IHC) was advised. After excisional biopsy, a nodule covered with skin and measuring 3x2.5x1.5cm in size was received [Table/Fig-1c (Inset)].
FNAC smears from thigh nodule show: a. Moderately cellular smear with pleomorphic cells in loose clusters (Giemsa, x100); b. Cells in acini with cytological atypia (Giemsa, x400); c. Histopathological sections showing metastatic adenocarcinoma in sub epidermal zone of thigh nodule (H & E, x100); Inset: Skin covered thigh nodule; d. Cells show nuclear pleomorphism and atypical mitoses as indicated by arrow (H&E, x400).
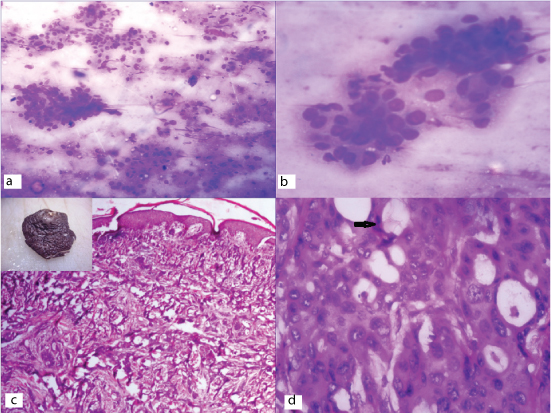
Histopathologic examination showed a lining of keratinized stratified squamous epithelium. The subepithelial zone showed cells predominantly in acinar pattern lying in a desmoplastic stroma. The cells were pleomorphic with high N:C, hyperchromatic nuclei, eosinophilic cytoplasm and numerous atypical mitoses [Table/Fig-1c,d]. Histological findings were favouring the FNAC diagnosis of Metastatic Adenocarcinoma. However, based on FNAC and Histopathological findings, the differential diagnoses considered were metastatic adenocarcinoma most likely Cholangiocarcinoma (CC), Colorectal adenocarcinoma (CRC), Hepatocellular Carcinoma (HCC), Primary Adenoid Cystic carcinoma of skin (ACC) and adenoid variant of basal cell carcinoma (BCC).
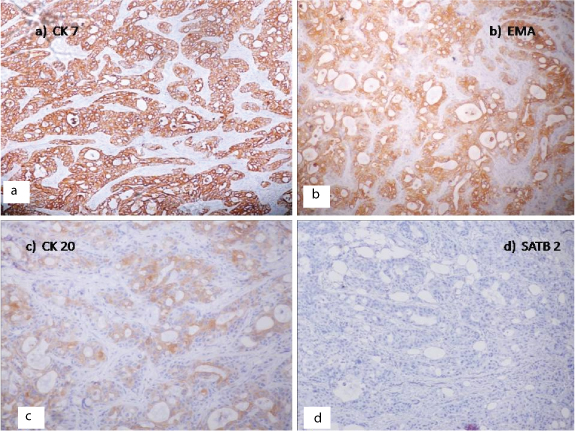
Detailed IHC panel was done to rule out other differential diagnosis as shown in [Table/Fig-2]. IHC was effectuated on 5μm thick paraffin embedded tissue sections. The antibodies in the study, their sources, clones, and dilutions are as follows. Cytokeratin AE1/AE3 (AE1/AE3; prediluted, CK7:OVTL 12/30, 1:50), CK20 (Ks 20.8; prediluted), CK 8/18 (DC10;1:25), MUC 2 (CCP58; prediluted), EMA (E29; prediluted), CEA (M7072:1:25), Hep Par-1 (OCH1E5;1:50). All above were DAKO products. SATB2 (CAB025742:1:100, Abcam). Heat Induced Epitope Antigen Retrieval (HIER) was done by heating the slides in microwave (800 watts) for 15 minutes (3 cycles × 5 minutes). The tumour cells on IHC showed diffuse positivity for Cytokeratin, AE1/AE3, EMA, CEA, CK8/18, CK 7, focal positivity for CK 20 [Table/Fig-3a-d] and negativity for MUC-2, SATB2 and 34β E12. Hence, IHC findings confirmed the diagnosis of Metastatic Cholangiocarcinoma.
Comparative Immunohistochemistry panel of present case with the differential diagnoses considered.
| AE1/AE3 | EMA | CEA | CK7 | CK 20 | CK 8/18 | 34BE12 | MUC 2 | Hep-Par-1 | SATB2 |
|---|
| HCC | S | S | + | N | N | + | N | N | + | N |
| Primary ACC | +* | + | N † | S ‡ | N | N | N | N | N | N |
| Adenoid BCC | + | N | N | S | N | N | N | N | N | N |
| CC | + | + | + | + | + | + | + | N | N | N |
| CRC | + | + | + | - | + | + | S | + | N | + |
| Present Case | + | + | + | + | + | + | N | N | | N |
*+ denotes positivity, N † denotes negative, S ‡, denotes sometimes positive Hepatocellular Carcinoma (HCC), Adenoid Cystic Carcinoma (ADC), Adenoid Variant Of Basal Cell Carcinoma (BCC), Cholangiocarcinoma (CC), Colorectal Adenocarcinoma (CRC)
Immunohistochemical staining of Tumour cells: a) CK 7 strong positivity; b) EMA positive; c) CK 20 positive; d) SATB2 negative (Immunohistochemical stain, x400).
Subsequently, further investigations were done to search for the primary lesion. An abdominal computed tomographic scan (CT scan) was done which showed mildly enlarged liver with dilatation of intrahepatic and extrahepatic bile duct without any calculus or mass lesion. A thickening was noticed in common bile duct and radiological impression was suggestive of a neoplastic stricture.
The patient was referred to a higher centre and Endoscopic Retrograde Cholangiopancreatography (ERCP) - directed brush cytology was taken which was suggestive of Adenocarcinoma. The patient was further lost to follow-up. Based on clinico-radiological and histopathological findings, a final diagnosis of cholangiocarcinoma with cutaneous metastasis to the thigh was made.
Discussion
Cutaneous metastases from internal malignancies are rare and they have been reported in only 5-10% of patients [1,2]. Only few published reports show cutaneous metastasis from (CC) to scalp, chest and back [3–6]. As per literature, most common tumours to metastasize to the skin are breast (36.2%), lung (16.3%), colorectal (11.3%), oral mucosal (7.8%), gastric (7.1%), hepatocellular (2.8%), and oesophageal (2.1%) [7,8].
The usual clinical presentation of a metastatic skin lesion is a firm, painless solitary nodule (37.7%). It can also present as macules, plaques, erythematous plaques, and ulcers [6]. Most common presentation of cutaneous metastases of CC is the nodular type as is also seen in the present case [5].
CC’s are malignant tumours arising from the intrahepatic as well as extrahepatic and hilar bile ducts. These are of three macroscopic types- nodular, periductal infiltrating or intraductal type which frequently invades adjacent organs and less commonly metastasize to visceral organs [9,10]. The most common visceral metastasis is to the lungs, bones, adrenal glands, and brain. Skin metastases is very rare, reported to occur in only 0.4 - 5.3% of cases [10].
Most of cases of cutaneous metastases of CC reported in literature describe dissemination of cancer cells due to seeding of tumour through catheter tracts used for percutaneous biliary drainage mainly to the chest (30.3%), abdomen (20.0%) [4,5,8,9]. However, cutaneous metastasis as primary presentation is extremely rare and was seen mainly to scalp, back and, in present case, to thigh [8,9].
Extensive literature search revealed ours to be the first case of cutaneous metastasis of CC presenting primarily as thigh nodule. An early diagnosis was made based on FNAC findings and confirmed by histology and IHC [Table/Fig-3]. CC usually reacts with CK7, AE1/AE3, CEA as was seen in our case. Its differentiation from HCC could be done by positive immunostaining with CK7 and CK19 for which latter is negative and negativity for Hep Par -1 which stains HCC [11,12]. As the results of CK 7/CK 20 are overlapping in CRC and CC, MUC 2, SATB2 (special AT-rich sequence-binding protein 2) was done which are found to be negative in latter. SATB2 is a specific marker of CRC and hence can prove to be a useful marker in the differential diagnosis of carcinoma of unknown primary origin [13,14]. CK 7 is more commonly positive in non-gastrointestinal carcinoma and ductal carcinoma. IHC for 34βE12 is negative in BCC and its variants which helped in ruling out a primary skin malignancy [12,13].
Skin metastasis as the first sign of CC was seen in 27% cases in a study by Liu et al., [15]. Hence suggesting that bile duct examination should be performed for cutaneous metastasis of unknown origin. The confirmation of primary malignancy is an important factor to be considered before rendering treatment. Cutaneous metastases indicates poor prognosis with Overall Survival after Cutaneous Metastasis (OSCM) of only few months. Male gender and single metastasis are associated with a relatively poorer OSCM. No potentially curative treatment yet exists except surgery. The role of adjuvant chemotherapy and radiotherapy is not well established.
Conclusion
In summary, cutaneous metastases from CC are rare, but do occur and may present anywhere in the body. An early and accurate diagnosis can be made with the help of FNAC, histopathology and IHC along with clinic-radiological findings. Clinicians should be aware of the possibility that CC may present as cutaneous metastases and henceforth manage the patient judiciously.
*+ denotes positivity, N † denotes negative, S ‡, denotes sometimes positive Hepatocellular Carcinoma (HCC), Adenoid Cystic Carcinoma (ADC), Adenoid Variant Of Basal Cell Carcinoma (BCC), Cholangiocarcinoma (CC), Colorectal Adenocarcinoma (CRC)
[1]. Schwartz RA, Cutaneous metastatic diseaseJ Am Acad Dermatol 1995 33:161-82. [Google Scholar]
[2]. Lookingbill DP, Spangler N, Sexton FM, Skin involvement as the presenting sign of internal carcinoma. A retrospective study of 7316 cancer patientsJ Am Acad Dermatol 1990 22:19-26. [Google Scholar]
[3]. Hyun SY, Lee JH, Shin HS, Lee SW, Park YN, Park JY, Cutaneous Metastasis from Cholangiocarcinoma as the First Clinical Sign: A Report of Two CasesGut Liver 2011 5:100-04. [Google Scholar]
[4]. Lu CI, Wong WR, Hong HS, Distant cutaneous metastases of cholangiocarcinoma: report of two cases of a previously unreported conditionJ Am Acad Dermatol 2004 51:108-11. [Google Scholar]
[5]. Dogan G, Karincaoglu Y, Karincaoglu M, Aydin NE, Scalp ulcer as first sign of cholangiocarcinomaAm J Clin Dermatol 2006 7:387-89. [Google Scholar]
[6]. Hussein MR, Skin metastasis: a pathologist’s perspectiveCutan Pathol 2010 37:1-20. [Google Scholar]
[7]. Hu SC, Chen GS, Lu YW, Wu CS, Lan CC, Cutaneous metastases from different internal malignancies: a clinical and prognostic appraisalJ Eur Acad Dermatol Venereol 2008 22:735-40. [Google Scholar]
[8]. Tersigni R, Rossi P, Bochicchio O, Cavallini M, Ambrogi C, Bufalini G, Tumour extension along percutaneous transhepatic biliary drainage tractsEur J Radiol 1986 6:280-82. [Google Scholar]
[9]. Lee BK, Seo YH, Lee NH, Joo SY, Ko HM, Cholangiocarcinoma with distant cutaneous metastasesKorean J Gastroenterol 2009 54:342-45. [Google Scholar]
[10]. Lookingbill DP, Spangler N, Helm KF, Cutaneous metastases in patients with metastatic carcinoma: a retrospective study of 4020 patientsJ Am Acad Dermatol 1993 29:228-36. [Google Scholar]
[11]. Kakar S, Gown AM, Goodman ZD, Ferrell LD, Best practices in diagnostic immunohistochemistry: hepatocellular carcinoma versus metastatic neoplasmArch Pathol Lab Med 2007 131:1648-54. [Google Scholar]
[12]. Duval JV, Savas L, Banner BF, Expression of cytokeratins CK 7 and 20 in carcinomas of extrahepatic biliary tract, pancreas and gall bladderArch Pathol Lab Med 2000 124:1196-200. [Google Scholar]
[13]. Magnusson K, de Wit M, Brennan DJ, Johnson LB, McGee SF, Lundberg E, SATB2 in combination with cytokeratin 20 identifies over 95% of all colorectal carcinomasAm J Surg Pathol 2011 35:937-48. [Google Scholar]
[14]. Nakagohri T, Kinoshita T, Konishi M, Takahashi S, Gotohda N, Surgical outcome and prognostic factors in intrahepatic cholangiocarcinomaWorld J Surg 2008 32:2675-80. [Google Scholar]
[15]. Liu M, Liu B-L, Liu B, Guo L, Wang Q, Song Y-Q, Dong L-H, Cutaneous metastasis of cholangiocarcinomaWorld J Gastroenterol 2015 21(10):3066-71. [Google Scholar]