Parkinson’s Disease (PD) is second most common neurodegenerative disorder affecting more than 10 million people worldwide [1]. The average life expectancy after diagnosis of PD is around 20 years and the mortality rate of Persons with PD (PWP) is two to three folds higher as compared to healthy population [2,3]. PWP experience more frequent hospital admissions and longer hospital stay due to pneumonia, urinary tract infections, hip fractures and motor decline [4]. Progressively disabling course of the disease warrants the need to include Quality of Life (QoL) measures to determine the effect of disease and its treatment on patients’ lives. Concept of QoL in PD was introduced about four decades ago when health professionals started using patient reported outcome measures as an adjunct to clinician based evaluation. Importance of patient reported outcome measure was recognized as civic bodies and insurance companies placed more weight on patient satisfaction in chronic and terminal illnesses. The effect on patients’ QoL has been suggested to be the prime criteria to develop guidelines and modify course of management [5]. Quality of life is a poorly understood concept and lacks universally accepted definition. Broadly it is considered as individuals’ perception of their position in life in the context of the culture and value systems in which they live in relation to their goals, expectations, standards and concerns (WHOQOL group 1995) [6]. Health Related Quality of Life (HRQoL) term is used to discriminate the effect of disease on patient’s QoL from overall QoL. HRQoL scales are of two types; generic scales and disease specific scales. Generic scales are aimed at general use to evaluate QoL irrespective of patients’ health and disease while disease specific scales intend to measure the impact of a particular disease on patient’s QoL.
In this article we present the development of a conceptual framework for constructing a scale for HRQoL in PD in Hindi language.
Materials and Methods
Literature review for concept, domains and items of HRQOL in PD: We did literature search on PubMed and Cochrane library from Jan 1960 to Dec 2009 with search items ‘Parkinson’s disease’ and ‘Health related quality of life’ in papers published in English language. These terms were combined with definition, domain and construct. We found generic scales, symptom specific scales and disease specific scales for PD but we focused only on disease specific scales for PD that had been used for evaluating HRQoL in PD. We reviewed two books on QoL [19,20], related articles from bibliography of resources and five websites dedicated to HRQoL (www.isoqol.org, www.proqolid.org, sites/utotonto.ca/qol, http://qol.thoracic.org and www.headandneckcancer.co.uk/For+professionals/Quality+of+Life+(qol).aspx) to understand the concept of HRQoL and identification of related domains which contribute to QoL in PD.
Interview of stakeholders: A total of 28 consecutive Hindi speaking persons with idiopathic PD irrespective of their age, gender, socio-economic status, years of education, occupation, clinical severity, place of residence and age of onset of symptoms referred for physiotherapy from movement disorder clinic of a tertiary care teaching hospital in India, were recruited from Feb 2010 to Oct 2010 after diagnosis of PD was confirmed by a movement disorder specialists (MB) on the basis of UK PD brain bank diagnostic criteria [21]. Persons with cognitive impairment (Mini Mental State Examination<24) [22] or suffering from other associated disabling neurological, musculoskeletal diseases were excluded to avoid confounding effect of other illness.
After obtaining informed consent and approval of the project by IRS/EC of the institute, recruited PWP were invited for semi-structured interview, using open ended questions to gauge what they understood by the term QoL, how PD affected their life and how their life had changed from pre-disease status. Following the interview with open-ended questions, same PWP were asked to comment on predefined domains of QoL as suggested by review of literature, i.e., physical activities, mood, social and family, finance related issues and non- motor features of PD. PWP were asked: “Are these domains important to you?” or “Are they relevant for you?” or “If they affect your lives?” The interviews were modified according to person’s knowledge/educational level and understanding of the concept.
Six caregivers of PWP, who were directly involved in care of PD persons were interviewed regarding domains and items identifications for appraisal of HRQoL. Nine specialists including eight movement disorder specialists (MB, SS, VG, GS, MG, CSA, KSA, SSR) and one psychiatrist (NK) were invited to comment on the concept, domains and other factors associated with HRQoL in PD.
Total duration of interview ranged from 15 minutes to 45 minutes. Interviews were conducted in Hindi language. Interviews of PWP, caregivers and specialists were audio recorded with due permission and consent. Single researcher (RA) conducted all interviews.
Domains of QoL in PD: On the basis of review of literature, PD specific QoL scales and content analysis of interviews; opinion of a panel consisting of people/ experts involved in care of PWP, four neurologists, one physiotherapist, one psychiatrist and one biostatistician extracted domains of QoL for PWP, which were tabulated to get consensus of stakeholders. Seven specialists, seven PWP (different from those who were interviewed earlier) and seven caregivers were asked to grade domains on the basis of their relevance on a 7-point scale [Very much relevant (1) to not relevant (7)]. We determined consensus by Median scores and Inter Quartile Deviations (IQDs). An IQD <1 was considered as good consensus on a 7–point Likert scale. We classified three outcomes: (a) Consensus and agreement that a domain is highly important (IQD < 1 and Median > 6); (b) Consensus that a domain is less or moderately important (IQD < 1 and Median < 5); (c) No consensus (IQD > 1) [23].
Conceptual framework and definition: After consensus for domains, the panel developed a conceptual framework to construct HRQoL scale for PWP based on principles laid down by Fayers and Machin [19] and Rothman et al., [17] on development of patients’ reported outcome measures. These principles are:
QoL scales should have both indicator domains and causal domains.
There should be a ‘priori’ model of postulated domains. The psychometric principles used to create various domains are not suitable for causal items.
The scale should include global question on QoL.
Finally, panel converged on a definition for HRQoL in PD by consensus, taking in account health and QoL definitions by WHO and conceptual framework of HRQoL in PD.
Results
Eight disease specific scales for PD were reviewed for finding domains of HRQoL [Table/Fig-1]. All scales have different domains but broadly these domains focus mainly on four domains. These domains are physical, psychological, family/social and Non Motor Symptoms (NMS) of PD. Both Parkinson’s Impact Scale (PIMS) [11] and Parkinson’s Disease Quality of Life Scale (PDQUALIF) [14] have single item on financial strain.
The key points regarding HRQoL from literature review are:
QoL should be reported by patient.
QoL in PD is a multidimensional concept so it can’t be measured directly by single domain.
QoL is influenced by causal domains. Causal domains are cluster of symptoms and other variables like complications of therapy, age, educational status etc.
QoL can be estimated by indictor domains like physical abilities, mood, social relationship, satisfaction with health and treatment etc.
Non-modifiable factors for QoL are: Age, gender and education level.
QoL is an individualized concept and not a pre-defined criterion.
QoL is a dynamic trait.
QoL is influenced by expectations and experiences.
QoL depends on the needs of a person in life.
Twenty eight PWP (mean ± SD age 54.2 ± 9.17 years, M:F :: 2.5:1) participated in semi-structured interviews. There was predominance of patients in moderate to severe disease (median Hoehn & Yahr stage of 3) and middle socioeconomic status [Table/Fig-2]. Six caregivers were interviewed (5 spouses and 1 son of the patients). Nine specialists had mean clinical experience of 19.2 (range 8-32) years for treating PD.
Characteristics of persons with PD interviewed for item pool generation (n=28) data has been presented as Mean ± SD (range) or n (%).
| Age (yrs.) | 54.2 ± 9.17 (40-74) |
| Gender (M:F) | 20:8 (71:29) |
| Duration of symptoms (yrs.) | 6.3 ± 3.4 (1-15) |
| Family Joint: Nuclear | 14:14 |
| H & Y stage |
| 1 | 1 (3.5) |
| 1.5 | 1 (3.5) |
| 2.5 | 7 (25) |
| 3 | 15 (54) |
| 4 | 4 (14) |
| Socio-economic status (Kuppuswamy scale) |
| Upper | 3 (11) |
| Upper middle | 10 (36) |
| Lower middle | 8 (28) |
| Upper lower | 6 (21) |
| Lower | 1 (4) |
| Qualifications |
| Higher education/Professional degree | 11 (40) |
| Bachelor degree | 6 (21) |
| Matriculate/Inter | 9 (32) |
| Below matriculate or uneducated | 2 (7) |
| Occupational status |
| Retired | 5 (18) |
| Left/modified job due to disease | 6 (21) |
| Working | 13 (47) |
| Housewives | 4 (14) |
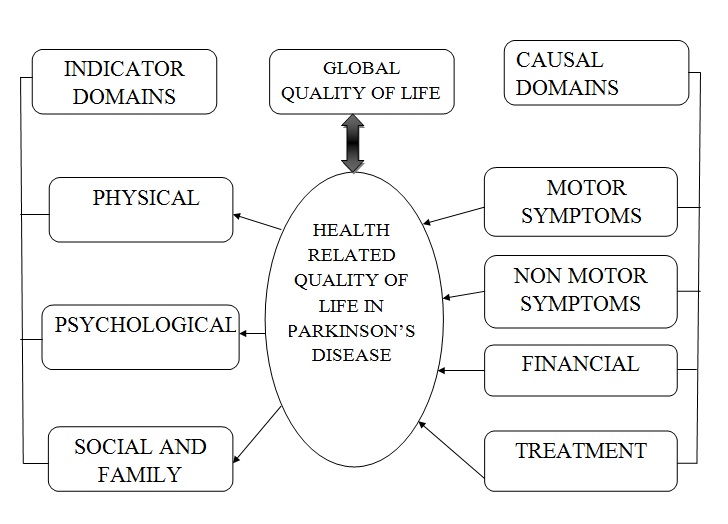
The content analysis of interviews revealed items related to financial hardship and efficacy of treatment were important component for QoL in PD in addition to physical, psychological, family/social and NMS domains [Table/Fig-3]. The grading of six domains by stakeholders is shown in [Table/Fig-4]. Patients, caregivers and clinicians combined had consensus (IQD <1; Median > 6) on relevance of proposed six domains. However, when individual groups were analyzed, clinicians didn’t have consensus for psychological, social, treatment and NMS domains (IQD>1), whereas all others had perfect consensus. The conceptual framework for HRQoL scale for PD [Table/Fig-5] consists of causal domains and indicator domains. Physical domain was considered in causal domain (motor domain) as well as indicator domain (physical abilities). Motor, NMS, treatment and finance are causal domains while physical abilities, social/family and psychological are indicator domains. Causal domains influence HRQoL of a PWP while indicator domains estimate it. Global QoL was postulated equivalent to HRQoL in PD.
Domains of health related quality of life in Parkinson’s disease.
| Domain | Description |
|---|
| Physical | Abilities to do activities of daily living, mobility, motor symptoms (slowness, tremors, stiffness), independence. |
| Psychological | Mood disorders, anxiety, depression, lack of concentration and fear. |
| Social and Family | Ability to take social and family responsibilities, social participation, role functioning. |
| Non motor symptoms | All symptoms other than motor symptoms like constipation, fatigue, urinary problem, hallucination, pain, sexuality, sensory symptoms, memory disturbance, loss of appetite, cognition, sleep disorders etc. |
| Treatment | Efficacy of treatment, satisfaction with treatment and complications of treatment. |
| Financial | Effect on family income by disease, expenditure on treatment and disturbance of family due to financial issues, need to decline more paying/challenging jobs or retiring prematurely. |
Grading of domains by stakeholders on a 7-point Likert scal.
| Physical | Psychological | Social and Family | Treatment | Finance | NMS |
|---|
| Median (Range) |
| Patients (n=7) | 7 (6-7) | 7 (7-7) | 7 (7-7) | 7 (7-7) | 7 (6-7) | 7 (7-7) |
| Caregivers (n=7) | 7 (6-7) | 7 (6-7) | 7 (5-7) | 7 (7-7) | 7 (5-7) | 7 (6-7) |
| Clinicians (n=7) | 7 (7-7) | 7 (4-7) | 7 (4-7) | 7 (4-7) | 7 (4-7) | 7 (3-7) |
| Combined (n=21) | 7 (6-7) | 7 (4-7) | 7 (4-7) | 7 (4-7) | 7 (4-7) | 7 (3-7) |
| IQD |
| Patients (n=7) | 0 | 0 | 0 | 0 | 0 | 0 |
| Caregivers (n=7) | 0 | 0 | 1 | 0 | 0 | 0 |
| Clinicians (n=7) | 0 | 2 | 2 | 2 | 1 | 2 |
| Combined (n=21) | 0 | 0.5 | 1 | 0 | 0.5 | 0.5 |
IQD: Inter quartile deviation; NMS: Non-motor symptoms domain.
Conceptual framework of Health related quality of life in Parkinson’s disease patients.
Causal domains consist of causal items that influence HRQoL while indicator domains contain indicator items which estimate the HRQoL. The amalgamation of causal domains and indicator domains constitute HRQoL. Subjective QoL perception (Global QoL) is postulated as equivalent to HRQoL estimated by multiple domains.
The consensus definition given by the panel was “Health related quality of life in Parkinson’s disease is defined as multidimensional concept consisting of patients’ self evaluation of the impact of motor and NMS, effect of treatment, psychological state, spirituality, social and financial implication and overall health satisfaction”.
Discussion
Quality of life is a latent multi-factorial concept which can’t be measured directly. As there is no consensus on definition and what constitutes HRQoL in PD [16], researchers [17,19] have suggested to define and conceptualize QoL before development of any new instrument. There is general agreement that HRQoL assess the physical, social and emotional well being and health satisfaction combining objective functioning and subjective perceptions and judgments [24].
The diagnosis of PD in a person, affects his/her life along with the life of their caregivers in multiple ways. Availability of good health resources, compensation for financial strains and psychosocial support are crucial factors that influence a patient’s QoL apart from maintaining pre disease state of independence and autonomy. In a rapidly advancing medical system, new drugs and treatment options are introduced into health sector regularly for PD management [25,26]. It can be argued that drugs with similar clinical benefits, with better effect on QoL should be recommended. At the same time, small treatment benefits may be more than outweighed by the cost of therapy and poorer QoL if new drug is expensive and/or associated with significant side effects. In extreme cases, cure might be worse than disease [19]. The efficacy and complications of treatment carry a great implication on patients’ lives [25,27].
Available scales to assess QoL of PWP, do not address implication of complications related to therapeutic interventions and financial strain. It may be attributed to lack of conceptual framework and/or definition of HRQoL in PD. In last two decades there is deluge of studies to assess QoL in PWP. Age at onset, gender, education level, physical abilities, motor symptoms, depression, anxiety, family, socialization, communication, NMS, financial status, treatment efficacy and complications of therapy have been postulated to be the predictors of QoL in PD [27–33]. [Table/Fig-5] shows the conceptual framework that recognizes the essential domains of HRQoL for PD persons. To create various domains; literature was reviewed, and patients, care givers and clinicians were interviewed. The conceptual framework of HRQoL in PD consisted of two important factors: 1) Causal domains and 2) Indicator domains. Causal domains are constellation of items on various motor and NMS, efficacy and satisfaction with treatment and financial implication, and may influence the QoL in both positive as well as negative ways. Items are grouped in causal domains on the basis of their frequency and severity as perceived by the patient (clinimetric principles) [34,35]. Items in causal domains are independent of each other and have differential effect on QoL depending on patient’s perception. On the other hand, indicator domains consist of items on physical abilities, family and social relationship, and psychological domains. Hence, items in indicator domain are highly correlated to each other and theoretically measure single aspect of QoL. Collectively indicator domains measure the latent trait of QoL. Items in indicator domains are grouped on the basis of their correlation to each other using factor analysis. Indicator domains are constructed using psychometric principles, i.e., item to item correlation in a scale (internal consistency), high correlation of an item to its scale (convergent validity) and lower correlation of an item to other scales (divergent validity). Although indicator domains estimate the QoL of a patient but these domains are poorly sensitive to change, due to lack of any disease specific item. Therefore, many researchers have suggested to include both causal as well as indicator domains in disease specific HRQoL instrument for improving its sensitivity, discriminatory properties and responsiveness [17,19,36]. The present conceptual framework proposes the interrelationship of causal and indicator domains with HRQoL in PD.
Global QoL is a single item concept where patients evaluate his/her overall QoL rather than individual domains. Gill & Feinstein [37] and Fayer & Machin [19] have suggested to include global QoL in every patient reported outcome measure on QoL. Global QoL is a reliable estimate of patients’ actual QoL and has been used by many popular QoL scales like Euro-QoL, EORTC QLQ-C30 etc. Spector (1992) [38] has criticized the use of single item scale due to its poor reliability where as other investigators have emphasized its inclusion for robustness and holistic nature [37,39]. As patient is final arbitrator of his/her QoL, the estimated score from multi item QoL questionnaire should correlate strongly with Global QoL. Hence, in conceptual framework we postulated the equivalence of Global QoL with overall QoL estimated through various domains.
We focused on six broad domains covering all essential components of HRQoL for people with PD after obtaining consensus of stakeholders, as it was difficult to include all domains of currently available scales due to heterogeneity in their content and nomenclature. Consensus on six domains was reached strongly by PWP and caregivers groups but clinicians did not agree for psychological, social and family, treatment and NMS domains. We didn’t embark on second round for consensus of clinicians for QoL domains for two reasons. First, combined stakeholders had consensus for all six domains; secondly we gave more emphasis on grading by patients as they are final perpetrator to evaluate their QoL, and did not consider any domain for removal. The definition of HRQoL in PD emphasized perception of patients’ due to various symptoms of the disease and their impact on their lives. Stakeholders did not put emphasis on spirituality component during interviews; still it was added in the definition adopting WHO model of health.
To our knowledge this is first time an attempt was made to develop a conceptual framework and define HRQoL for PWP. This framework incorporates financial and treatment domains which were not addressed to in earlier scales.
Conclusion
To conclude, this study has defined conceptual framework for HRQoL scale in PWP based on literature review, interview and consensus of experts as to what constitutes QoL. This framework addresses causative factors, indicator factors and self reporting of QoL including concept of global QoL. Motor symptoms, NMS, financial implications and efficacy of treatment are essential causal domains where as physical aspects, psychological aspects, family and social aspects are essential indicator domains to evaluate HRQoL in people with Parkinson’s disease.
BELA-p-k: Belastungsfragebogen Parkinson kurzversion; PDQ-39: 39 item Parkinson’s disease questionnaire; PDQ-8: Short form Parkinson’s disease questionnaire; PDQL: Parkinson’s disease quality of life questionnaire; PIMS: Parkinson’s impact scale; PLQ: Fragebogen Parkinson Lebens Qualität; SCOPA-PS: Scales for Outcomes in Parkinson’s disease – Psychosocial; PDQUALIF: Parkinson’s disease quality of life scale.
* PDQ-8 is a short form of PDQ-39 ADL= Activities of Daily Living
IQD: Inter quartile deviation; NMS: Non-motor symptoms domain.