Mucocele like Tumour of the Breast Associated with Ductal Carcinoma in situ and Focal Ductal Carcinoma: What is the Best Approach to these Patients?
Serdar Altinay1, Safak Ersöz2, Yavuz Üye3, Feyyaz Özdemir4
1 Medical Faculty, Department of Pathology, Selcuk University, Konya, Turkey.
2 Medical Faculty, Department of Pathology, Karadeniz Tecnic University, Trabzon, Turkey.
3 Department of General Surgery, Giresun Kent Hospital, Giresun, Turkey.
4 Medical Faculty, Department of Oncology, Karadeniz Tecnic University, Trabzon, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Serdar Altınay, Selcuk University, Selçuklu Tıp Fakültesi, Tıbbi Patoloji Anabilim Dalı, Akademi Mah. Yeni İstanbul Cad. No:313 Selçuk Üniversitesi Alaeddin Keykubad Yerleşkesi 42130 Selçuklu/KONYA.
E-mail: drserdara@yahoo.com
Mucocele Like Tumours (MLT) of the breast are quite rare neoplasms displaying a broad spectrum. These lesions were considered benign initially. But now, they are believed to be related to atypical ductal hyperplasia, ductal carcinoma, or mucinous carcinoma. Preoperative diagnosis in fine needle aspiration and core biopsy is difficult. We are reporting a case of mucocele like tumour with ductal carcinoma in situ and ductal carcinoma in a 71-year-old Turkish woman. The patient had a palpable mass in her left breast. Mammograpy showed ill defined and lobulated mass with widespread tiny microcalcifications. A few cells with sporadic nuclear atypia, were detected on FNAB (Fine Needle Aspiration Biopsy). Mastectomy was done on the left side because of the suspicion of malignancy as evident by mammograpy and FNAB. We examined adequate tissue samples from resection material. Histopathologic findings were consistent with MLT and microscopic focus of ductal carcinoma was also noted in mastectomy specimen. She is currently disease-free in the 118th month. We believe that our case will be the first patient from Turkey and will be added to the database as one of the longest term follow-up MLT cases reported. If a mucocele-like tumour is suspected in fine needle biopsy, surgical excision should be recommended and the specimen should be carefully evaluated to exclude the presence of ductal carcinoma in situ or carcinoma.
Breast surgery, Cytology, DCIS
Case Report
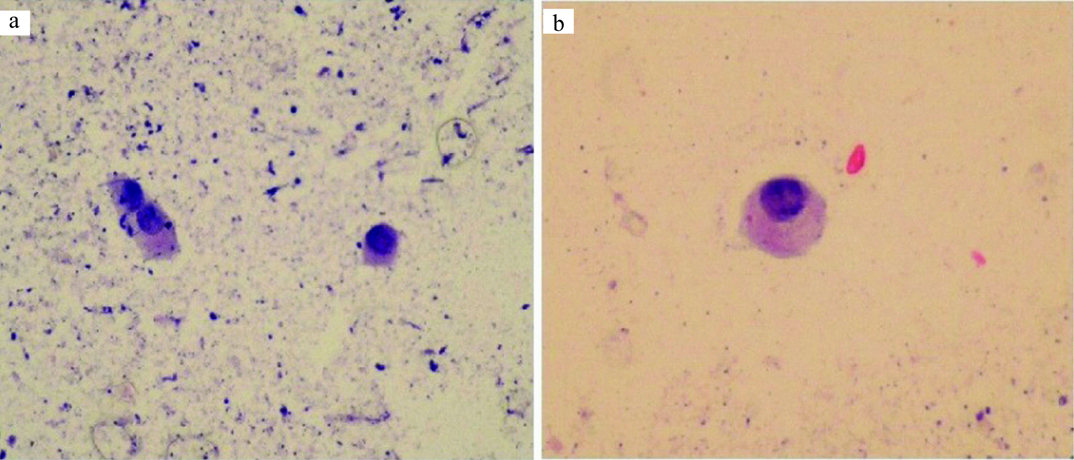
A 71-year-old female patient was admitted to the surgery clinic with the complaint of a palpable mass without pain in the left breast. There was no family history for breast cancer. She had not undergone an operation for breast previously. There was no nipple discharge. Mammography showed a hypodense nodule comprising of slightly irregular, confined, coarse and granular calcification with a diameter of 5x4 cm [Table/Fig-1]. It was reported as diffuse linear calcifications around the nodule. A dark green coloured mucoid-like material with a volume of 0.2 cc, which could hardly be pushed back from the injector, was obtained in the FNAB. A few cells with sporadic nuclear atypia, giving the impression that a cyst wall was laid on the hypocellular background were noted in the microscopic assessment [Table/Fig-2]. Mastectomy was done on the left side due to the suspicion of malignancy as evident by mammography and FNAB. The gross specimen showed a thick-walled cystic structure (diameter aproximately 5x5 cm) containing dark green coloured mucoid material in the internal central quadrant on the surface [Table/Fig-3]. Similar cysts were also present in the other quadrants.
Mammography showing nodular ill defined mass and diffuse linear calcification around the nodule.
a: Photomicrograph exhibiting atypical cells with large and prominent nucleolus in mucoid background. (MGG; x200). b: Photomicrograph showing peripheral localization of nucleus and a prominent nucleolus in high power (MGG; x400).
A thick- walled cystic structure with a diamater of approximately 5x5 cm was noted (arrows) on the surface of the mastectomy specimen.

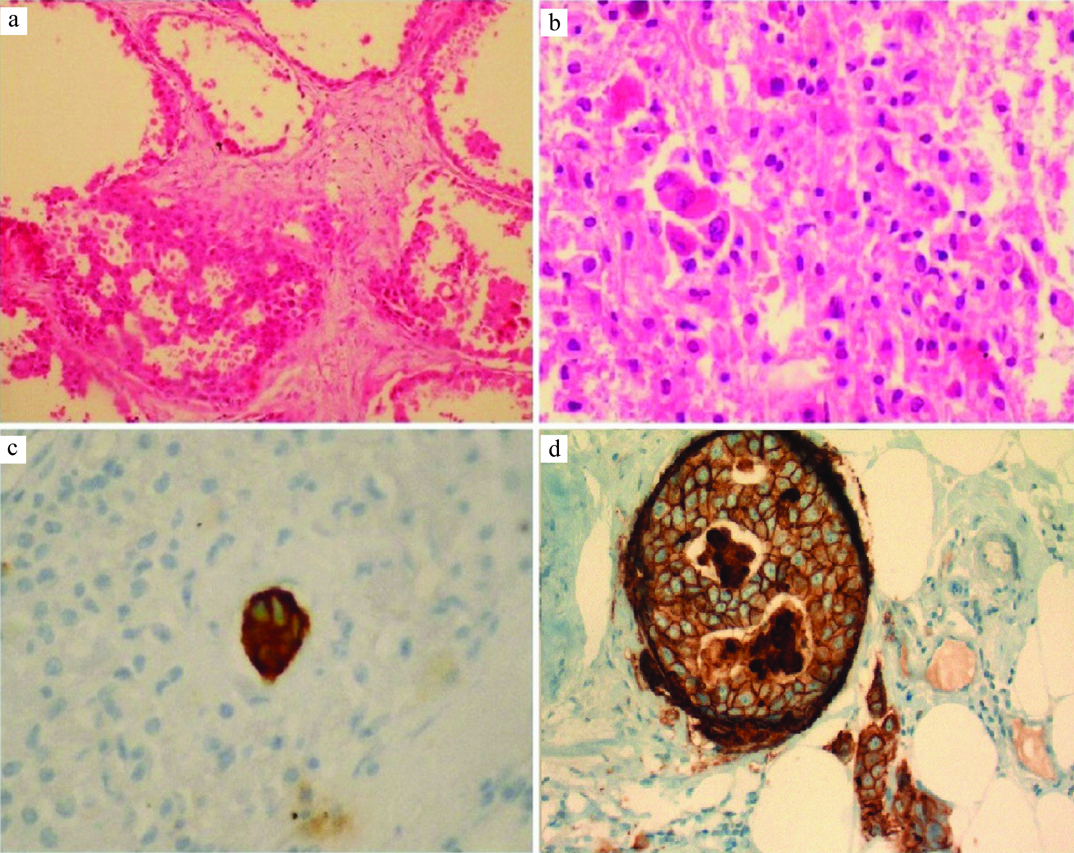
The histopathological assessment showed cystic ducts surrounded with hyalinized fibrous tissue in samples from all quadrant. The cystic epithelial lining exhibited changes in one or a few layers. Sporadic hyperplasia, with large pleomorphic and hyperchromatic nucleus and wide eosinophilic cytoplasm, ranging from atypical ductal hyperplasia to in situ were identified. Right adjacent to these, a stand-alone microscopic carcinoma focus which stained with pancytokeratin (+) was observed, while the estrogen and progesteron receptors was (-) in the immunohistochemical staining, c-erbB2 (+) displayed reactivity [Table/Fig-4]. No metastasis was observed in the axillary lymph nodes. The patient is in the 118th month of follow-up and is disease-free and healthy.
a: Focus of ductal hyperplasia and ductal carcinoma in situ were identified (H&E; x200). b: Single atypical cells in necrotic area (H&E; x200). c: Tumour cells were positive for cytokeratin (x200). d: Membranous c-erbB-2 positivity were detected in atypical cells. Ductal carcinoma in situ in the upper left, carcinoma cells in the bottom right (x400).
Discussion
Mucocele-Like Tumour (MLT) of the breast may display various histological spectrums. These range from benign tumours to Atypical Ductal Hyperplasia (ADH), Ductal Carcinoma in situ (DCIS) and even mucinous carcinoma. There was no association with malignancies in the cases reported by Rosen [1] who was the first person to define it in 1986. Ro et al., presented seven cases comprising of atypical ductal hyperplasia or microscopic mucinous carcinoma [2]. Most recent reports draw attention mainly to the coupling of ductal carcinoma in situ and invasive carcinoma and indicate that mucinous carcinoma may be a precursor early lesion [2,3]. Therefore, it is extremely important to exclude the presence of carcinoma with sufficient samples in the presence of MLT in breast biopsy. We sampled a lot of tissue blocks and observed areas of ADH, low-degree DCIS and focal invasive carcinoma in our case.
The question now arises that is it possible to make a correct diagnosis with fine needle aspiration on patients which are presenting with a cystic mass in the breast? Sohn et al., evaluated the differential diagnostic findings between MLT and mucinous carcinoma [4]. They reported that cytologically, mucinous carcinomas are more cellular and epithelial cellular layers do not contain any myoepithelial cells. These cells with marked prominent nucleolus may look like atypical cells in the epithelial layers. Such cytological characteristics should be taken into account when making a specific diagnosis. However, MLT cases erroneously diagnosed with mucinous carcinoma with FNAB were also reported in literature [5]. In our case, aspiration was obtained only from the cystic area containing dark coloured mucoid fluid with a few atypical cells. This indicated that it could be associated with malignancy and refrained us from making a diagnosis of mucinous carcinoma.
But, is core biopsy an appropriate option in MLTs? The pathologist can make a diagnosis if he sees atypical cells inside the mucin. However, making a diagnosis becomes challenging because MLTs often contain minimal epithelial components. As MLTs display a wide spectrum ranging from benign to mucinous carcinoma, there is a significant risk of under-diagnosis especially in small biopsies [6]. Therefore, surgical excision is recommended. On the other hand, Rakha et al., reviewed the course of pure mucocele-like lesions (not containing atypia) diagnosed with core biopsy in literature and published that DCIS was identified in two of the 54 patients (4%) in the excision material [7]. They stated that in case of presence of atypia in core biopsy in the previous studies [8,9], the frequency of malignancies were higher (21%, 7/33). We could not apply Tru-Cut biopsy on our 71-year-old case because of lack of facilities. However, mammography was done and it showed diffuse linear micro-calcifications on a wide area of breast. We performed mastectomy due to suspicion of malignancy both in Ultrasound Sonography (USG) and FNAB. Authors have reported that mastectomy was done on two patients in a long-term follow-up study comprising 15 patients. Their ages ranged between 38-56 years (24-99 months, average 63.8 months). They found that one lesion (ADH) in core biopsy relapsed accompanied with DCIS at 37 months after excision, while no relapse or lymph node/distant metastasis was detected in the other patients [10]. Hamela-Bena et al., studied 53 lesions from 49 patients, in whom 25 MLT were benign and 28 were malignant (14 in situ, 14 invasive) [11]. They reported that two patients had recurrences in the breast (one benign MLT and one MLT with carcinoma).
Thus, MLTs with indeterminate aetiopathogenesis may receive different histopathological diagnoses ranging from benign proliferative pathologies, like in our case, to malignancies and present a relapse risk although at a low number.
MLTs have non-specific mammographic findings and the sonographic findings are similar to those of low internal echolar and multiple, well-marginated, hypoechoic oval/tubular structures and complex cysts [12]. Fine-needle aspiration may show mucinous material that may not be specific, unless a large number of cells is present. In the presence of mucinous material with only a few cells, it is impossible to differentiate a Mucocele-like lesions (MLL) from a mucinous carcinoma, and a surgery must be performed to confirm the diagnosis. Recently authors pointed out that surgery is clearly warranted for MLT associated with atypia seen in core needle biopsy because it may be upgraded to malignancy upon excision. Authors observed an upgrade to DCIS slightly superior to 5%. Upgrading at surgery is a phenomenon that was also observed in patients with ADH and DCIS. Hence, if atypia is seen in core biopsy, surgical excision is required for more advanced evaluation. And if the surgical excision also suggests the same, mastectomy may be required in some cases [13,14]
Conclusion
Attention should be given both to the cytological assessment and core biopsy in MLTs. If a mucocele-like tumour is suspected in fine needle biopsy, surgical excision should be recommended and the specimen should be carefully evaluated to exclude the presence of DCIS or carcinoma. Based on our current knowledge, radiology, breast surgery and the multidisciplinary approach of pathologists, excision and clinical follow-up appear to be the best option for MLTs.
[1]. Rosen PP, Mucocele-like tumours of the breastAm J Surg Pathol 1986 10:464-69. [Google Scholar]
[2]. Ro JY, Sneige N, Sahin AA, Mucocelelike tumour of the breast associated with atypical ductal hyperplasia or mucinous carcinoma. A clinicopathologic study of seven casesArch Pathol Lab Med 1991 115:137-40. [Google Scholar]
[3]. Yeoh GP, Cheung PS, Chan KW, Fine-needle aspiration cytology of mucocele-like tumours of the breastAm J Surg Pathol 1999 23:552-59. [Google Scholar]
[4]. Sohn JH, Kim LS, Chae SW, Fine needle aspiration cytologic findings of breast mucinous neoplasms: differential diagnosis between mucocelelike tumour and mucinous carcinomaActa Cytol 2001 45:723-29. [Google Scholar]
[5]. Kikuchi S, Nishimura R, Osako T, Mucocele-like tumour associated with ductal carcinoma in situ diagnosed as mucinous carcinoma by fine-needle aspiration cytology: report of a caseSurg Today 2012 42:280-84. [Google Scholar]
[6]. Bilous M, Breast core needle biopsy: issues and controversiesMod Pathol 2010 23:36-45. [Google Scholar]
[7]. Rakha EA, Shaaban AM, Haider SA, Outcome of pure mucocele-like lesions diagnosed on breast core biopsyHistopathology 2013 62:894-98. [Google Scholar]
[8]. Carder PJ, Murphy CE, Liston JC, Surgical excision is warranted following a core biopsy diagnosis of mucocoele-like lesion of the breastHistopathology 2004 45:148-54. [Google Scholar]
[9]. Ouldamer L, Body G, Arbion F, Avigdor S, Michenet P, Mucocele-like lesions of the breast: management after diagnosis on ultrasound guided core biopsy or stereotactic vacuum-assisted biopsyGynecol. Obstet. Fertil 2010 38:455-59. [Google Scholar]
[10]. Ohi Y, Umekita Y, Rai Y, Mucocele-like lesions of the breast: a long-term follow-up studyDiagn Pathol 2011 6:29 [Google Scholar]
[11]. Hamele-Bena D, Cranor ML, Rosen PP, Mammary mucocele-like lesions. Benign and malignantAm J Surg Pathol 1996 20:1081-85. [Google Scholar]
[12]. Leibman AJ, Staeger CN, Charney DA, Mucocele like lesions of the breast: mammographic findings with pathologic correlationAJR Am J Roentgenol 2006 186:1356-60. [Google Scholar]
[13]. Ha D, Dialani V, Mehta TS, Keefe W, Iuanow E, Slanetz PJ, Mucocele-like lesions in the breast diagnosed with percutaneous biopsy: is surgical excision necessary?AJR Am J Roentgenol 2015 204:204-10. [Google Scholar]
[14]. Diorio C, Provencher L, Morin J, Is there an upgrading to malignancy at surgery of mucocele-like lesions diagnosed on percutaneous breast biopsy?Breast J 2016 22:17 [Google Scholar]