Clinicopathological Characteristics of Thymic Tuberculosis- A Rare Entity
Keerthi Ramachandran Pillai1, Meenu Prakash2, Muktha Ramesh Pai3
1 Postgraduate Student, Department of Pathology, AJ Institute of Medical Sciences, Mangalore, Karnataka, India.
2 Postgraduate Student, Department of Pathology, AJ Institute of Medical Sciences, Mangalore, Karnataka, India.
3 Professor, Department of Pathology, AJ Institute of Medical Sciences, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Keerthi R. Pillai, 610, Residents Hostel, AJ Institute of Medical Sciences, Kuntikana, Mangalore, Karnataka-575001, India.
E-mail: pillai.keerthi88@gmail.com
Tuberculosis is a severely debilitating disease and it rarely presents with involvement of the thymus. Only fifteen cases have been reported worldwide. We report a case of thymic tuberculosis in a 12-year-old female presenting with cervical lymphadenopathy. Computed tomographic imaging revealed a mediastinal mass which was then excised via thoracotomy. The gross appearance of the cut surface of both lobes was variegated with white, granular caseating material. Microscopy revealed multiple, caseating, epithelioid granulomas with dispersed Langhans giant cells surrounded by thymic parenchyma with Hassals corpuscles. The patient was treated with anti-tubercular drugs and her condition improved. On follow up, the patient is healthy and has gained weight.
Caseation, Granuloma, Thymus
Case Report
A 12-year-old female presented to the pediatric outpatient department with a swelling in the right side of the neck since one month associated with cough, weight loss and lethargy. On examination, the right cervical lymph nodes were matted and enlarged, measuring 4x3x1cm. Chest X-ray was normal and sputum was negative for Acid Fast Bacilli (AFB). Peripheral smear examination showed microcytic hypochromic anaemia. Serological and biochemical tests were normal. Ultrasound imaging of the swelling showed heteroechoic lymph nodes in the right supraclavicular region (35 X 24mm). Fine needle aspiration of the right cervical lymph nodes showed cohesive clusters and singly scattered epithelioid histiocytes surrounded by small mature lymphocytes and neutrophils with granular caseous material in the background. A diagnosis of tuberculous lymphadenitis was made and anti-tubercular therapy (Category 1; Revised National TB Control Program) was started.
After five months of therapy, she developed breathlessness and mild intermittent fever without chills and rigors. The neck swelling had decreased in size. Examination of the respiratory system revealed increased vocal resonance in the right suprascapular area and monophonic wheeze along with coarse biphasic crepitations in the right infraclavicular area.
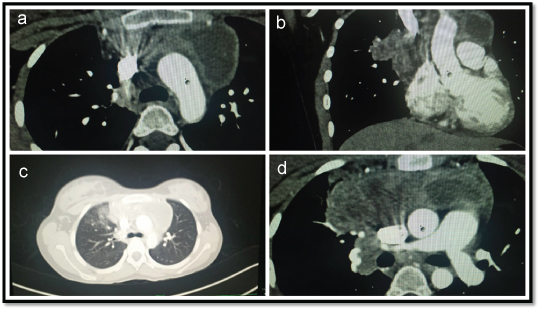
Chest X-ray showed an anterior mediastinal mass while the lung fields were normal. Therefore, the crepitations and wheeze were attributed to possible bronchial obstruction due to the mediastinal mass. The subsequent contrast enhanced computed tomography revealed focal atelectasis with associated fibrotic changes of the right upper lobe and multiple rim enhancing mediastinal lymph nodes [Table/Fig-1]. Ultrasound-guided fine needle aspiration of the mediastinal mass showed caseating epithelioid granulomas suggestive of tuberculosis. The probability of drug resistant tuberculosis was considered based on clinical and radiological assessment. The patient underwent thoracotomy. Intraoperatively, the mass was identified as the thymus and excision was done.
a) Axial section of CT chest showing an ill-defined hypodense peripherally enhancing lesion with smooth margin; b) Coronal section of CT showing ill-defined hypodense peripherally enhancing lesion in bilateral peri-hilar region; c) Sagittal sections showing similar findings as (b); d) Ill-defined peripherally enhancing lesion with central non-enhancing areas.
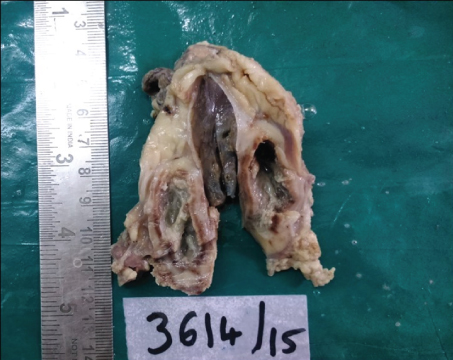
Macroscopically, the right lobe of thymus and the cystic left lobe of thymus measured 6.5x6.5x3cm and 9x3.5x1.5 cm respectively. The cut surface of both lobes showed a variegated appearance with hemorrhagic grey-white caseating areas rimmed by a fibrous capsule [Table/Fig-2]. The cyst in the left lobe was also filled with whitish granular caseating material.
Gross specimen of left lobe of thymus showing a cyst filled with whitish granular material.
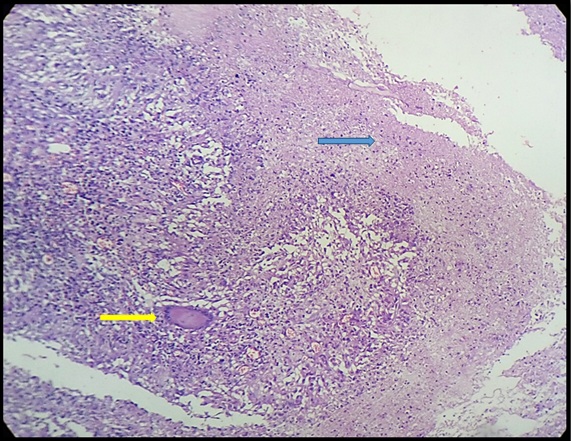
Microscopically, the thymic tissue was studded with numerous large, confluent, caseating and non caseating epithelioid granulomas with dispersed Langhans giant cells [Table/Fig-3]. There were foci of dystrophic calcification, haemorrhage surrounded by reactive lymphoid tissue and thymic parenchyma with Hassalls corpuscles. Acid fast bacilli were seen on Ziehl Neelsen staining.
Photomicrograph showing thymic tissue with epithelioid granulomas with Langhans giant cells (yellow arrow) and caseation necrosis (blue arrow) (H&E,10X).
Category 2 anti-tubercular therapy was started post-operatively since she had received category 1 previously for the cervical lymphadenopathy. The fever subsided after 15 days of therapy. On follow up after 2 months, there was no history of recurrence of fever, no mediastinal widening, and the patient was tolerating anti-tubercular therapy.
Discussion
Tuberculosis continues to intimidate humanity as a severely debilitating disease. The involvement of the mediastinum by tuberculosis is very rare [1]. There have been very few case reports of mediastinal tuberculosis in literature. Tuberculosis rarely features in the list of thymic masses. Only fifteen cases of thymic tuberculosis have been reported in literature in the past seven decades, worldwide [1–14].
Even though the incidence of tuberculosis has increased with the increased prevalence of acquired immunodeficiency syndrome, the diagnosis of tuberculosis of the thymus is extremely rare [1]. Almost all of these cases were diagnosed in adults and adolescents with one case each involving a child and a six-month-old infant [8,13]. It has been suggested that thymic tuberculosis in infants and children was most likely primary tuberculosis unlike adults where it represents remnants of post primary localized mediastinal tuberculosis [4,14]. Salient characteristics of the 15 published cases are included in [Table/Fig-4].
Characteristics of the 15 reported cases.
| Characteristics | Number | Percentage |
|---|
| 1. Age Group (N=15) |
| Infant (<1year) | 1 | 6.7 |
| Childhood (1-15years) | 1 | 6.7 |
| Adolescent (15-18 years) | 3 | 20.0 |
| Early Adulthood (19-30 years) | 6 | 40.0 |
| Late Adulthood (>30years) | 4 | 26.7 |
| 2. Gender (N=15) |
| Male | 9 | 60.0 |
| Female | 6 | 40.0 |
| 3. Presentation (N=13) |
| Dyspnoea | 6 | 46.0 |
| Cough | 5 | 38.5 |
| Chest Pain | 4 | 30.8 |
| Wheezing | 2 | 15.4 |
| Weight Loss/ Failure to thrive | 2 | 15.4 |
| Asymptomatic | 3 | 23.1 |
| 4. Location of Lesion (CT; N=10) |
| Anterior mediastinum | 9 | 90.0 |
| Middle mediastinum | 1 | 10.0 |
| 5. Thymic Tissue (N=15) |
| Histopathological diagnosed TB (N=15) | 15 | 100 |
| Ziehl- Neelsen stain for AFB (N=13) | 5 | 38.5 |
| Culture for Mycobacterium tuberculosis (N=9) | 5 | 55.5 |
| 6. Treatment (N=15) |
| Surgical excision | 15 | 100 |
| Anti- tuberculous drugs | 14 | 93.3 |
The symptoms in previously reported cases of thymic tuberculosis included retrosternal chest pain, cough and progressive dyspnoea. Tuberculosis of the thymus can also present with non specific general symptoms like fever, lethargy, loss of appetite and weight loss. Three of the cases had a mediastinal mass without any clinical symptoms. Of the 12 symptomatic patients, 4 had evidence of a co-existing pulmonary lesion [1–14]. The symptoms in these patients were slowly progressive except in the six-month-old infant which showed relatively rapid progress requiring medical attention within a week. This rapid progression was probably due to the infant airway being easily compressible leading to prominent complications resulting from airway obstruction [14].
The CT scan of our patient showed an anterior mediastinal mass which was similar to all the previously reported cases whose lesions were located in the antero-superior mediastinum except the one reported by Ruangnapan et al., [14]. In this case, the child had a middle mediastinal mass which was attributed to distortion of mediastinal structures due to over distension of the right lung.
Fitz Gerald et al., reported a case of thymic tuberculosis associated with human immunodeficiency virus (HIV) [4]. Thus, thymic tuberculosis is possibly an immunodeficiency related opportunistic infection [9]. Therefore, routine haematological, biochemical tests and serological investigations for HIV/HbsAg need to be done. In our case, the serological investigations were negative.
As compared to chest X-ray, computed tomography of the thorax is more reliable. The presence of caseating epithelioid granulomas in cytologic and histopathologic examination establishes the diagnosis. Ziehl Neelsen stain for acid fast bacilli, tissue culture and polymerase chain reaction may also be done to confirm tuberculosis. Only 5 of the 15 reported cases had Mycobacterium tuberculosis documented by tissue culture [1–14]. In our case, even though Ziehl Neelsen stain was reported positive, the tissue culture was negative.
Conclusion
Tubercular infection can have varied and sometimes atypical presentations. Proper clinical history, examination and other laboratory investigations along with radiological tools help to evaluate all possible forms of presentation of disease. The occurrence of tuberculosis in unusual locations should be considered when the differential diagnosis of mediastinal masses is made as it is a treatable condition with a good outcome.
[1]. Peabody JW Jr, Walkup HE, Murphy JD, Tuberculoma of the mediastinum; report of the first culturally proved caseJ Thorac Surg 1958 35:397-99. [Google Scholar]
[2]. Duprez A, Cordier R, Schmitz P, Tuberculoma of the thymus. First case of surgical excisionJ Thorac Cardiovasc Surg 1962 44:115-20. [Google Scholar]
[3]. Silvola HJ, Lahdesmaki M, On tuberculosis of the thymusAnn Chir Gynaecol Fenn 1966 55:27-30. [Google Scholar]
[4]. FitzGerald JM, Mayo JR, Miller RR, Jameison WR, Baumgartner F, Tuberculosis of the thymusChest 1992 102:1604-05. [Google Scholar]
[5]. Simmers TA, Jie C, Sie MC, Thymic tuberculosis: a case reportNeth J Med 1997 51:87-90. [Google Scholar]
[6]. Awad WI, Graves TD, White VC, Wong K, Airway obstruction complicating mediastinal tuberculosis: A life threatening presentationAnn Thorac Surg 2002 74:261-63. [Google Scholar]
[7]. Stephen T, Thankachen R, Parihar B, Nair S, Shukla V, Multilocular tuberculous cyst of thymus glandJ Thorac Cardiovasc Surg 2003 126:2093-94. [Google Scholar]
[8]. Sacco O, Gambini C, Aicardi M, Silvestri M, Rossi UG, Tomà P, Thymus tuberculosis poorly responding to anti-microbial therapy in young girl with primary infectionSarcoidosis Vasc Diffuse Lung Dis 2004 21:232-36. [Google Scholar]
[9]. Kpodonu J, Cook JL, Massad MG, Snow NJ, Tuberculosis of the thymus: a case report and review of literatureCurr Respir Med Rev 2005 1:123-26. [Google Scholar]
[10]. Saeig MA, Bernardi FC, Goncalves R, Botter M, Saad Junior R, Pozzan G, Tuberculosis of thymusJ Bras Pneumol 2007 33:355-57. [Google Scholar]
[11]. Iwata T, Inoue K, Mizuguchi S, Tsukioka T, Morita R, Suehiro S, Thymic tuberculosis preoperatively evaluated with Thallium-201 SPECT: two resected casesAnn Thorac Cardiovasc Surg 2007 13:44-46. [Google Scholar]
[12]. Prabhu AD, Ismail ET, Rajendran S, Thomas J, Kallath M, Vellachamy KA, Tuberculosis of thymus-a case reportHeart Lung Circ 2008 17:345-46. [Google Scholar]
[13]. Ganesan S, Ganesan K, Multilocular thymic tuberculosis: case reportBr J Radiol 2008 81:e127-e129. [Google Scholar]
[14]. Ruangnapan K, Anuntaseree W, Suntornlohanakul S, Tuberculosis of the thymus in a 6-month old infant with literature reviewPediatr Infect Dis J 2014 33(2):210-12. [Google Scholar]