Large Dumbbell Shaped Vesicovaginal Calculus Managed with Holmium Laser Cystolithotripsy Followed by Staged Repair of Vesicovaginal Fistula
Ajit Sawant1, Ashwin Sunil Tamhankar2, Prakash Pawar3, Gaurav Vinod Kasat4, Lomesh Kapadnis5
1 Professor and In-Charge, Department of Urology, LTMMC & LTMGH, Mumbai, Maharashtra, India.
2 Resident, Department of Urology, LTMMC & LTMGH, Mumbai, Maharashtra, India.
3 Assistant Professor, Department of Urology, LTMMC & LTMGH, Mumbai, Maharashtra, India.
4 Resident, Department of Urology, LTMMC & LTMGH, Mumbai, Maharashtra, India.
5 Resident, Department of Urology, LTMMC & LTMGH, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ashwin Sunil Tamhankar, Resident, Department of Urology, Room no 219, College Building, LTMMC & LTMGH, Sion, Mumbai-400022, India.
E-mail: ashwintamhankar@gmail.com
Complicated Vesicovaginal Fistulae (VVF) is prevalent in developing countries following obstetric injury. We report a rare case of a large dumbbell shaped vesicovaginal calculus measuring 7x 4.6cm in a patient with recurrent, complicated VVF managed successfully in two stages 6 weeks apart. Holmium laser (30 Watt) cystolithotripsy was used to break the vesical portion of the stone at the waist of the dumbbell, followed by delivery of vaginal part of the stone. Trans-abdominal VVF repair (O’Connor method) with omental interposition flap with right side ureteric reimplant was done after six weeks.
Our case was unique because of occurrence of a larger sized fistula after a gynaecological surgery. She had developed larger stone (weight more than190gm- vaginal component) into the fistula tract. Also she had undergone multiple failed VVF repair attempts before. Use of holmium laser energy to break the stone was unique which minimized the morbidity of the first procedure leading to early recovery followed by staged repair of fistula after six weeks.
Continuous urinary leak per vaginum, Hysterectomy, O’Connor method
Case Report
A 47-year-old female of Caucasian race presented with continuous urinary leak per vaginum since last four years. Since five months she had perineal and suprapubic pain and sensation of bearing down which was increasing gradually. She was operated for total abdominal hysterectomy five years back for dysfunctional uterine bleeding. Patient was informed about the intraoperative bladder injury which was repaired at the same time. Histopathology of the specimen showed benign fibroids. Following the surgery after catheter removal she developed a Vesicovaginal Fistula (VVF). Trans-abdominal VVF repair was attempted twice in other institutes. First was performed two months after the hysterectomy and second was performed after one year for the recurrence. Unfortunately she had persistent urine leak after second attempt of repair also. She did not seek further treatment until she presented to us. Per speculum and per vaginum examination revealed a calculus at the introitus without any significant vulval excoriation. Calculus was seen extending from bladder into vagina through a defect which had indurated margins. She did not have any positive family history of urinary stone disease.
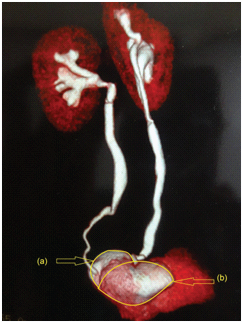
Serum creatinine was normal. Urine culture was positive for E. coli. Computed tomography with contrast (CECT) [Table/Fig-1,2] showed 7x4.6cm (600HU) dumbbell shaped calculus extending from bladder into vagina through a rent in posterior wall of bladder and contrast extravasation was seen through the rent. Upper tracts were normal. On cystoscopy more than three centimeters vesicovaginal defect with oedematous margins was present involving right ureteric orifice. Urinary bladder capacity was adequate.
CECT picture showing 7x4.6 cm dumbbell shaped vesicovaginal calculus with vesicovaginal fistula.

With the due consideration to the total stone load and previous failed attempts of VVF repair, patient was planned for staged surgical approach. First stage was planned to make her stone free. VVF repair was considered electively in second stage. Perioperative antibiotics were started as per sensitivity. Intravesical part of stone was 3x4 cm, smooth, round in contour; which was difficult to be removed by cystolitholapaxy. Holmium laser cystolithotripsy was used to break the vesical portion of stone at the waist of the dumbbell, following which vaginal portion [Table/Fig-3] was removed by gentle manipulation per vaginally which weighed 190 grams. Remaining intravesical part was blasted to powder form with holmium laser. Stone analyses showed crystals of magnesium ammonium phosphate. Trans-abdominal VVF repair (O’Connor method) with omental interposition flap with right side ureteric reimplant was done after six weeks of stone clearance. Supra-pubic and per urethral catheters were removed after 21 days. Voiding trial was successful. The margins of the defect were analyzed for histopathology to rule out any dysplasia or malignancy in view of long standing history of five years. It did not show any dysplastic change. Patient was asked to follow-up regularly. Patient did not have urinary leak till 24 months of follow-up.
Discussion
In developing countries large VVF results following obstetric trauma resulting in field injury to a broader area [1]. In contrast, postsurgical (hysterectomy) fistula results from more direct and localized trauma to otherwise healthy tissues and generally is less than two centimeters. Large calculus in association with VVF is relatively a rare presentation. Risk factors for calculus formation in VVF [2] are presence of foreign body, urinary tract infection and prolonged duration of disease. Urinary bladder calculi were found in 7% of VVF cases evaluated radiologically by Akamaguna et al., [3]. In most of the published series of VVF with stone disease; calculus was approached either by open cystolithotomy or by endoscopic cystolitholapaxy [Table/Fig-4] [4–9]. Bouya et al., have reported seven cases of VVF with stone disease [4]. Six cases out of them developed following caesarean sections and seventh were following obstructed labour. Calculus was removed by cystolithotomy in five of them and through vaginal route in remaining two patients. The extracted calculi varied in size from 3 to 7cm all underwent VVF repairs in staged manner. Another published series by Dalela et al., mentions total 19 patients of VVF with primary vesical stone [5]. All of them occurred following obstructed labour. In 17 cases calculus was approached endoscopically by cystolitholapaxy and two patients required open suprapubic cystolithotomy. All underwent VVF repairs in staged manner. Segawa et al., have reported a case with giant vesicovaginal stone with VVF following hysterectomy and radiotherapy [6]. It was removed by chisel and hammer and it weighed 180 grams. Nnabugwu I et al., have reported a similar case of giant dumbbell shaped calculus in a 34-year-old female following obstructed labour [7]. She had previous two attempts of VVF repair. Calculus was approached by open cystolithotomy for the vesical portion. It was 8cm in longest dimension. Dimensions of the remaining vaginal portion were 9cm x 6cm x 4cm. Ambreen Amna Siddiqui et al., have reported a case of giant vaginolith in 18-year-old female following obstructed labour [8]. Patient presented with signs of infection. Stone was removed vaginally with the use of forceps. VVF repair was done in staged manner. Ming-HueiCheng et al., have reported a case of 85-year-old female patient with history of radiotherapy for cervical carcinoma developing a large 9 cm vesical calculus with VVF [9]. Patient presented in sepsis and unfortunately succumbed to the sepsis.
Reconstructed CECT image with coronal section showing dumbbell shaped calculus {2a) vesical portion’ 2b) vaginal portion}.
Transvaginal portion of calculus being delivered intraoperatively.

Representative articles of cases of stone disease in association with vesicovaginal fistula [4–9].
| S. No | Authors | Number ofpatients | Etiology | Size of calculus/weight | Stone surgery | Vesico-vaginalfistula repair |
|---|
| 1. | Bouyaet al., [4] | 7 | Obstetric Injury | 3-7cm | 5- open cystolithotomy- vaginal route | Staged repair in all |
| 2. | Dalelaet al., [5] | 19 | Obstetric injury | | 17- endoscopic route2-open cystolithotomy | Staged repair in all |
| 3. | Segawaet al., [6] | 1 | Hysterectomyand radiotherapy | 180gm | Open cystolithotomy | Staged repair |
| 4. | Nnab-ugwuI et al., [7] | 1 | Obstructedlabour | 8cm vesicalpart9cm vaginal part | Open cystolithotomy | Patient lost to follow up |
| 5. | Ambreen AmnaSiddiqui et al., [8] | 1 | Obstructedlabour | 5x5cm | Transvaginal extraction | Staged repair |
| 6. | Ming-HueiCheng et al., [9] | 1 | Radiotherapyfor cervicalcarcinoma | 9cm vesical | Sepsis | Death because of sepsis |
| 7. | Our case | 1 | Hysterectomy-dysfunctionaluterine bleeding | 7x4.6cm Vaginalpart- 190 gm | Holmium laser for vesicalportion and vaginal portionby gentle manipulation | Staged repair |
In our case holmium laser was used to break the vesicovaginal junction of the calculus near the defect followed by laser cystolitholapaxy without causing any undue tissue dissection. Laser settings used were 1.5 Joules energy, 20 Hz frequency and 30 Watt power. Trans-vaginal part was easily extracted by gentle manipulation after removal of vesical portion. Bladder component of the stone could not be weighed as it was dusted by laser. Vaginal portion weighed 190 grams. Bladder component was almost one third of the total stone burden as per the CECT image. Abdominal repair of VVF was done six weeks later by open O’Connors method with right side ureteric re-implant. Omental interposition flap was placed. The key to successful repair of VVF lies in the classic principles defined by Couvelaire “good visualization, good dissection, good approximation of the margins and good urine drainage” [10].
Our case was unique because of the unusual finding of a larger size fistula after a gynaecological surgery for benign etiology, multiple prior failed attempts of VVF repair and larger stone load (weight more than190gm- vaginal component) (dimension-7x4.6cm). Intra-vesical part of stone was broken endoscopically by holmium laser and vaginal part of stone was delivered trans-vaginally. Endoscopic approach to the stone with laser using a smaller size sheath was unique. Use of laser energy was the best possible approach for such a large stone with chronically inflamed bladder. This could minimize the morbidity of the first procedure by avoiding open surgery for stone clearance, leading to early recovery. Staged repair after six weeks of the defect helped to resolve stone induced oedema and inflammation of vesical wall which was the key to successful VVF repair in second stage.
Conclusion
In cases of long standing VVF, patients are at risk of formation of large stones in the defect. After ruling out the malignant pathology, minimally invasive approach for the stone clearance in the form of Holmium laser energy can minimize the morbidity of the procedure by avoiding open cystolithotomy. This can lead to early recovery. Following which fistula can be repaired successfully in staged manner after resolution of stone induced oedema and inflammation.
[1]. Dobhada S, Bhansali M, Vesicovaginal fistula with secondary vaginal stonesJ Laparoendosc Adv Surg Tech A 2006 16(4):386-89. [Google Scholar]
[2]. Dmochowski R, Surgery for vesicovagional fistula, urethrovaginal fistula and urethral diverticulumCampbell’s Urology8th ed:1195-217. [Google Scholar]
[3]. Akamaguna AI, Odita JC, Ajabor LN, Okpere EE, Radiology of obstetric vesicovaginal fistulaUrol Radiol 1983 5(4):247-50. [Google Scholar]
[4]. Bouya PA, Odzébé AW, OndongoAtipo MA, Andzin M, Stones associated with vesicovaginal fistulasProg Urol 2012 22(9):549-52. [Google Scholar]
[5]. Dalela D, Goel A, Shakhwar SN, Singh KM, Vesical calculi with unrepaired vesicovaginal fistula: a clinical appraisal of an uncommon associationJ Urol 2003 170(6):2206-08. [Google Scholar]
[6]. Segawa N, Katsuoka Y, Kaneda K, Vesico-vaginal fistula with a giant vesico-vaginal stone: a case reportHinyokika Kiyo 1998 44(7):517-20. [Google Scholar]
[7]. Nnabugwu I, Osakue E, Giant dumb-bell calculus complicating vesico-vaginal fistula - a case reportJ West AfrColl Surg 2011 1(3):91-97. [Google Scholar]
[8]. Ambreen AS, Fehmida M, Pushpa S, Anila Q, Giant vaginolith – case reportJLUMHS 2013 12(2):125-27. [Google Scholar]
[9]. Ming-Huei C, Hsiang-Tai C, Huann CH, Man-Jung H, Ben-Shian H, Peng-Hui W, Vesical calculus associated with vesicovaginal fistulaGynaecology and Minimally Invasive Therapy 2014 3(1):23-25. [Google Scholar]
[10]. Couvelaire R, Reflections on a personal statistics of 136 vesicovaginal fistulasJ Urol Medicale Chir 1953 59:150-56. [Google Scholar]