Umbilical Pilonidal Sinus: A Report of Two Cases and Recent Update of Literature
Susanta Meher1, Tushar Subhadarshan Mishra2, Prakash Kumar Sasmal3, Rakesh Sharma4, Bikram Rout5
1 Senior Resident, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
2 Additional Professor, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
3 Associate Professor, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
4 Senior Resident, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
5 Senior Resident, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Susanta Meher, Senior Resident, Department of Surgery, AIIMS, Bhubaneswar-751019, Odisha, India.
E-mail: chikusus@gmail.com
Umbilical Pilonidal Sinus (UPS) is a rare differential diagnosis of umbilical disease as encountered by general surgeons. They usually present with history of pain and umbilical discharge. Young active adolescent males with dense hairy abdomen with a deep naval are at risk of developing this disease. There are no consensus guidelines for the management of this disease probably because of its rarity. Treatment depends on the type of presentation. Most of the cases are managed by conservative treatment with hair extraction and personal hygiene. Surgery is indicated in case of failure of conservative management. Although umbilectomy is a commonly done procedure, complete sinus excision with reconstruction which can be done to have better cosmesis. Incomplete hair extraction from the sinus tract has been found to be the commonest cause of failure of conservative management. In this paper we have presented two cases of UPS, managed conservatively, with no recurrence after one year of follow-up. We have also presented a recent update on current literature about this uncommon disease.
Recurrence, Suction, Young adult
Case Report
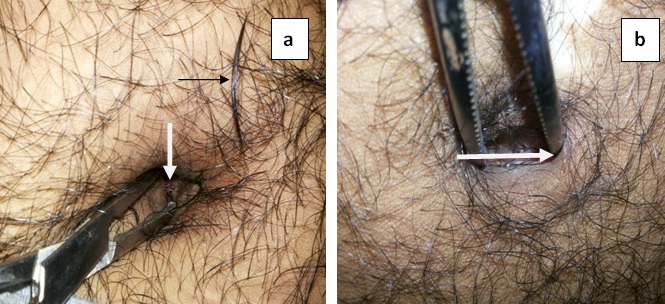
Two young male students of 18-year and 19-year presented to the surgical outpatient department on consecutive days with complaints of pain and discharge from the umbilicus for 5 months and 8 months respectively. Umbilical pain was the starting symptom in both the cases which, was followed by umbilical discharge. The discharge was serous, occasionally mixed with blood and pus. Neither of them had any previous history of similar symptoms or any trauma to the umbilicus. Both the patients had lots of hairs on the abdomen and around the umbilicus with a deep naval. On examination of the umbilicus, in the first case a tuft of hair was found protruding from the sinus opening, which was removed from the deeper part of the umbilicus with pinkish granulation tissue around the sinus opening [Table/Fig-1a]. In the second case, careful examination of the deeper part of umbilicus revealed two small sinus opening with tuft of hair protruding from the sinus [Table/Fig-1b]. Based on the clinical examination and history, a diagnosis of Umbilical Pilonidal Sinus (UPS) was made. The hair in the sinus tract were completely removed and a course of antibiotics along with an anti-inflammatory agent was given. The patients were discharged with the advice of maintaining local hygiene by washing the umbilicus daily before bedtime and regular depilation of hairs around the umbilicus. They were also advised not to wear tight clothing. After a year of follow-up they did not have any symptoms of discharge or infection.
(a) Hairy abdomen with a deep naval showing a sinus opening with granulation tissue (white arrow). A tuft of hair removed from the sinus is kept by the side of umbilicus (black arrow). (b) Hairy abdomen with deep naval showing sinus openings (white arrow).
Discussion
UPS is a rare disease of umbilicus encountered by general surgeons. Although the diagnosis of UPS is not very difficult, it is frequently overlooked in routine clinical practice because of lack of careful examination. The importance of this disease lies in its recurring symptoms and the probability of spread of infection into the peritoneal cavity.
The spectrum of pilonidal disease includes pilonidal sinus, pilonidal cyst and pilonidal abscess. It is a chronic inflammatory disease characterised by granulomatous reaction to fragments of broken hair shaft which enters the dermis through a stretched hair follicle [1]. This was first described by Herbert Mayo in 1833 as a hair containing cyst in the sacrococcygeal region [1–3]. UPS is an uncommon disease; only few 100 cases have been mentioned in the literature. Its incidence is around 0.6% of all cases of pilonidal disease [4]. The first case of UPS was reported by Patey and Williams in 1956 [5,6].
Aetiopathogenesis
The exact pathogenesis of the disease is still unknown. This was originally thought to be of congenital origin. The acquired theory gained importance after the Second World War, when a high incidence of this disease was found among jeep drivers [3]. Extensive research has been done since then by Patey, Scarff, Bascom and Karydakis to prove the acquired origin of this disease [6]. Evidence which supports the acquired theory is the occurrence of this disease in the interdigital web space of barbers and sheep shavers [1].
Patey and Scarff, in 1940-1950, first described hair movement from the surrounding skin under frictional movement into the skin as the initial step in the pathogenesis of this disease [6]. The hair enters the subcutaneous tissue through dilated hair follicles, which is thought to occur in the late adolescence by some unexplained suction mechanism that occurs due to local anatomical predisposition. Foreign body reaction starts, which leads to the formation of a sinus tract lined by granulation tissue. Secondary infection of the sinus can lead to the formation of abscess. In pilonidal sinus of umbilicus, the broken hair enters the skin to the deepest part of the umbilicus and cause foreign body reaction and subsequent development of discharging sinus [1].
The contributory factors for the development of umbilical pilonidal sinus include male gender, obesity, hairy body, tight clothing, deep naval and poor personal hygiene [4]. Coşkun, A et al., found a statistically significant correlation between age, profession, hirsutism, wearing tight clothes, family history of pilonidal sinus and Body Mass Index (BMI) [6]. In our case presence of hairy body, deep naval, tight clothings and poor personal hygiene were found to be the predisposing factors.
Clinical Presentation
In a recent study, umbilical pain (100%) was found to be the most common presenting symptom followed by bloody discharge (69%), purulent discharge (23%), and umbilical mass (26%) [7]. In both of our patients umbilical pain was the initial symptom which was followed by blood mixed serous discharge. In the study, Erylimaz R et al., found that males (92%) were affected more commonly affected than females [Table/Fig-2] [6–12].
Various large series of published literature on umbilical pilonidal sinus [6–12].
| SlNo | Authors | Year ofpublication | Numberof cases | Malepatients(%) | Conservativetreatment givenin % of patients1st Session 2nd Session |
| 1 | Kareemet al., [8] | 2013 | 134 | 121(90.2) | 76.19% 23.8% |
| 2 | Sarmast Met al., [9] | 2011 | 51 | 35(68.6) | 90% - |
| 3 | Fazeli, MSet al., * [10] | 2008 | 45 | 39(86.5) | All underwent surgery |
| 4 | Coşkun, Aet al.,** [6] | 2011 | 31 | 27(87) | - - |
| 5 | Eryilmaz Ret al., [7] | 2005 | 26 | 24(92.3) | 96% 8% |
| 6 | Abdelnour Aet al., [11] | 1994 | 27 | 26(96.2) | 100% 14.8% |
| 7 | James Het al., [12] | 2000 | 5 | 5(100) | 75% - |
*study based on surgical outcome of UPS
**study based on etiological factors associated with UPS
Investigations and diagnosis
Pilonidal sinus is a clinical diagnosis and seldom requires investigations. A careful examination of the sinus under good day light and presence of deep seated hair in the cavity is all that is required to confirm the diagnosis. El-Bakry et al., in a study of 44 patients with umbilical discharge found tuft of hair in the infected umbilicus (pilonidal disease of umbilicus) in most of their patients [13]. Investigations may be required to rule out other differential diagnosis in doubtful cases and spread of infection to the peritoneal cavity [1].
Histopathological examination of the surgical specimen adds little to the confirmation of the diagnosis. Microscopic feature of pilonidal sinus includes keratinized stratified squamous epithelial lining of the sinus tract ending into the sinus cavity. Hair follicles and broken hair shaft can be found on the cavity. Dense inflammatory cell infiltrate comprising lymphocytes, plasma cells, histiocytes, few polymorphs and proliferating congested vessels with numerous foreign body type giant cells can also be seen around hair shafts [14].
Differential diagnosis
The differential diagnosis of umbilical pathology which can mimic pilonidal disease include umbilical hernia, pyogenic granuloma, endometriosis, epidermoid cyst, metastatic tumors, urachus and other commonly encountered congenital anomalies of umbilicus [1].
Treatment and Prevention
There is no consensus or guidelines for the management of this disease because of its rare occurrence. However, the treatment depends on the type of presentation. In case of acute abscess incision and drainage is the treatment of choice [1]. For asymptomatic patients treatment is usually not required except maintaining a good personal hygiene. For recurrent discharging sinus conservative management which include simple hair extraction from the sinus tract, depilation of hair around the umbilicus, maintaining good personal hygiene and avoiding tight clothing, is the first line of management [8,9,12]. In their largest series on umbilical sinus Kareem et al., and Sarmast et al., concluded that conservative treatment should be the first and the main method in the management of UPS [8,9]. They have also found that incomplete hair extraction is the commonest cause for failure of conservative management. Proper instruction to the patients at the time of discharge can further reduce the recurrence [8].
Surgery is indicated after repeated failure of conservative management [1,12]. Although umbilectomy has been advised to reduce recurrence, complete excision of sinus followed by reconstructive procedure are the other available surgical options [1]. Fazeli et al., used reconstructive procedure for the treatment of UPS in their series of 45 cases [10]. They completely excised the sinus after everting the umbilicus and leaving a portion for reconstruction. The purpose of reconstruction was to maintain cosmesis which gives a better psychological impact and to reduce the depth of the umbilicus which is a predisposing factor for this disease [1,10].
Conclusion
UPS should be suspected in all young active male with dense hairy abdominal skin presenting with discharging umbilical sinus. Management of this condition depends on the presenting symptoms. Conservative management with extraction of the hairs from the sinus and personal hygiene should be the first line of treatment in all cases of symptomatic UPS. Failed conservative management is an indication for surgery.
Authors’ Contributions
Dr. Susanta prepared the initial manuscript. Dr. Bikram and Dr. Rakesh collected the data and contributed in preparation of the manuscript. Dr. Prakash and Dr. Tushar critically revised the final version of the manuscript. All authors have read and approved the final version of the manuscript.
Consent
Informed and written consent has been taken from the patients for publication of this case report and accompanying images.
[1]. Al-Kadi AS, Umbilical Pilonidal SinusInternational Journal of Health Sciences 2014 8(3):308-10. [Google Scholar]
[2]. Mayo OH, Observations on Injuries and Disease of Rectum 1833 LondonBurgess and Hill:45-46. [Google Scholar]
[3]. Oueidat D, Rizkallah A, Dirani M, Assi TB, Shams A, Jurjus A, 25 years’ experience in the management of pilonidal sinus diseaseOpen J Gastroenterol 2014 04(01):1-5. [Google Scholar]
[4]. Mustafa G, Akber G, Lodhi JK, Mutahir M, Malik A, Umbilical pilonidal sinusJ Ayub Med Coll 2014 26(1):100-01. [Google Scholar]
[5]. Patey D, Williams ES, Pilonidal sinus of the umbilicusLancet 1956 11 271(6937):281-82. [Google Scholar]
[6]. Coşkun A, Buluş H, Faruk Akıncı O, Ozgönül A, Etiological factors in umbilical pilonidal sinusIndian J Surg 2011 73(1):54-57. [Google Scholar]
[7]. Eryilmaz R, Sahin M, Okan I, Alimoglu O, Somay A, Umbilical pilonidal sinus disease: predisposing factors and treatmentWorld J Surg 2005 29(9):1158-60. [Google Scholar]
[8]. Kareem T, Outcomes of conservative treatment of 134 cases of umbilical pilonidal sinusWorld J Surg 2013 37(2):313-17. [Google Scholar]
[9]. Sarmast MH, Javaherizadeh H, Shahvari MR, Non-surgical treatment of umblical pilonidal sinus in adolescent and adult casesPol Przegl Chir 2011 83(12):652-53. [Google Scholar]
[10]. Fazeli MS, Lebaschi AH, Adel MG, Kazemeini AR, Evaluation of the outcome of complete sinus excision with reconstruction of the umbilicus in patients with umbilical pilonidal sinusWorld J Surg 2008 32(10):2305-08. [Google Scholar]
[11]. Abdelnour A, Aftimos G, Elmasri H, Conservative surgical treatment of 27 cases of umbilical pilonidal sinusJ Méd Liban Leban Med J 1994 42(3):123-25. [Google Scholar]
[12]. McClenathan JH, Umbilical pilonidal sinusCan J Surg 2000 43(3):225 [Google Scholar]
[13]. El-Bakry AA, Discharging umbilicusSaudi Med J 2002 23(9):1099-100. [Google Scholar]
[14]. Fatima U, Yadav YK, Umbilical pilonidal sinus- A rare clinical occurenceIndian Journal of Research 2014 :249-50. [Google Scholar]