Adult Idiopathic Renal Vein Thrombosis Mimicking Acute Pyelonephritis
Arpan Choudhary1, Prasenjit Majee2, Rupesh Gupta3, Supriyo Basu4, Ranjit Kumar Das5
1 Resident, Department of Urology, R G Kar Medical College and Hospital, Kolkata, West Bengal, India.
2 Resident, Department of Urology, R G Kar Medical College and Hospital, Kolkata, West Bengal, India.
3 Resident, Department of Urology, R G Kar Medical College and Hospital, Kolkata, West Bengal, India.
4 Professor, Department of Urology, R G Kar Medical College and Hospital, Kolkata, West Bengal, India.
5 Professor and Head, Department of Urology, R G Kar Medical College and Hospital, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arpan Choudhary, Room 36, KB hostel, R G Kar Medical College Campus, Kolkata -700004, India.
E-mail: jn_rpn@yahoo.co.in
Renal Vein Thrombosis (RVT) is a rarely encountered condition. It occurs due to a hypercoagulable state in the body, caused by nephrotic syndrome and membranous nephropathy in the adults. Mode of presentation is variable. In chronic form, it may remain silent for a long time and presenting later with symptoms of pedal oedema, varicocele, proteinuria. In acute state, it manifests as flank pain, nausea or haematuria. We present a case of 25-year-old male, with left sided flank pain, haematuria and nausea for 4 days. Ultrasound showed enlarged kidney with altered echogenecity. No calculus was found on x-ray. Empirical antibiotics were started considering possibility of Acute Pyelonephritis (APN). With no improvement seen after 3 days along with no growth on urine culture, CT-urography was done. It revealed enlarged non-excreting left kidney with thrombus seen over left renal vein extending into Inferior Vena Cava (IVC). Immediate anticoagulant therapy was started. Patients recovered gradually and after 6 months, follow-up CT showed disappearance of thrombosis. Anticoagulants were withdrawn gradually. So we highlight the possibility of RVT as a differential diagnosis to APN or renal colic and its evaluation and management.
Acute pyelonephritis, Case report, Renal colic
Case Report
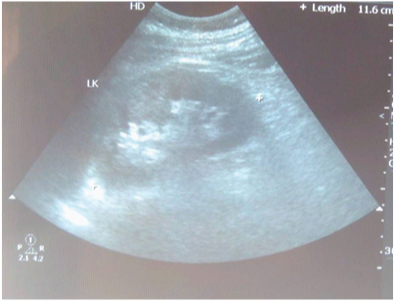
A 25-year-old young healthy male presented with complaint of sudden onset of left side flank pain, vomiting and haematuria for 5 days. There was no history of voiding difficulty or burning micturition. No past history of renal calculus disease or any surgical intervention was noted. On examination, tenderness was noted over left flank, but no mass was felt and rest of the abdominal examination was normal. Routine blood parameters showed leukocytosis (15,000 wbc/mm3) and normal level of urea (27mg%), creatinine (0.9 mg%), electrolytes (Na-140, K-3.4) and sugar (110mg%). Urine test revealed plenty of pus cell and RBC; however culture of urine was sterile. Ultrasound KUB (kidney, ureter and bladder) showed enlarged left kidney with altered echogenecity. Kidney outline was well maintained and no pelvicalyceal system fullness or calculus was found [Table/Fig-1]. X-ray KUB was normal.
USG showing enlarged kidney with mild alteration of echogenecity.
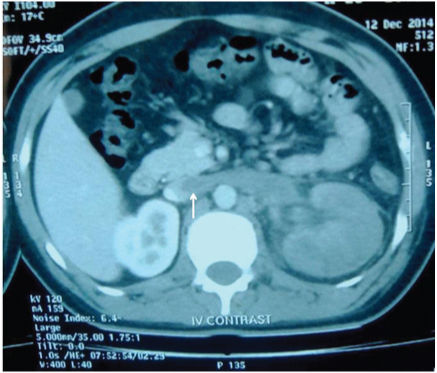
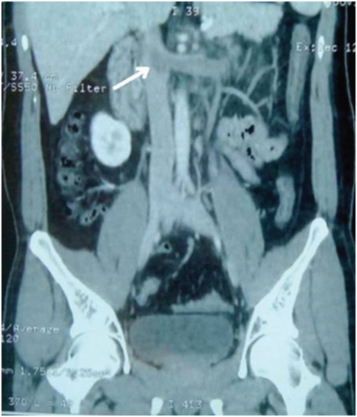
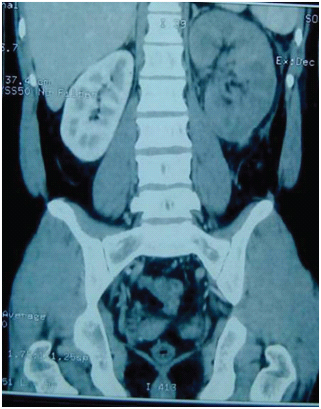
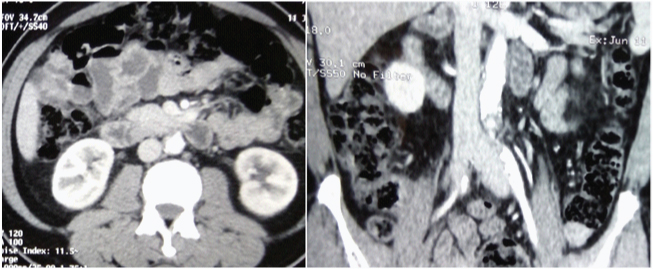
Patient was put on i.v. empirical antibiotic consisting of Cefoperazone sulbactam, 1.5 gm, bd and Levofloxacillin 500 mg od, considering the possibility of acute pyelonephritis. After 3 days of therapy, patient was still symptomatic with persisting nausea and flank pain (APN). In view of diagnostic dilemma, CT-urography was done. It revealed grossly enlarged left kidney with no uptake of contrast and thrombosis of left renal vein without any extension to Inferior Vena Cava (IVC) [Table/Fig-2,3 and 4]. Right kidney and bladder were normal.
CECT axial view displaying enlarged non enhancing left kidney with renal vein thrombosis (white arrow).
CECT coronal view revealing renal vein thrombosis, approaching IVC (white arrow).
CECT coronal view indicating enlarged non enhancing left kidney.
Patient was put on anticoagulant therapy, using enoxaparin 40 mg subcutaneously, of for 7 days. Patient was switched over to oral warfarin therapy afterwards, which was then continued for 6 months after nephrologist consultation. In search of cause of thrombosis, evaluation for nephrotic syndrome was done. A 24-hour urine protein and serum albumin were within normal limit. No cast was found in urine microscopy. Coagulation profile and platelet counts were also normal. Renal biopsy was not done, as there was no evidence found favouring the possibility of renal parenchymal disease. Serum for anti-phospholipid antibody was negative. Patients improved symptomatically and follow-up scan after 6 months showed clearance of thrombus and improved renal appearance [Table/Fig-5]. Warfarin was tapered gradually after 6 months. Renal function remained stable throughout the period.
Follow up CT after 6 months showing thrombus resolution and good enhancement of the left kidney.
Discussion
Renal Vein Thrombosis (RVT) is a rare condition. It has a bimodal way of presentation, affecting mainly adults and neonates [1]. According to virchow’ triad, endothelial injury, hypercoagulability and stasis are the principal pathological factors responsible [Table/Fig-6]. In neonates, dehydration and sepsis account for majority of the cases and in adults; nephrotic syndrome is the most common etiology, followed by malignancy, trauma, puerperium etc [2]. In adults with parenchymal pathology and malignancy, RVT usually has an insidious way of onset, being asymptomatic initially, with presence of pedal oedema and varicocele later on. In setting of non-parenchymal pathologies such as trauma, surgery, endovascular intervention and Antiphospholipid Syndrome (APS), it may present acutely with flank pain, fever, vomiting and haematuria. Here, it mimics as Acute Pyelonephritis (APN), renal colic, ureteric colic, cholecystitis and appendicitis. In case of bilateral RVT and in solitary kidney, acute renal failure may ensue [3]. Thrombosis may also extend to IVC and fear of acute pulmonary embolism may ensue. Acute Renal Failure (ARF) is rare with normal contralateral kidney. Literature also reports few cases of idiopathic variety, despite extensive work up [4,5].
Aetiologies of renal vein thrombosis, classified by pathogenesis.
| Endothelial damage | Stasis | Hypercoagulability |
|---|
| HomocystinuriaEndovascular interventionRenal transplantAcute rejectionSurgeryAbdominal trauma | DehydrationRetroperitoneal fibrosis causing compressionor kinkingAbdominal neoplasmHypovolemia | Nephrotic syndromeGlomerulonephritisAntiphospholipid antibodysyndrome Protein C/S/Antithrombin deficiencyFactor V LeidenOCD intake |
Ultrasound in RVT shows enlargement of kidney, hyperechogenecity with loss of corticomedullary differentiation. It also helps to rule out hydronephrosis, calculi and perirenal collection; however differentiation from APN may not be possible. Colour Doppler helps in visualization of renal artery and vein, however sensitivity is low in detecting thrombosis. In renal transplant, it has definite role in suspected RVT [6,7]. Urine examination may show proteinuria, cast or haematuria, favouring possibility of APN or nephritic syndrome. Renal biopsy is confirmatory. CECT is the modality of choice with sensitivity approaching 100%. It also helps to rule out other possibilities [8]. In case of suspicion of IVC thrombosis, CT angiography (CTA) or MR Angiography (MRA) can be done. Invasive test such as renal venography and venacavagraphy are out of favour now-a-days.
Treatment of RVT is anticoagulation, while thrombolysis and thrombectomy is reserved in selected cases. Initially therapy is started with heparin. Low Molecular Weight Heparin (LMWH) can be utilized with added benefits [9]. After 1 week of heparin therapy, warfarin is started and continued for 6 months to one year, depending on the resolution of thrombosis and return of renal function. Throughout the anticoagulant treatment, prothrombin time is kept between 2.0-2.5 times of the normal value. Monitoring of disease is done with serial USG/colour doppler. IVC filter is used for prophylaxis of Acute Pulmonary Embolism (APE), in case of IVC thrombosis. In case of contraindication to anticoagulation therapy, APE, Bilateral RVT, ARF, local thrombolysis is an alternative and superior to systemic therapy [10]. Recovery of renal function is delayed and may not be complete in all cases. Long term monitoring is advised. In nonresponders with severe symptoms, impending rupture and in presence of concomitant tumour, nephrectomy is the last resort.
Conclusion
RVT cases may go unrecognised due to lack of typical clinical manifestations. With high clinical suspicion, appropriate diagnostic testing and prompt therapy, late sequel of RVT can be minimized. Current trends favour CECT scan as the diagnostic modality of choice. Anticoagulation has emerged as the mainstay of treatment in the majority of the cases. Radiological interventions including thrombolysis with or without thrombectomy and ablative surgical measures like nephrectomy are only required in highly selected cases.
[1]. Brenner B.M, Disorders of renal arteries and veins. in: The kidney 2004 7th edPennsylvaniaSaunders:1584 [Google Scholar]
[2]. Ajmera A, Joshi A, Kamat B, Germaine P, Idiopathic acute renal vein thrombosis in a young healthy woman with no hypercoagulable state taking oral contraceptivesAm J Med Sci 2010 339(4):38082 [Google Scholar]
[3]. Bashir R, Tinkel J, Malhotra D, Renal vein thrombosis: a case reportAngiology 2007 58(5):64043 [Google Scholar]
[4]. Chikaraishi T, Kobayashi S, Harada H, Idiopathic and spontaneously regressing thrombus in right renal vein and inferior vena cavaInt J Urol 1997 4(1):835 [Google Scholar]
[5]. Ignjatović I, Ilić M, Marković N, Idiopathic thrombosis of the renal veinSrp Arh Celok Lek 1995 123(78):21820 [Google Scholar]
[6]. Seupaul RA, Stepsis TM, Doehring MC, Idiopathic renal vein thrombosis in a healthy young woman with flank painand feverAm J Emerg Med 2005 23(3):417-19. [Google Scholar]
[7]. Radermacher J, Ultrasonography of the kidney and renal vessels. I. Normal findings, inherited and parenchymal diseasesUrologe A 2005 44(11):1351-63.quiz 1364 [Google Scholar]
[8]. Alvarez-Castells A, Sebastiá Cerqueda C, Quiroga Gómez S, Computerized tomography angiography of the renal vesselsArch Esp Urol 2001 54(6):603-15. [Google Scholar]
[9]. Hmidi M, Hani MA, Hafsia G, Idiopathic renal vein thrombosis. About two casesTunis Med 2006 84(6):37476 [Google Scholar]
[10]. Asghar M, Ahmed K, Shah SS, Siddique MK, Renal vein thrombosisEuropean Journal of Vascular and Endovascular Surgery 2007 34(2):217-23. [Google Scholar]