Provisional or interim restorations are commonly used restorations in dentistry. The increased desire for aesthetics has lead interim restorations to serve as valuable diagnostic tools in fixed prosthodontics. The dentist can gain the patient’s confidence by successfully handling this intermediate phase of the treatment; thus, promisingly influence the ultimate success of the final restoration.
Provisional restorations can be classified into two types i.e., prefabricated or custom made. Prefabricated forms include stock aluminium cylinders (tin cans), anatomic metal crown forms, clear celluloid shells, and tooth coloured polycarbonate crown forms. They can be used only for single tooth restorations. Custom made crowns and Fixed Partial Dentures (FPD) can be fabricated by direct or indirect methods from different kinds of resins [1].
The fabrication of an ideal provisional restoration is crucial for gingival health, protection of pulp tissue and space maintenance and serves as blueprint in the laboratory for the final prosthesis to be fabricated. Since provisional restoration should be the replica of the definitive restoration, it must meet all the requirements of the definitive restoration with the exception of longevity and possibly sophistication of colour [2].
Interim fixed restorative materials can be divided into four groups based on their composition as Polymethylmethacrylate (PMMA), polyethyl or butyl methacrylate, microfilled bisphenol A-glycidyldimethacrylate (Bis-GMA) composite resin, and Urethane Dimethacrylate (UDMA) (light-polymerizing resins). Epimine resin which for a decade also was used for this purpose is no longer available. No one interim material is superior in all aspects and restorative dentist must select the product based on factors such as ease of manipulation, cost effectiveness, aesthetics, strength and marginal fit [1].
The flexural strength of an interim restorative material is greatly tested during mastication. Long span fixed provisional prosthesis functions as a beam, greater the length of the edentulous area being spanned with pontic, greater is the flexure of the restoration. So an understanding of the mechanical properties of these materials is important in determining whether the restoration will be able to survive repeated functional forces in the oral environment. In some clinical scenarios like bite raising step in case of full mouth rehabilitation cases, long span FPDs, TMJ dysfunction therapies and in patients exhibiting parafunctional habits the flexural strength of the interim restorations plays an important role [3].
Few studies on provisional restorations have evaluated flexural strength following polymerization. However, this method has limited ability in determining the clinical behaviour of a dental material as it evaluates the failure of a material without ageing the material. Ageing of the material by a process called thermal cycling can cause material fatigue and fastens/hastens up the deterioration of the material [4].
Therefore, the aim of the study was intended to compare the flexural strength after thermocycling of four chemically different provisional materials used in fixed prosthodontics. The objective of the study was to evaluate the flexural strength of the following provisional resins used in the study: (1) Self cure (2) Heat cure (3) Chemical cure (4) Light cure resins
The null hypothesis was that there is no difference between flexural strength of these interim restorative materials.
Materials and Method
The present in-vitro study was conducted in the Department of Prosthodontics, Sibar Institute of Dental Sciences, Takkellapadu, Guntur, Andhra Pradesh, India. Before commencement of this laboratory study, the study design was approved by the Institutional Ethical Committee.
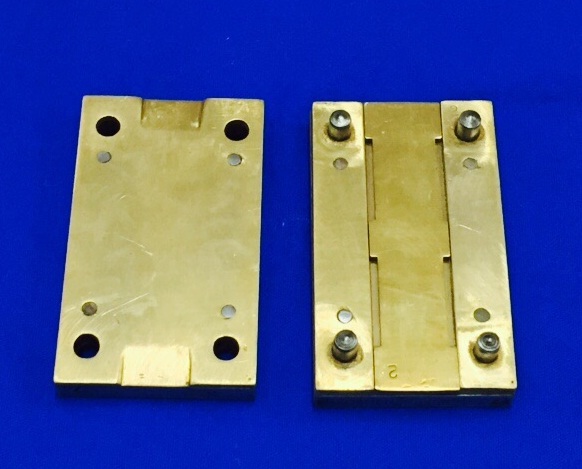
A customized three piece brass flask of dimensions 85mmx 50mmx25mm was machined, compromising four equal sized mould spaces measuring 25mm in length, 2mm in width and 25mm in height (25mmx2mmx2mm) corresponding to the dimensions of the specimens according to ADA specification no.27 [Table/Fig-1].
The interim restorative materials compared in this study were four tooth coloured resin materials currently used for making interim fixed prostheses [Table/Fig-2]. These tested materials are representative of all four types of interim restorative materials.
Materials used in the study.
| Resin Type | Polymerization Method | Manufacturer | LOT Number |
|---|
| Poly methyl methacrylate | Auto polymerizing | Dental Products of India Ltd., Mumbai, India | 3452 |
| Poly methyl methacrylate | Heat cure | Dental Products of India Ltd., Mumbai, India | 4133 |
| Bis-GMA composite | Auto polymerizing | Integrity, Dentsply Caulk, USA | 1502031 |
| Urethane Di Methacrylate | Light Cure | Revotek, GC Corporation, Japan | 150326 |
Fabrication of Group A Specimens (PMMA Resin): The material is supplied in powder and liquid form as polymer and monomer respectively and the main component of the material is PMMA. The manipulation of the material was carried out according to the manufacturer’s instructions. The standard polymer/monomer ratio is 1.0g/0.5ml. Spatulation was done for approximately 20–30 seconds to evenly wet the polymer particles. This material was placed in to the lubricated mould space and the flask compartments were approximated under constant pressure until the flash comes out. After five minutes, the samples were retrieved and polished. Similarly, all the 10 samples were fabricated.
Fabrication of Group B Specimens (Polymethyl Methacrylate Resin): Wax patterns were made by pouring molten modelling wax into the customized mould space of dimensions 25mm×2mm×2mm and conventional flasking was done using two pour technique. Dewaxing was done. Short curing cycle was followed by placing the flasks at 74°C for 2 hours and then the temperature was raised to 100°C and processed for 1 hour. After completion of the polymerization cycle, the flasks were allowed to cool in the water bath to room temperature before deflasking and samples were retrieved.
Fabrication of Group C Specimens (Bis-GMA Composite Resin): The material is supplied in cartridge form as base and catalyst pastes and the main component of the material is Bis-GMA. The cartridge was placed in the mixing gun and the material was loaded into the mould spaces of the lubricated brass flask. The flask compartments are approximated and after five minutes, the samples were retrieved and polished. All the samples were prepared in the same way.
Fabrication of Group D Specimens (UDMA Resin): The material is supplied in the form of a putty stick and the main component of the material is UDMA. Required amount of material was dispensed using a spatula and the material was kneaded with fingers to soften it. Initial light curing was done using a Light Emitting Diode (LED) powered visible light curing unit for 10 seconds in fast cure mode (440–480nm) for each specimen according to the manufacturer’s instructions. The specimens were then retrieved and final curing was done for 10 minutes with Delta Polymat Light Curing Unit.
After obtaining the 40 specimens, they were assessed for internal or external flaws. Later finishing procedures were carried out using stone burs and 1200 grit abrasive waterproof paper and polishing was done using pumice slurry. Then conditioning of these specimens was done by storing in the artificial saliva (Wet Mouth, Batch no50015) for 14 days [Table/Fig-3].
Specimens stored in artificial saliva.

Thermocycling was done by immersing the samples in two temperature controlled water baths maintained at 5°C (cold bath) and 55°C (hot bath). The samples of each group were packed in separate colour coded bags. These bags were put in cold and hot water baths alternatively and the dwell time was 6 seconds in each water bath. A total of 2500 cycles were carried out in similar manner.
These specimens were subjected to three point bend test, at a crosshead speed of 0.75mm/min carried out by Universal Testing Machine. The load was applied to the centre of the specimen until the specimen fractures. The breaking load was noted in Newton. The procedure was repeated accordingly for all the specimens [Table/Fig-4]. These breaking load values were converted to flexural strength using the formula,
Specimens tested on universal testing machine.

S=3FL/2bd2
Where, S = Flexural strength/modulus of rupture in Mega Pascals, F = Load at the fracture point in Newton’s at which specimens failed between load bearing edges, L= Length of the support span (15mm), b = Width of specimen (2mm), d = Thickness of the specimen (2mm).
Statistical Analysis
Substituting the above formula for each load value obtained, the corresponding flexural strength was calculated for all 40 specimens. The flexural strength values obtained were in Mega Pascal (Mpa) [Table/Fig-5]. The data were analysed and computed with statistical software package SPSS 16 version (Chicago.inc). Statistical tests used were Mann-Whitney U test for comparison between any two groups and Kruskal-Wallis test for comparison between four groups. A significance level of p<0.05 was used for all statistical analysis.
Comprehensive tabulation of mean flexural strengthin Mpa of Group A, B, C and D specimens.
| Specimen | Widthin mm | Thicknessin mm | Lengthin mm | Flexural strength in Mpa | Flexural strength in Mpa | Flexural strength in Mpa | Flexural strength in Mpa |
|---|
| B | D | L | Group A specimens | Group B specimens | Group C specimens | Group D specimens |
|---|
| 1 | 02 | 02 | 25 | 78.76 | 91.23 | 101.78 | 60.01 |
| 2 | 02 | 02 | 25 | 79.01 | 94.02 | 105.56 | 60.56 |
| 3 | 02 | 02 | 25 | 80.01 | 91.86 | 99.44 | 59.07 |
| 4 | 02 | 02 | 25 | 79.67 | 93.32 | 102.45 | 59.56 |
| 5 | 02 | 02 | 25 | 78.21 | 91.12 | 102.57 | 61.01 |
| 6 | 02 | 02 | 25 | 80.09 | 90.09 | 106.84 | 61.06 |
| 7 | 02 | 02 | 25 | 79.78 | 94.06 | 103.34 | 60.45 |
| 8 | 02 | 02 | 25 | 78.56 | 92.23 | 104.09 | 60.87 |
| 9 | 02 | 02 | 25 | 79.22 | 91.99 | 98.44 | 59.58 |
| 10 | 02 | 02 | 25 | 80.0 | 92.56 | 99.23 | 59.07 |
| Mean | 79.13 | 91.86 | 102.98 | 60.01 |
Results
The mean flexural strength of all group specimens as tabulated in [Table/Fig-6] demonstrate higher flexural strength for Group C (102.98 Mpa) followed by Group B (91.86 Mpa), Group A (79.13 Mpa) and Group D (60.01 Mpa).
Comparison of flexural strengths between any two groups was evaluated by Mann-Whitney U test. There is a significant difference between the means of different groups (p<0.05).
| GROUP | MEAN | SD | p-value |
|---|
| GROUP A | 79.13 | 0.65 | <0.001Significant |
| GROUP B | 91.86 | 1.24 |
| GROUP A | 79.13 | 0.65 | <0.001Significant |
| GROUP C | 102.98 | 2.52 |
| GROUP A | 79.13 | 0.65 | <0.001Significant |
| GROUP D | 60.01 | 0.71 |
| GROUP A | 91.86 | 1.24 | <0.001Significant |
| GROUP C | 102.98 | 2.52 |
| GROUP B | 91.86 | 1.24 | <0.001Significant |
| GROUP D | 60.01 | 0.71 |
| GROUP C | 102.98 | 2.52 | <0.001Significant |
| GROUP D | 60.01 | 0.71 |
Comparison between mean flexural strength values between any two groups were analysed using Mann-Whitney U test and tabulated in [Table/Fig-6]. There were significant differences between any two materials tested (p<0.05).
Comparison between mean flexural strength values between four groups were analysed using Kruskal-Wallis test and tabulated in [Table/Fig-7]. The Kruskal-Wallis test indicated a significant difference between the interim materials (p<0.05). The greatest flexural strength belonged to Bis-GMA composite resins followed by heat cure methacrylate resins, autopolymerizing methacrylate resins and least for light cure resins.
Comparison of flexural strengths between four groups was evaluated by Kruskal-Wallis test. There is a significant difference between the means of different groups (p<0.005).
| GROUP | Lower bound | Upper bound | Mean | Standard deviation | p-value |
|---|
| Group A | 78.21 | 80.09 | 79.13 | 0.65 | <0.005 (Significant) |
| Group B | 90.09 | 94.06 | 91.86 | 1.24 |
| Group C | 98.44 | 106.84 | 102.98 | 2.52 |
| Group D | 59.07 | 61.06 | 60.01 | 0.71 |
Discussion
Provisional restorations are designed to enhance aesthetics, stabilization and function for a transitional period for fixed prosthesis [5]. The ideal properties to be possessed by provisional restorative materials are good marginal adaptation, adequate retention and resistance to dislodgement during normal masticatory function, durable, not irritating to pulp and other tissues, low exothermic reaction, non-porous and dimensionally stable; aesthetically acceptable shade selection, translucent tooth like appearance, colour stability, easy to fabricate, relieve and repair, short setting time, conducive to routine oral home care cleaning procedures, low incidence of localized allergic reactions, and should have a highly polishable, plaque and stain resistant surface. However, the long term maintenance of these provisional restorations can present considerable difficulty for both the patient and the dentist [6]. Repair procedures can be time consuming and breakage of these restorations can lead to tooth movement, functional and aesthetic problems. Hence, provisional restorations made of appropriate material are considered to be critical components of fixed prosthodontic treatment [7].
Many commercially available provisional restorative materials have evolved with the same base resin group having varying physical properties depending upon the type, amount, geometry and size of the filler particles and the properties of the polymer matrix. However, no single material was proved to be ideal for all clinical situations. Therefore, careful understanding of the composition and mechanical properties of the materials available is required to select a material that best suits the clinical situation [8].
In this study the flexural strength of four types of provisional restorative resin materials were compared after thermal cycling i.e., autopolymerizing PMMA (Group A); heat activated PMMA (Group B); autopolymerizing Bis-GMA composite resin (Group C) and light activated UDMA (Group D). These materials were chosen because of their wide clinical usage.
Flexural strength tests are essentially a test of a bar supported at each end, subjected to three point flexure. These tests evaluate stresses as compressive at the point of application of load and tensile and shear at the point of resistance to the load applied, making them similar to the stresses produced by multi-unit FPD. Flexural strength can be determined by three point bend test in Universal Testing Machine. Various studies have documented about the use of three point bend test in order to determine the flexural strength of provisional restorative resins. The flexural strength of provisional materials may be influenced by saliva, food components, beverages and interactions among these materials. The changes that occur to a material when subjected to various temperature regulations should be assessed when the material is used in the long run. Thermal cycling is one such process which causes ageing of the material and simulates changes in oral environment [3,9].
So, the changes that occur to a material when subjected to various temperature regulations should be assessed when the material is used in the long run. A total of 10,000 cycles represent one year on clinical usage. Hence, 2,500 cycles represents the material studied is subjected to stresses equivalent to its clinical usage of three months. Mouth is subjected to temperature range between –8°C and +81°C, and the resulting temperatures on the surfaces of a construction between 5°C and 55°C [10].
Various studies conducted by Nejatidanesh et al., Lang et al., and Yao et al., supported the use of thermal cycling process to age the material. To partially simulate the oral environment, specimens were stored for 14 days in artificial saliva and thermocycled for 2,500 cycles (5°C to 55°C). Then standard three point bending test was conducted on the specimens [3,9,10].
Analyzing the data, within the limitations of the study the mean flexural strength of the materials compared were in the following descending order: Autopolymerizing Bis-GMA (Group C) > heat activated PMMA (Group B) > light activated UDMA (Group D) > autopolymerizing PMMA (Group A).
According to the International Organization for Standardization (ISO 4049) and the American National Standards Institute (ANSI)/American Dental Association (ADA) Specifications no. 27, an interim fixed prosthesis material must have a minimum strength of 50 Mpa when a bar of the material undergoes a 3-point bend test [11]. All the specimens tested in this study had flexural strength values more than 50 Mpa, which infers that all the materials, can comfortably be used for the fabrication of provisional restorations.
Bis-GMA composite resin material exhibited greater flexural strength than the other materials because of multifunctional monomers, which increase the strength due to cross-linking with other monomers. Additionally, they contain inorganic nano fillers which further improve the strength of the material [3]. The method of dispensing Bis-GMA by cartridge delivery system was accurate and the auto mixing system ensures complete polymerization. It is hydrophobic in nature, ensuring minimal water uptake and thus reducing the plasticizer action when stored in artificial saliva [12,13].
Hasselton et al., compared flexural strength of methacrylate base resins and bis-acryl resins after immersing in artificial saliva for 10 days. They concluded that due to chemical composition i.e., difunctional and capable of crossing linking with other monomer chain bis-acryl resins demonstrated significantly superior flexural strength over traditional methacrylate resins which were mono functional in their chemical composition [12].
Heat cured PMMA resins were ranked next to Bis-GMA resins because heat polymerization eliminates excess residual monomer (0.2%-0.5%), leading to a higher degree of polymerization and therefore makes the material stronger. However, the presence of even small amount of residual monomer and its evaporation makes the material to absorb water when placed in artificial saliva. These water molecules interfere with the polymer chains and act as plasticizer when stored in artificial saliva. The main disadvantages with heat cure acrylic are time consuming and exhaustive laboratory procedures [14,15].
Autopolymerizing PMMA resins are mono functional, low molecular weight linear molecules that exhibit decreased strength and rigidity. However, the reasons for decreased flexural strength could be lack of time available for the monomer in self cure resin to wet the polymer beads. So, a less homogenous polymer is produced. The material deforms under stresses subjected by thermal cycling unlike other materials [3,15].
The flexural strength of the light polymerized urethane dimethacrylate composite resin material was comparatively low among all the materials compared. The reason for this result was mainly because of less crystalline silica filler particles (15%-35%) when compared to normal composites (85% by weight). These glass filler particles are slowly leached out in the presence of artificial saliva and thus, reducing the flexural strength of the material. Secondly, the material exhibits inherent brittleness to resist the stress that it is subjected to during thermal cycling procedure [14,16].
Nejatidanesh et al., conducted a study to compare the flexural strength of seven provisional restorative materials. In their study, composite resins exhibited better flexural strength values when compared to acrylic resins. Within the acrylic resin groups, polyethyl methacrylate exhibited higher flexural strength values when compared to polymethyl methacrylate and vinyl ethyl methacrylate resins. However, the difference in flexural strength performance is material specific and hence, direct comparison with other studies was not possible [3].
The results obtained in this study are consistent with those of past studies [3, 17–20] in which flexural strength of bis-acryl resins was higher than conventional provisional restorative materials [Table/Fig-8]. However, the direct comparison among various studies cannot be done as this property is material specific and continuous developments to improve the material properties are taking place.
Various studies conducted to know the effect of thermocycling on interim resin materials.
| AUTHOR | MATERIALS TESTED | RESULTS |
|---|
| Balkenhol M, et al., [17] | Flexural strength (FS) and Flexural Modulus (FM) of four materials (Trim, Luxatemp AM Plus, Luxatemp AM Plus Solar and Cool Temp Natural) were tested in a three point bending test at various times after mixing (37°C dry/water) including thermocycling (5000x, 5-550C). | FS and FM significantly depend on the time after mixing. Composite resin based materials are preferred versus methacrylate resins due to more favorable mechanical properties. |
| Nejatidanesh F, Momeni G, Savabi O [3] | Seven different interim materials (Trim, Acropars, Protemp 3 Garant, Unifast LC, TempSpan, Tempron, Duralay) were stored in artificial saliva for 14 days and thermocycled for 2500 cycles (5°C to 55°C) and flexural strength was then evaluated. | Bis-acryl interim materials exhibited higher flexural strength than the methacrylate resins tested in this study. |
| Bacchi A, et al., [18] | Flexural strength of four resins (Luxatemp and Structur 2 are Bis-acryl based resins and Duralay and Alike are methacrylate based resins) were tested after thermal cycling. | The Bis-acryl resins exhibited superior flexural strength than the methacrylate ones. |
| Thompson GA, et al., [19] | Effect of storage media, storage temperature, storage time, thermocycling, postpolymerization thermal treatment or application of a surface Sealer on Flexural strength and microhardness of poly methyl methacrylate (Jet Acrylic) and 2 bis-acryl composite resin (Protemp3 Garant and Integrity) interim restorative materials were evaluated. | All experimental treatments investigated had significant effects on flexural strength, with material and thermocycling being dominant. Material and age had a significant effect on impact strength which suggests usage of Bis acrylic composite resins for prolonged use. |
| Yao J, Li J, Wang Y, Huang H [20] | Flexural strength and marginal accuracy of 2 traditional Bis-acryl composite interim materials (Protemp 4 and Structur 2 SC/QM) and 2 CAD/CAM interim materials (Teilo CAD and VITA CAD-Temp) before and after thermocycling. | Teilo CAD showed the highest mean flexural strength of the 4 interim materials before and after thermal cycling, and VITA CAD-Temp demonstrated the lowest. The margin discrepancies were higher for the bis-acryl interim crowns than for the CAD/CAM crowns before and after thermal cycling. |
Finally, it should be mentioned that flexural strength is only one of a number of factors influencing the success of an interim prosthesis. A strong material may possess other less desirable characteristics. For example, a restorative material may be difficult to manipulate, have tendency to stain easily, lack polishability, or may not be aesthetically pleasing. The clinician must be aware of all attributes of various materials and choose the interim material appropriate for each patient.
Recommendations and Future Prospects
1) Further studies can be done using three unit FPD fabricated on cast dies either using the same fabrication/polymerization technique or milling from a block of material.
2) Further research can be improvised by using various combinations of frequency, loads and cycles in order to further evaluate a clinical situation similar to what occurs on a daily basis with meals, swallowing and para-functional habits.
Limitation
Although the study was designed in an attempt to simulate in-vivo conditions, this experimental design still had limitations in replicating clinical conditions accurately. Another aspect in clinical situations is that an immediate load is placed on the interim prosthesis once it is cemented into place whereas in this experiment a load was not applied until 14 days of artificial saliva storage.
Conclusion
Within the limitations of the study, Bis-GMA composite resin can be considered as superior material for long term provisionalization, as it exhibited greater flexural strengths. Also, the fabrication of provisional crowns with Bis-GMA composite resin is much easier, as it is delivered in cartridge system. Although heat cured PMMA resins exhibited higher flexural strength values, the fabrication of heat cure provisional crowns require additional laboratory steps and is time consuming. However, it is the best material of choice for long term provisionalization when economic factors are to be considered.