Tuberculosis of Distal Radius Presenting as Cystic Lesion in a Nine-Month-Old Infant: A Rare Case Report
Aniruddha Sinha Sarkar1, Anant Kumar Garg2, Abhishek Bandyopadhyay3, Sanjay Kumar4, Sumanta Pal5
1 Junior Resident, Department of Orthopaedics, Nil Ratan Sircar Medical College and Hospital, Kolkata, West Bengal, India.
2 Assistant Professor, Department of Orthopaedics, Nil Ratan Sircar Medical College and Hospital, Kolkata, West Bengal, India.
3 Junior Resident, Department of Pathology, Nil Ratan Sircar Medical College and Hospital, Kolkata, West Bengal, India.
4 Associate Professor, Department of Orthopaedics, Nil Ratan Sircar Medical College And Hospital, Kolkata, West Bengal, India.
5 Junior Resident, Department of Orthopaedics, Nil Ratan Sircar Medical College and Hospital, Kolkata, West Bengal, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aniruddha Sinha Sarkar, Room no. 14, Doctor’s Quarters, 25 Dixon Lane, N.R.S. Medical College and Hospital, Kolkata-700014, West Bengal, India.
E-mail: dr.asinhasarkar@gmail.com
Tuberculous osteomyelitis affecting long bones is a rare form of tuberculosis. Among infants born in endemic region, often it is difficult to diagnose owing to its subtle clinical features. Here, a case of tuberculous osteomyelitis affecting the distal radial metaphysis is reported, presenting as a cystic lesion in a nine-month-old male infant. Open biopsy with curettage was performed followed by filling of the cavity with synthetic bone substitute (beta tricalcium phosphate granules). The diagnosis was confirmed by histopathological examination and demonstration of acid fast bacilli. Further treatment with anti-tubercular drugs led to clinical and radiological improvement. This case report highlights the importance of keeping tuberculosis as a differential diagnosis while dealing with cases with similar presentation in an endemic region.
Bone substitutes, Osteoarticular, Osteomyelitis
Case Report
A nine-month-old male infant was brought to orthopaedic outpatient department of N.R.S. Medical College and Hospital, after his mother noticed a swelling over his left distal forearm 1 month back. The swelling gradually increased in size and was painful. He avoided using his left hand during activities. He also had decreased appetite and Failed to gain weight since he started weaning at 6 months of age. There were episodes of evening rise of temperature and night cries in the previous 3 months. There was no preceding history of significant trauma or chronic cough. As his symptoms persisted even after taking analgesics and antibiotics, he was referred to our hospital. He was the only child of his parents. He was born through normal delivery, at term in a government hospital weighing 2.7 kilograms at birth and underwent BCG vaccination. Apart from his mother, he was breastfed occasionally by his maternal aunt. His aunt had a history of pulmonary tuberculosis, treated 5 years back with multidrug therapy of anti-tubercular drugs.
General examination was normal and showed no pallor, icterus or any signs of malnutrition. He was apparently a healthy playful child. His developmental milestones were on par with his age. On local examination there was a tender globular swelling of about 3 cm diameter involving the volar aspect of left distal radius with smooth surface, hard consistency, diffuse margin. The swelling was fixed and continuous with the underlying bone. Skin was normal without any scar, ulcer or discharging sinus. Wrist joint was mobile but range of movement could not be examined as it was painful. There was no neurovascular deficit. No significant enlargement of axillary lymph nodes was palpated.
On laboratory examination, haemoglobin level and leucocyte count were within normal limits. ESR was 45mm/hr and C-reactive protein was elevated. Chest X-ray was within normal limits. X-ray of forearm with wrist showed an oval expansile cystic lesion located eccentrically in the metaphysis of the left distal radius [Table/Fig-1a,b]. It had a dimension of 2cmx3cm with thinning of the overlying cortex and without any marginal sclerosis. The bone was osteopenic around the lesion. MRI was not done as the patient could not be sedated. Previously, FNAC was done outside and it was suggestive of granulomatous lesion but the slides were not available for re-evaluation.
(a&b) Pre-operative radiographs of forearm showing a cystic lesion in distal metaphysis of radius with perilesional osteopenia, without any apparent marginal sclerosis. (c&d) Postoperative radiographs taken 3 weeks and 4 months after surgery respectively showing gradual healing.

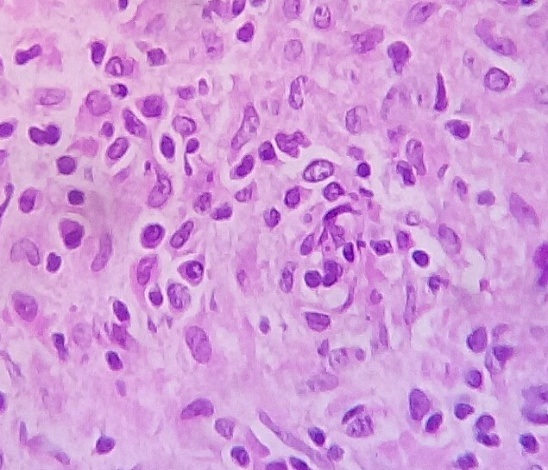
An open biopsy was performed under general anaesthesia and under tourniquet control. A cortical window at distal radius was made through a volar approach and caseous material was found. Thorough curettage of the lesion was done and collected samples were sent for investigations. The irrigated cavity was then filled with synthetic bone substitute (beta tricalcium phosphate granules). The wrist and forearm were immobilized with an above elbow back slab, which was removed subsequently at 4 weeks. The curetted material demonstrated acid fast bacilli and histopathological examination showed granulomatous inflammation, suggestive of tuberculosis [Table/Fig-2]. Anti-Tubercular Drugs (ATD) were started at thrice a week regime with oral paediatric doses according to Revised National Tuberculosis Control Program (RNTCP) guidelines. Isoniazid, Rifampicin, Pyrazinamide and Ethambutol were given in intensive phase for two months followed by Isoniazid and Rifampicin in continuation phase for 10 months. After 1 month a sinus with serous discharge was noted over the operative scar. Sample from the discharge was taken for culture studies and Co-amoxyclav suspension was started empirically. The culture report was negative and CRP was not elevated. Co-amoxyclav was stopped and ATD was continued. The wound healed subsequently with regular dressing [Table/Fig-3]. Symptoms and appetite improved along with weight gain which was noticeable after few weeks of starting ATD. ESR decreased to 15 mm/hr after 4 weeks. Clinical examination for possible toxicity to ATD was done at regular interval. Radiological healing of the lesion was observed in subsequent follow-up of 7 months [Table/Fig-1c,d].
Section shows plenty of ill formed granulomas composed of clusters of epitheloid cells surrounded by lymphocytes and few multinucleated giant cells. (400X, H&E stain).
Postoperative clinical picture of the forearm showing healed sinus scar and apparent swelling over the radial aspect, 2 months after surgery.

Discussion
Osteoarticular Tuberculosis (OAT) which represents 11% to 15% of all cases of extrapulmonary TB [1]. may resemble various infective and neoplastic bone lesions leading to diagnostic difficulties [2]. Tubercular osteomyelitis involving long bones is a rare presentation of skeletal tuberculosis, compared to articular and spinal lesions. The myriad radiological presentations makes the diagnosis challenging. Isolated lesions are usually of four basic types: (a) cystic; (b) infiltrative; (c) focal erosions; and (d) spina ventosa [2]. Solitary cystic lesion of metaphysis, though commoner than the other varieties, is overall a rare lesion and only a few cases have been reported in literature. The age of presentation in our case was rare. After thorough review of literature, only a few reported cases were found, of which one was reported in a child of less than 1 year age. It was a case of sternal tuberculosis in an infant of 9 months age (Kato et al., 2000) [3]. In young children and infants, the lesion usually occurs as primary complex following direct haematogenous seeding in bone [4]. In older children, it occurs following reactivation and spread of bacilli from primary pulmonary focus [4]. During postpartum period horizontal spread by droplet inhalation or ingestion from mother or undiagnosed family member is most commonly suggested mode of transmission [5]. Tuberculosis however is not transmitted through breast milk [6]. In this case droplet ingestion was the possible mode of transmission. The metaphysis of the long bones being highly vascular with sluggish flow are commonly affected. After lodging in the narrow terminal arteries TB bacilli grow, caseate and produce cystic lesion. In OAT the nature of the symptoms are subtle, so the diagnosis is difficult to make until the disease process is well advanced. A large number of patients in one series was treated initially with non-steroidal anti-inflammatory drugs, which falsely improved symptoms, leading to delayed diagnosis.
Rasool et al., retrospectively studied 53 children for primary osseous lesions of TB between 1989 and 2007 [2]. He showed a series of 13 children of 1 year to 13 year age group with histologically confirmed cystic tuberculosis mostly in the metaphysis of long bones [2]. Ten had solitary cystic lesions and 3 had the multi-cystic form. In his study, the lesions were radiolucent, round or oval with variable marginal sclerosis resembling subacute and chronic osteomyelitis. They also resembled simple and aneurysmal bone cysts, cartilaginous tumours, osteoid osteoma, granulomatous lesions, haematological disease and certain malignant tumours [2]. Only 2 of the children had pulmonary tuberculosis. The lesion in tubercular osteomyelitis may extend to involve the cortex and may break through it. The physis is no barrier to spread as lesions may extend into the epiphysis and may resemble chondroblastoma. Sequestra are uncommon and smaller than in pyogenic infection. The diagnosis of osteoarticular tuberculosis requires a high index of suspicion. Tuberculosis must be confirmed histologically [2]. Anti-tubercular therapy is the principal modality of treatment with favourable response in 85% cases when given for a period of 9 months to one year [7]. In suspected bony tubercular lesion in the proximity of a joint, biopsy from bony lesion is suggested rather than only a synovial biopsy. Curettage at the time of biopsy has been reported to yield favourable results as tubercle bacilli sequestrated in necrotic tissue found in cystic lesions and bone defects are inaccessible to chemotherapeutic agents [2]. Favourable outcome was achieved with artificial bone graft. Controversy exists regarding the use of bone graft after curettage of a large lesion [2]. Very few studies exist regarding usage of synthetic bone substitute in this age group. Good clinical recovery and resolution of the lesion was achieved and it support the results of the study done by Rasool et al., [2].
Conclusion
Tuberculous osteomyelitis presenting as cystic lesion in the long bone is unusual in an infant of 9 months age. Diagnosis requires high index of suspicion owing to its varied presentations especially in an endemic country like India. Open biopsy is often required when diagnosis remains elusive. Curettage and bone grafting followed by ATD therapy yields good result.
[1]. Lemnouer A, Frikh M, Belfquih B, Jaafar A, Bouya A, Jidal M, Navicular tuberculosis: A rare localization of bone tuberculosisIDCases [Internet] 2015 2(3)Elsevier Ltd:80-82.Available from: http://linkinghub.elsevier.com/retrieve/pii/S2214250915000207 [Google Scholar]
[2]. Rasool MN, Orth FCS, Tuberculosis – the masquerader of bone lesions in children Reprint requests : Table I 2009 :21-25.Available from: http://www.scielo.org.za/scielo.php?script=sci_arttext&pid=S1681-150X2009000100004&lng=en&nrm=iso&tlng=en [Google Scholar]
[3]. Kato Y, Horikawa Y, Nishimura Y, Shimoda H, Shigeto E, Ueda K, Sternal tuberculosis in a 9-month-old infant after BCG vaccinationActa Paediatr Int J Paediatr [Internet] 2000 89(12):1495-97.Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L32044196\nhttp://dx [Google Scholar]
[4]. Agarwal A, Khan SA, Qureshi NA, Multifocal osteoarticular tuberculosis in childrenJ Orthop Surg (Hong Kong) [Internet] 2011 19(3):336-40.Available from: http://www.ncbi.nlm.nih.gov/pubmed/22184166 [Google Scholar]
[5]. Mittal H, Das S, Faridi MMA, Management of newborn infant born to mother suffering from tuberculosis: Current recommendations & gaps in knowledgeIndian J Med Res [Internet] 2014 140:32-39.Available from: http://www.ncbi.nlm.nih.gov/pubmed/25222775 [Google Scholar]
[6]. Adhikari M, Jeena P, Bobat R, Archary M, Naidoo K, Coutsoudis A, HIV-Associated Tuberculosis in the Newborn and Young InfantInt J Pediatr [Internet] 2011 2011:354208Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3083848&tool=pmcentrez&rendertype=abstract [Google Scholar]
[7]. Malik S, Joshi S, Tank JS, Cystic bone tuberculosis in children - A case seriesIndian J Tuberc 2009 56 [Internet]2009;3(2):220–24. Available from: http://imsear.hellis.org/handle/123456789/146825 [Google Scholar]