Lymph Node Fibrosis in a Case of Primary Lymphoedema- A Report of Two Cases
Smitha Surendra Masamatti1, Aparna Narasimha2, Jayalakshmi Valligari Janardhan3, Vijaya Chowdappa4
1 Assistant Professor, Department of Pathology, Sapthagiri Medical College and Hospital, Bangalore, Karnataka, India.
2 Professor, Department of Pathology, Sapthagiri Medical College and Hospital, Bangalore, Karnataka, India.
3 Tutor, Department of Pathology, Sapthagiri Medical College and Hospital, Bangalore, Karnataka, India.
4 Head of the Department, Department of Pathology, Sapthagiri Medical College and Hospital, Bangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aparna Narasimha, No.22, Moyenvilla, Moyenville Road, Langford Town, Bangalore-560025, Karnataka, India.
E-mail: Sonrichie14@gmail.com
Lymphoedema can be classified into primary and secondary. Primary lymphoedema arise in patients where the cause is not known. Secondary lymphoedema are those in which the lymph system has been damaged by some well recognised pathological process, such as extensive malignancy, filariasis, radiation etc. The changes may occur either in the lymph node, or in lymph vessels or both. The clinical evolution and the prognosis of the oedema in the limb involved will depend on the extension and evolution of these lesions. The degree of fibrosis and its distribution in lymph node play an important role on the prognosis, clinical course and treatment of the patient. Hence pathologist should be aware of the microscopic distribution and patterns of lymph node fibrosis in primary lymphoedema. We hereby report two cases- a 50-year-old male diabetic patient and a 35-year-old male patient presenting with varicose veins, lymphoedema showing lymph node fibrosis.
Lymphodema, Lymph node fibrosis, Varicose veins
Case Report
Case 1: A 50-year-old male, diabetic since 8 years on oral hypoglycaemic agents presented with marked swelling of left lower limb along with pain since past 3 years. Examination revealed grade IV left lower limb oedema, along with dilated varicose veins. Left sided inguinal lymphnodes were enlarged, mobile, firm and non tender. All routine investigations were within normal limits. The color Doppler revealed incompetent Saphenofemoral (SF) junction along with tortuous, enlarged great saphenous vein with multiple varicosities. The SF junction and multiple perforators’ were ligated. Due to tissue oedema, the varicose vein could not be stripped off. The inguinal lymph nodes were excised and sent for histopathological examination.
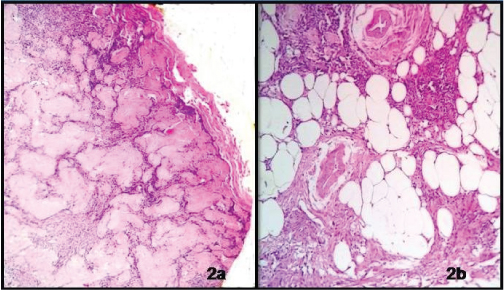
On Gross examination, two nodular grey tan masses were presented, larger measuring 2x2x1 cm and smaller measuring 1.5x1x0.5 cm. Cut surface of both the masses showed homogenous grey white appearance [Table/Fig-1]. On Microscopic examination, the lymph nodes showed pericortical fibrosis. The cortex and medulla showed depletion of lymphoid cells and were replaced by dense masses of hyaline fibrosis. The medulla also showed areas of lipomatosis [Table/Fig-2a&b].
Gross picture of both lymph nodes. Cut surface of the lymphnodes show homogenous grey white appearance.

Microphotograph showing: a) Cortex and medulla with depletion of lymphoid cells and are replaced by dense masses of hyaline fibrosis (H&E,X40) b) The medulla also shows focal areas of lipomatosis (H&E,X100).
Case 2: A 35-year-old male patient presented with swelling of right lower limb with varicosities since one and half years, with no significant past medical history. On examination, along with varicosities he had enlarged right inguinal lymph node. His color Doppler revealed SF junction incompetence along with enlarged, tortuous right saphenous vein, few of the veins showed filling defect with non compressive lumens, suggestive of superficial thrombosis and also revealed increased skin thickness suggestive of cellulitis. The perforators were ligated and even in this case, the vein couldn’t be stripped out due to oedema. Lymphnode was excised and sent for histopathology examination.
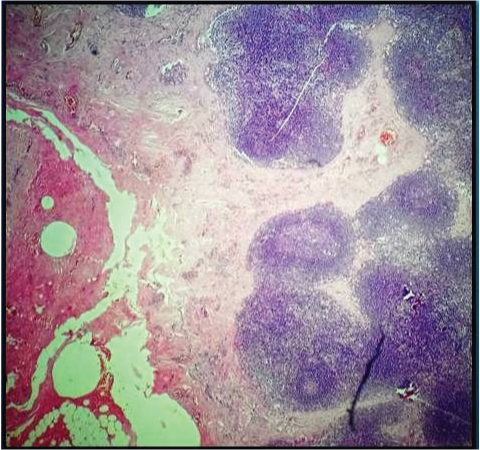
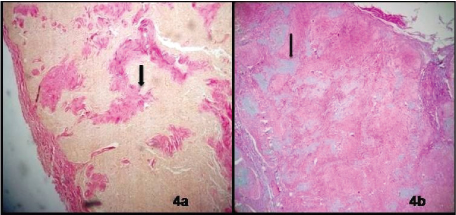
Gross examination revealed a single nodular mass measuring 0.5x 0.5x0.2cm. Cut surface showed grey tan appearance. On microscopic examination increased pericortical fibrosis was noted, along with bands of fibrosis extending from capsule into cortex and Medulla [Table/Fig-3]. Cortex showed many lymphoid follicles with prominent germinal centres. Focal hyalinization was noted in few follicles. The amount of fibrosis was less as compared with previous case. All the findings were consistent with effects of cellulitis in lymphnode which were described in the literature. A final diagnosis of fibrosing lymphadenitis was offered in both the cases. Areas of fibrosis were demonstrated by Masson’s trichrome stain and Van Gieson stain [Table/Fig-4a&b]. Special stain like Congo red was performed to rule out amyloid deposition in both the cases. In the first case, there was extensive degree of fibrosis whereas in second case the fibrosis was restricted to the pericortical areas and was moderate. Both the patients were lost for follow up and hence the prognosis couldn’t be assessed in either.
Microphotograph of lymph node of second case showing increased pericapsular fibrosis (H&E,X40).
Microphotograph showing areas of fibrosis: a) Masson’s trichrome stain (MT,X40); b) Van Gieson stain (VG,X40).
Discussion
Lymphoedema is accumulation of water and proteins in tissues. This may be associated with structural changes in the affected tissues such as skin, lymphatics and lymph nodes. Several studies have documented fibrosis occurring either in the lymph node, lymph vessels or both [1].
The early lymphographic studies of primary lymphoedema probably laid undue emphasis on changes in the lymph nodes and lymphatics. Previous studies suggest that in many patients with primary lymphoedema, the pathological process arises first in the nodes as the majority of the histopathological changes were worse in lymph nodes [2]. The basic pathogenesis for lymphoedema is that the filtration capacity and processing capabilities of the affected lymph node are altered [3].
Kinmoth classified lymphoedema based on radiographic abnormalities as ‘aplasia’, ‘hypoplasia’ and ‘hyperplasia’ [2]. The amount of fibrosis varies in these different clinical and lymphographic groups. It is more in proximal hypoplasia and bilateral hypoplasia patients while it is less in case of distal hypoplasia. The cause of fibrosis remains unknown however the probable hypothesis as stated by Kinmonth et al., suggested that even minor degrees of pathological changes in lymph node may increase the normal resistance to lymphatic flow [4]. And patients with lymph node fibrosis usually have family history, congenital onset of disease and non lymphatic congenital anomalies. Hence the clinical features suggest that the fibrotic process and tendency to oedema are due to genetic or familial defect. In minority of the cases, mild trauma or inflammation leads to fibrosis in lymphnodes. In first case, congenital defect in lymphatics may be the cause for fibrosis and in the second case, patient had associated cellulitis, hence that could be the probable reason. Fibrosis also depends on the duration of the disease, i.e., it was more evident in patients with a short history of lymphoedema [4].
Grossly the affected lymph nodes may be of normal size or enlarged or even atrophic. Senile changes include involution of lymphoid tissue and fibrolipomatosis [5]. In many lymph nodes, the normal architecture was lost, reticular fibres become fragmented; lymphoid elements were depleted, and replaced by fibroblasts, increased pericortical fibrosis, few active germinal centres, dense areas of fibrosis, fibrosclerosis, fatty infiltration, hyalinization, giganto cellular response etc may also be seen. Various histopathological changes noted in lymph nodes by Kinmonth et al., and Rada et al., were also noted in our cases [4,6]. Lymph flow through such nodes is sluggish [1]. Rada et al., referred this process of fibrosis as “lympho nodal pseudo cirrhosis” [6]. In less affected nodes, the fibrosis appeared as a perivascular cuff associated with intimal proliferation of patent lymphatics. Pericortical fibrosis was seen in patients with history of cellulitis which was also seen in our case. Fibrin is a potent stimulus for fibrosis but no interstitial deposition of fibrin was noted in our cases [4].
Mowlem in 1948 suggested that lymph node obstruction was the cause of primary lymphoedema but had no lymphographic or other supportive evidence. But recently the possibility of a primary lymph node abnormality has been reconsidered [7]. Hence it is advisable to correlate microscopic findings along with lymphoscintigrams to provide us with clue regarding advancement of the disease. This may be helpful in guiding the clinician to devise an appropriate treatment plan.
Apart from lymph node changes, skin and lymph vessel also show various histological changes. The changes in lymph vessel are, intimal proliferation, muscle hypertrophy, subintimal fibrohyalinosis etc. The changes occurring in skin included hyperkeratosis, fibrosis, lymphatic lakes, dilated capillaries, increased langerhans cells etc. Infact these changes noted in the lymph vessel and skin are attributed to the fibrosis in the lymph node [1].
The differential diagnosis include proteinaceous lymphadenopathy like amyloidosis, IgG4- related sclerosing disease, HIV infection, age dependant lymph node sclerosis, systemic sclerosis, rheumatoid arthritis, Hodgkins lymphoma etc [8–10].
Conclusion
Patients with primary lymphoedema may show marked fibrosis in lymph nodes. The main pathology of primary lymphoedema lies chiefly in the lymph nodes. Lymph node biopsies should not be undertaken routinely, as it damages the collaterals. It should be differentiated from other causes of sclerosis in lymph nodes. The degree of fibrosis and their distributions have important bearings on the prognosis, clinical course and treatment of the patient.
[1]. Olszewski WL, Kruszewski S, Zgliczynski L, Observations on movements of lymph vessels in patients with lymphadema of limbsPol Tyg Lek 1968 23:1345-47. [Google Scholar]
[2]. Kinmonth JB, Eustace PW, Lymph nodes and vessels in primary lymphoedema. Their relative importance in aetiologyAnnals of the royal college of surgeons of England 1976 58:278-84. [Google Scholar]
[3]. Rada O, Russo I, Pathogenesis of primary lymphoedemasRev chir Oncol radiol O R L oftamol stomatol chir 1979 28(6):419-24. [Google Scholar]
[4]. Kinmonth JB, Wolfe JH, Fibrosis in the lymph nodes in primary lymphoedema. Histological and clinical studies in 74 patients with lower limb oedemaAnnals of the royal college of surgeons of England 1980 62:344-54. [Google Scholar]
[5]. Hadamitzky C, Spohr H, Debertin AS, Guddat S, Tsokos M, Pabst R, Age dependent histoarchitectural changes in human lymph nodes: an underestimated process with clinical relevance?Journal of anatomy 2010 216:556-62. [Google Scholar]
[6]. Rada IO, Tudose N, Roxin BR, Lympho nodal fibrosclerosis in primary lymphoedema. Considerations on lympho nodal fibrosclerosis in primary lymphoedema. Part oneLymphology 1983 [Google Scholar]
[7]. Mowlem R, The Surgical correction of chronic lymphaoedema of legBrit J plastic Surg 1948 1:48 [Google Scholar]
[8]. McCluggage WG, Barucha H, Lymph node hyalinisation in rheumatoid arthritis and systemic sclerosisJournal of clinical pathology 1994 47:138-42. [Google Scholar]
[9]. Grimm KE, Barry TS, Chizhevsky V, Anslem Hii, Weiss LM, Siddiqi IN, Histopathological findings in 29 lymph node biopsies with increased IgG4 plasma cellsModern pathology 2012 25:480-91. [Google Scholar]
[10]. Ioachim HL, Medeiros LJ, Proteinaceous lymphadenopathy, In: Jonathan pine, edLymph node pathology 2009 4th edPhiladelphiaLippincott Williams and Wilkins:266-69. [Google Scholar]