Steroid Cell Tumour of Ovary – A Rare Case Report
Ranjeev Bhagat1, Vijay Kumar Bodal2, Nishit Gupta3, Pooja Garg4
1 Assistant Professor, Department of Pathology, Government Medical College and Hospital, Chandigarh, India.
2 Associate Professor, Department of Pathology, Government Medical College, Patiala, Punjab, India.
3 Junior Resident, Department of Pathology, Government Medical College, Patiala, Punjab, India.
4 Junior Resident, Department of Pathology, Government Medical College, Patiala, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ranjeev Bhagat, 224 Phase 11 Sec 65 Mohali-160062, Punjab, India.
E-mail: ranjeevbhagat@gmail.com
Steroid cell tumours of the ovary are uncommon sex- hormone secreting tumours characterized by a steroid cell proliferation. The incidence of steroid cell tumour of the ovary is only 0.1% of all ovarian tumours. As far as steroid cell tumours, not otherwise specified (NOS) is concerned; it constitutes about 56% of all steroid cell tumours. Here we present a case of 55-year-old, postmenopausal patient who presented with complaints of bleeding per vaginum and abdominal pain for last 3-4 months, with history of excessive hair growth since 3-4 years. Ultrasonography revealed a solid right ovarian mass with a possibility of ovarian sex cord tumour. Histopathology confirmed the diagnosis of steroid cell tumour NOS type with no cytological atypia.
Adnexal mass, Androgenic, Post-menopausal
Case Report
A 55-year-old postmenopausal lady presented with complaints of bleeding per vaginum and lower abdominal pain for the last 3-4 months. She also had increased body hair for last 3-4 years. She had three children and there was no history of any abnormality during her pregnancy. There was no history of any contraception and exogenous hormone intake.
Past medical history was otherwise unremarkable. Family history was noncontributory. Ultrasonography revealed a hypoechoic right adenexal mass measuring 65x40x30mm. This mass was not separated from right ovary. A possibility of ovarian sex cord tumour was given. A total hysterectomy with bilateral salpingo-oophorectomy was done and the specimen was received in our department for histopathological examination.
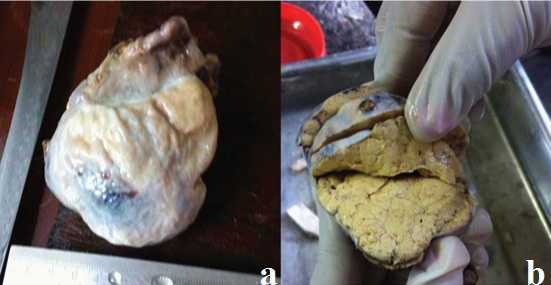
An already cut open gross specimen of uterus was received measuring 9x6x3.5cm in size with one tube and ovary and other fallopian tube and ovary lying separately in container. Ovarian tumour measured 6x4x3cm. It was replacing whole of the ovary without any peripheral ovarian stroma. Cut surface was solid and yellow in colour [Table/Fig-1a&b]. Other side ovary was grossly normal. Specimen of omentum measuring 45cm in length was also received.
(a) Showing grey-white tumor. (b) Showing yellow and lobulated cut surface.
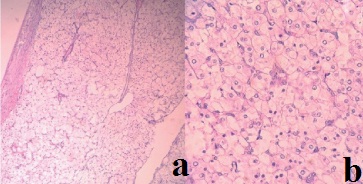
Sections from ovarian tumour showed well circumscribed tumour comprising of large round to polygonal cells with centrally placed nuclei, prominent nucleoli and abundant amount of eosinophilic cytoplasm [Table/Fig-2a&b]. There was no atypia, mitotic figures or necrosis noted in the tumour. Stroma was scanty. Histological features were consistent with steroid cell tumour NOS type. The cervix showed features of chronic cervicitis while the endometrium showed atrophic changes. The other side ovary and tube was unremarkable. Patient was discharged after 1 week with stable condition and was adviced follow up after 1 month. Patient’s excessive hair growth reduced after few months and there were no other complaints.
(a) Showing well circumscibed tumor wiyh scanty stroma (H&E,10X). (b) High power showing polygonal tumor cells with central nuclei, prominent nucleoli and abundant cytoplasm (H&E,40X).
Discussion
The incidence of steroid cell tumours, NOS is highest in women of child bearing age group, particularly during the third and fourth decades, but in rare cases postmenopausal women or children may also have this tumour. Androgenic manifestations are common in these tumours as they secrete hormones like androstenedione, α-hydroxyprogesterone, and testosterone [1,2].
These tumours are known to produce symptoms of virilisation particularly hirsutism. So in cases where there is unexplained hirsutism, ovarian and adrenal tumour association should be ruled out as there may be occult malignancies [3]. However, there may be atypical presentations of these tumours also when they do not show any symptoms of virilisation. In these cases the diagnosis is usually made postoperatively on finding a tumour in ovary [4].
These tumours have been divided into three subtypes according to their cells of origin: stromal luteoma, leydig cell tumour and steroid cell tumour, not otherwise specified (NOS). Of these subtypes, the steroid cell tumours, NOS account for about 56% of steroid cell tumours [5].
A majority of steroid cell tumour NOS are unilateral and well circumscribed. The size varies from 1.2 to 45 cm [6]. Grossly these tumours are commonly solid, however a combination of solid and cystic form or predominantly cystic form may also be seen. The color of the cut surface may range from yellow to orange to red or brown depending upon the lipid content. Area of haemorrhage and necrosis may also be seen [6]. The tumour in our case was completely solid with no cystic area. The cut surface was typically yellow and lobulated.
Steroid cell tumour, NOS should be differentiated from other two entities in the category of steroid cell tumours including stromal luteoma and leydig cell tumour. Stromal leutoma is usually located in the ovarian stroma. It frequently occurs in association with stromal hyperthecosis. Another feature which can help in diagnosing this tumour is presence of degenerative pseudovascular spaces containing red blood cells [7]. On the other hand, leydig cell tumour is usually present in hilar location. The tumour cells shows cytoplasmic reinke crystals and it is commonly associated with leydig cell hyperplasia [8]. Although pregnancy luteoma may sometimes resemble steroid cell tumour microscopically, however it is commonly multifocal and occurs bilaterally in approximately one-third of patients. It usually regresses after pregnancy [7,9]. In our case, there was no feature like stromal hyperthecosis, pseudovascular spaces or rceinke crystals to suggest the possibility of stromal luteoma and leydig cell tumour.
A clinicopathological correlation is very important in these tumours as the benign looking tumours on histomorphology can behave in a clinical malignant manner [10]. As far as immunohistochemical markers are concerned, inhibin is quite useful in differentiating this tumour from other non sex cord tumours [11].
The treatment of these tumours should be based on the histological picture, surgical staging and patient’s desire to preserve fertility [10,12]. In young patient who want to preserve their fertility, unilateral salpingo-oophorectomy is the preferred method of treatment [13]. In our case, as the patient was postmenopausal, a total abdominal hysterectomy with bilateral salpingo-ophorectomy was done. There are certain clinicopathologic parameters which correlate with adverse behaviour of the tumour like older age at the time of presentation, size of the tumour more than 7.0 cm, mitosis more than 2/10HPFs, grade 2–3 nuclear atypia, necrosis, and haemorrhage [4]. Our case had a good prognosis as the size was less than 7 cm, there were occasional mitotic figure and there was absence of necrosis also.
Conclusion
Steroid cell tumours, Not Otherwise Specified (NOS), are rare ovarian sex cord-stromal tumours which are usually associated with various virilizing symptoms like hirsutism and amenorrhea. The typical clinical, radiological and histopathological findings can clinch the diagnosis in most of the cases however in difficult cases, immunohistochemistry can be useful.
[1]. Outwater EK, Wagner BJ, Mannion C, McLarney JK, Kim B, Sex cord-stromal and steroid cell tumours of the ovaryRadiographics 1998 18(6):1523-46. [Google Scholar]
[2]. Cserepes E, Szucs N, Patkos P, Csapo Z, Molnar F, Toth M, Ovarian steroid cell tumour and a contralateral ovarian thecoma in a postmenopausal woman with severe hyperandrogenism. GynecolEndocrinol 2002 16(3):213-16. [Google Scholar]
[3]. Dinc G, Saygin I, Kart C, Mungan S, Guven S, SedaGuvendagGuven E, A rare case of postmenopausal severe virilization: Ovarian steroid cell tumour, not otherwise specifiedJ Cases Obstet Gynecol 2016 3(1):19-21. [Google Scholar]
[4]. Rubido Valle CD, Fuente de la JLC, Martinez CS, Calvo LN, Escarda MR, Ovarian Steroid Cell Tumour Associated to Endometrial Hyperplasia and Presenting as Postmenopausal Vaginal BleedingGynecol Obstet (Sunnyvale) 2015 5(9):316 [Google Scholar]
[5]. Baloglu A, Bezircioglu I, Cetinkaya B, Karci L, Bicer M, Development of secondary ovarian lesions after hysterectomy without oophorectomy versus unilateral oophorectomy for benign conditions: a retrospective analysis of patients during a nine-year period of observationClin Exp Obstet Gynecol 2010 37:299-302. [Google Scholar]
[6]. Hayes MC, Scully RE, Ovarian steroid cell tumours (not otherwise specified): A clinic-pathological analysis of 63 casesAm J Surg Pathol 1987 11(11):835-45. [Google Scholar]
[7]. Scully RE, Stromal luteoma of the ovary. A distinctive type of lipoid-cell tumourCancer 1964 17:769-78. [Google Scholar]
[8]. Paraskevas M, Scully RE, Hiluscell tumour of the ovary. A clinico-pathological analysis of 12 Reinke crystal-positive and nine crystal- negative casesInt J Gynecol Pathol 1989 8(4):299-310. [Google Scholar]
[9]. Clement PB, Tumour-like lesions of the ovary associated with pregnancyInt J Gynecol Pathol 1993 12(2):108-15. [Google Scholar]
[10]. Mehdi G, Ansari HA, Sherwani RK, Rahman K, Akhtar N, Ovarian Steroid Cell Tumour: Correlation of Histopathology with Clinico-pathologic FeaturesPathology Research International 2011 2011:9878955 pages, 2011 [Google Scholar]
[11]. Rabban JT, Zaloudek CJ, A practical approach to immune-histochemical diagnosis of ovarian germ cell tumours and sex cord-stromal tumoursHistopathology 2013 62:71-88. [Google Scholar]
[12]. Jiang W, Tao X, Fang F, Zhang S, Xu C, Benign and malignant ovarian steroid cell tumours, not otherwise specified: case studies, comparison, and review of the literatureJ Ovarian Res 2013 6:53 [Google Scholar]
[13]. Swain J, Sharma S, Prakash V, Agrawal NK, Singh SK, Steroid cell tumour: a rare cause of hirsutism in a femaleEndocrinology, diabetes and metabolism case reports 2013 2013:130030 [Google Scholar]