The choice of implant length is an essential factor in deciding the survival rates of these implants and the overall success of the prosthesis. Placing an implant in the posterior part of the maxilla and mandible has always been very critical due to poor bone quality and quantity. Long implants can be placed in association with complex surgical procedures such as sinus lift and bone augmentation. These techniques are associated with higher cost, increased treatment time and greater morbidity. Hence, there is need for a less invasive treatment option in areas of poor bone quantity and quality. Data related to survival rates of short implants, their design and prosthetic considerations has been compiled and structured in this manuscript with emphasis on the indications, advantages of short implants and critical biomechanical factors to be taken into consideration when choosing to place them. Studies have shown that comparable success rates can be achieved with short implants as those with long implants by decreasing the lateral forces to the prosthesis, eliminating cantilevers, increasing implant surface area and improving implant to abutment connection. Short implants can be considered as an effective treatment alternative in resorbed ridges. Short implants can be considered as a viable treatment option in atrophic ridge cases in order to avoid complex surgical procedures required to place long implants. With improvement in the implant surface geometry and surface texture, there is an increase in the bone implant contact area which provides a good primary stability during osseo-integration.
Introduction
The choice of implant length in relation to the available bone quality and quantity and biting force is a critical factor in the success of implants and longevity of the prosthesis. Long implants have always been considered more desirable in this respect but in patients with advanced alveolar bone resorption their placement is problematic due to the anatomic boundaries. Anatomical limitation in resorbed maxilla includes the maxillary sinus posteriorly and nasal floor and nasopalatine canal anteriorly whereas in resorbed mandible it is inferior alveolar canal. Advanced surgical procedures such as guided bone regeneration, block grafting, maxillary sinus floor grafting, distraction osteogenesis and nerve repositioning can be carried out to gain alveolar height in these areas and permit placement of long length implants but these techniques are sensitive, challenging, costly, time consuming and increase surgical morbidity. Short implants offer a less invasive treatment alternative in resorbed ridge cases [1–3]. There is no general consensus on the definition of short implant. Most of the authors have considered implants less than 10mm as short implants [4–6]. [Table/Fig-1] summarizes the studies conducted on short implants depicting their survival rates and comparison with long implants.
Studies comparing survival rates of long and short implants.
| Author | Year | Study |
|---|
| Wyatt et al., [7] | 1998 | Studied 77 patients with 230 machined implants with a follow-up of 12 years and found that cumulative survival rate of short implants was 75% whereas that of long implants was 95% |
| Bahat et al., [8] | 2000 | Found a high failure rate of 17% for 7mm and 8.5mm implants |
| Weng et al., [9] | 2003 | Conducted a study on 493 patients with 1179 implants with a follow-up of 72 months and found a cumulative survival rate of 74% with 7mm implants, 81% with 8.5mm implants and 93.1% with >10mm implants |
| Herrmann et al., [10] | 2005 | Conducted a multicenter analysis of 487 implants and found a 10.1% failure rate for 10mm implants and 21.8% failure rate for 7mm implants |
| Esposito et al., [1] | 2011 | Conducted a study on 60 patients comparing 6.3mm with 9.3mm implants associated with vertical augmentation procedure and found more complications with augmented patients and less bone loss, less time, less cost and less morbidity with short implants |
| Annibali et al., [11] | 2012 | Conducted a systematic review and meta-analysis and concluded that more long term follow-up results are required to support the use of short implants |
| Hassani et al., [12] | 2013 | Found initial post-operative sensory impairment to be the most common complication after inferior alveolar nerve transposition with 16% of patients left with a permanent and irreversible condition |
| Vasquez et al., [13] | 2014 | Documented complication rate in 200 sinus lift procedures and found that Schneiderian membrane perforation occurred in 25.7% of the cases |
| Al-Hashadi et al., [14] | 2014 | Concluded that there is sufficient evidence showing high success rates with short implants as compared to surgical augmentation procedures in the treatment of atrophic ridges |
| Nisandand Renouard [15] | 2014 | Reviewed studies on short implants and found similar survival rates and reduced treatment cost and time when compared to long implants assisted by advanced surgical procedures |
Advantages of Short Implants
Bone grafting to compensate for less height is unnecessary.
Less money, pain and time associated with various surgical procedures before placement of implant.
Complex surgical techniques are often associated with complications during surgery such as bleeding, perforation of the Schneiderian membrane or nerve injury and post-operatively such as transient or permanent alteration of mandibular sensation, graft and/or membrane exposure, infections and increased peri-implant bone loss. This can be avoided.
Osteotomy preparation is simplified since shorter bone preparation is required at the implant site which provides direct access for water irrigation and reduces the possibility of bone overheating.
Implant insertion is easier.
Angulation to load is improved with short osteotomy site since the basal bone beyond the original alveolar ridge is not always located in the long axis of the missing tooth.
Biomechanical Considerations
They have been categorized as follows
1. Diagnostic
a) Implant diameter: It is more efficient than implant length for dissipation of stresses, because the area receiving maximum effort is the bone crest and very little stress is transferred to the apical portion. An increased length would therefore only improve primary stability but wider implant would not only increase the primary stability but also the functional surface area at the crestal bone level leading to better distribution of occlusal forces. Finite element analysis has also supported this concept and demonstrated that implant length might not be the principal factor influencing transfer of occlusal loads to the bone-implant interface [16].
b) Crown/implant ratio: Increased crown/implant ratio can act as a vertical cantilever leading to crestal bone loss and implant failure. However, improvements of surfaces and implant systems along with proper force orientation and load distribution have allowed high crown/implant ratios to be applied with success.
c) Bone quality: It is the primary factor for short implant success [17]. Areas with type III and type IV bone show more failures regardless of the implant surface treatment. The combination of short implant length and poor bone quality reduces the implant stability during implant placement and the healing period.
d) Lack of cantilevers: A cantilever magnifies the forces directly proportional to the height of the crown. It creates six different potential rotation points on the implant body. Eliminating cantilevers favors biomechanics and increased treatment predictability.
e) Number of implants: Use of multiple implants will increase the functional surface area to resist occlusal forces.
f) Implant design: The implant surface area can be increased by [18]:
Thread number: More the number of threads per unit length in the same axial plane more is the implant surface area in contact with the bone.
Thread depth: Deeper threads provide more implant surface area.
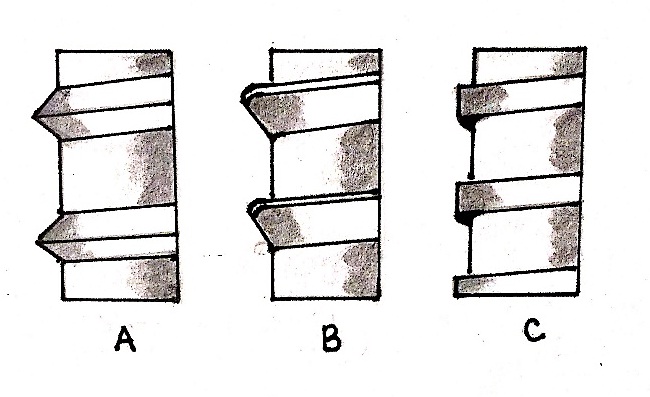
Thread shape: The square thread design has a higher bone-implant contact percent as compared to v-shape and reverse buttress thread designs [Table/Fig-2a-c].
Implant surface: As compared to turned smooth surface, rough microtopography of implant surface increases the bone-implant contact surface area and accelerates osseo-integration. It also compensates for inadequate crown/implant ratio.
a) V-thread b) Reverse thread c) Square thread.
2. Surgical
a) Two step surgical protocol: A two stage surgery is advocated for short implants as it provides good primary stability during healing phase. The time elapsed between the surgical and load stage should be 4-6months for maxilla and 2-4months for mandible [19].
b) Adapted surgical protocol: Enhanced initial implant stability can be achieved by eliminating a step in standard surgical protocol such as eliminating the countersink drill or eliminating the final drill in the standard drilling sequence [20]. Soft bone drilling protocol should be followed in poor quality bone whereas, the final bone drilling is done with narrow drills rather than standard size drills.
3. Prosthetic
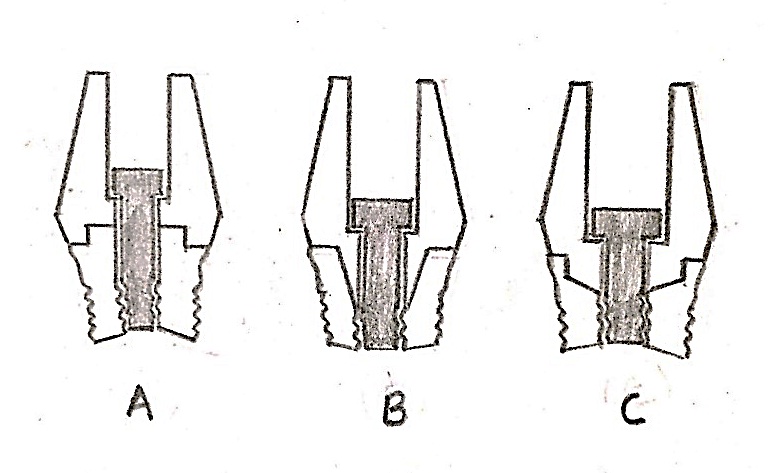
a) Implant to abutment connection: Morse taper connection induces less marginal bone loss as compared to external hex abutment connection and also promotes bone growth over the implant shoulder [21]. Internal hex implant abutment connection shows a wider force distribution as compared to external hex connection [22] [Table/Fig-3a-c]. Platform switching maintains the crestal bone for the entire length of the implant up to the collar level.
a) External hex b) Morse taper c) Internal hex.
b) Occlusal table: Small occlusal table reduces the offset loads on the implant.
c) Incisal guidance: Implants should follow a biomechanical approach similar to natural teeth to accommodate the higher bite forces in the posterior regions of the mouth. Incisal guidance of the anterior teeth eliminates lateral forces to the posterior teeth in all mandibular excursions.
d) Splinting: Splinting implants increases the functional surface area of support and transmits less force to the prosthesis, the cement, abutment screws and the implant bone interface especially when placed in soft bone.
Clinical Guidelines for Placing Short Implants
Nisand and Renourd in 2014 suggested guidelines for placement of short implants and other therapeutic options based on available bone height, bone quality and certain risk factors such as smoking, history of periodontal disease and advanced age [15]. These guidelines are summarized in [Table/Fig-4,5] and are applicable in the situations where residual ridge alveolar ridges are wide enough to permit the placement of at least 5mm diameter implant.
| Ridge height | Bone type | History of periodontitis, smokers, patient’s age | Treatment |
|---|
| <5mm | Type I, II, III | No | Sinus lift |
| Type IV | Yes | Sinus lift |
| 5-6mm | Type I, II, III | No | Short implants |
| Type IV | Yes | Sinus lift |
| ≥6mm | Type I, II, III | No | Short implants |
| Type IV | Yes | Short implants |
| Ridge height | Bone type | Treatment |
|---|
| <8mm | Type I, II, III, IV | Advanced surgical procedure |
| ≥8mm | Type I, II, III, IV | Short implants |
Indications for Short Implants: Short implants can be used in almost all types of replacements whether fixed or removable including:
Single and multiple fixed prosthesis in posterior jaw.
In the treatment of a severely resorbed edentulous mandible, with four short-length implants used to support an overdenture or six short implants used to support a fixed prosthesis.
In edentulous maxilla, two short-length implants are additionally placed in the distal area, together with longer implants in the premaxilla to support a maxillary overdenture or a fixed prosthesis.
Discussion
Himmlova et al., conducted finite element analysis to study stresses occurring at the bone-implant interface [16]. It was found that maximum stress concentration occurred near the crest portion of the implant surface i.e., at the top 5-6mm of the implant and there was little difference in the area affected by varying the implant lengths. Earlier implant supported prosthesis were given based on the rationale of optimum crown/implant ratio as implant was considered similar to the root of a tooth. This led to the placement of longest possible implants. But there is a vast difference in the attachment of root and implant to the alveolar bone. Root is attached via periodontal ligament whereas implant is in direct contact with the bone via osseo-integration.
Griffin and Cheung in 2004 recognized maximized implant surface area as the most contributing factor to the high success rate of short implants [23]. Hagi et al., in 2004 conducted a systematic review and concluded that implant surface geometry is a major determinant in the performance of short implants [24]. Fugazzotto et al., did not recommend the use of countersink for implant placement [20]. Gentile et al., in 2005 in their study found high survival rates with rough surface implants and two stage surgical protocol in implant placement [25]. Renouard and Nisand recommended the use of an adapted surgical protocol to enhance initial implant stability [26]. Routine surgical protocol usually involves a tapping procedure which reduces the initial primary stability of the implant.
Goene et al., found similar success rates of short implants with textured surface and standard length implants [27]. Misch advised splinting when using short implants for better load distribution due to direct contact between implant and surrounding alveolar bone [18]. It also compensates for unfavorable crown/implant ratio. Renourd and Nisand in 2006 conducted a review and found factors causing high failure rate associated with short implants were operator inexperience, following standard surgical preparation, use of machined surface implants and placement in areas of poor bone density [28]. Misch et al., analyzed short implants placed in maxilla and mandible’s posterior area and found that by applying the biomechanical properties of stress reduction i.e., adequate crown/implant ratio, number of implants similar to lost teeth, lack of cantilever, splinting and reduction of occlusal table, short implants presented a success rate of approx 99.2% [5].
Tawil et al., recommended the use of short implants under the conditions of favorable load distribution and controlled parafunctional habits [6]. Arlin in 2006 reported a success rate of 94% for moderately rough surface implants compared to <80% for machined surface implants [29]. Blanes et al., found in a 1- year follow-up study of patients with short implants that the survival rate was as high as 94.1% with a mean crown/implant ratio of 1.8 [30]. Anitua and Orive in 2010 reported positive results with short length implants when placed under strict clinical protocols [31]. Romeo et al., in 2010 conducted literature review and emphasized the significance of treatment planning on the successful rehabilitation of short implants [32]. Birdi et al., in their study did not find any relation between crown/implant ratio and initial bone to implant contact levels [33].
Telleman et al., in 2011 proposed that high failure rate of short implants was mainly because of less bone to implant contact, placement in areas of poor bone quality and high crown/implant ratio [34]. They conducted a systematic review and found a better prognosis of short implants in partially edentulous patients who are non- smokers. Sun et al., conducted a systematic review to study the parameters responsible for failure of short implants such as implant length, implant position, implant surface and surgical protocol and found that the most critical factors were poor bone quality and machined surface of the implants [35]. Yilmaz et al., compared splinted prosthesis with non-splinted prosthesis and found more favorable load distribution with the former as compared to the latter [36].
Mijiritsky et al., in 2013 found in their study that there is no correlation between the survival rate of implants and implant length and diameter and found high success rates of short and narrow implants in partially edentulous patients [37]. In a study by Anitua et al., in 2013 no relation was found between crown/implant ratio and mean bone level [38]. Implant diameter is more effective in stress distribution than implant length and implant geometry. Thoma et al., advised placement of short implants in atrophied posterior maxilla as they reduce patient morbidity, treatment time and overall cost [39]. Gonclaves et al., emphasized the importance of factors such as patient’s habits, presence of systemic diseases, features related to implant insertion, characteristics of the implants, particularities of the prosthesis and biological parameters when placing short implants [40].
Conclusion
The use of short-length implants allows treatment of patients who are unable to undergo complex surgical techniques for medical, anatomic or financial reasons. By reducing the need for complex surgeries short implants reduce morbidity, cost and treatment time. When placed considering all the critical biomechanical factors and using strict clinical protocol short implants can be a successful treatment option in atrophic ridges. However, there is still a dearth of data on the prospective long-term success and survival of these short implants, particularly with respect to occlusal loading, crown/implant ratio, and insituations of less than optimal bone quality.
[1]. Esposito M, Cannizarro G, Soardi E, Pellegrino G, Pistilli R, Felice P, A 3-year post-loading report of a randomized controlled trial on the rehabilitation of posterior atrophicmandibles: Short implants or longer implants in vertically augmented bone?Eur J Oral Implantol 2011 4:301-11. [Google Scholar]
[2]. Felice P, Soardi E, Pellegrino G, Pistilli R, Marchetti C, Gessaroli M, Treatment of the atrophic edentulous maxilla: short implants versus bone augmentation for placing longer implants: Five-month post-loading results of a pilot randomised controlled trialEur J Oral Implantol 2011 4:191-202. [Google Scholar]
[3]. Neves FD, Fones D, Bernardes SR, Prado CJ, Neto AJ, Short implants: an analysis of longitudinal studiesInt J Oral Maxillofac Implants 2006 21:86-93. [Google Scholar]
[4]. Barboza E, Carvalho W, Francisco B, Ferreira V, Desempenhoclínico dos implantescurtos: um estudoretrospectivo de seisanosR Periodontia 2007 17:98-103. [Google Scholar]
[5]. Misch CE, Steignga J, Barboza E, Misch Dietsh F, Cianciola LJ, Kazor C, Short dental implants in posterior partial edentulism: a multicenter retrospective 6-year case series studyJ Periodontol 2006 77:1340-47. [Google Scholar]
[6]. Tawil G, Aboujaoude N, Younan R, Influence of prosthetic parameters on the survival and complication rates of short implantsInt J Oral Maxillofac Implants 2006 21:275-82. [Google Scholar]
[7]. Wyatt CC, Zarb GA, Treatment outcomes of patients with implant-supported fixed partial prosthesesInt J Oral Maxillofac Implants 1998 13:204-11. [Google Scholar]
[8]. Bahat O, Branemark system implants in the posterior maxilla: clinical study of 660 implants followed for 5 to 12 yearsInt J Oral Maxillofac Implants 2000 15:646-53. [Google Scholar]
[9]. Weng D, Jacobson Z, Tarnow D, Hürzeler MB, Faehn O, Sanavi F, A prospective multicenter clinical trial of 3i machined-surfaced implants: results after 6 years of follow-upInt J Oral Maxillofac Implants 2003 18:417-23. [Google Scholar]
[10]. Herrmann I, Lekholm U, Holm S, Kultje C, Evaluation of patient and implant characteristics as potential prognostic factors for oral implant failuresInt J Oral Maxillofac Implants 2005 20:220-30. [Google Scholar]
[11]. Annibali S, Cristalli MP, Dell’Aquila D, Bignozzi I, La Monaca G, Pilloni A, Short dental implants: a systematic reviewJ Dent Res 2012 91:25-32. [Google Scholar]
[12]. Hassani A, Motamedi M, Saadat S, Inferior alveolar nerve transpositioning for implant placement, a textbook of advanced oral and maxillofacial surgery 2013 Rijeka, CroatiaIn Tech Publishing [Google Scholar]
[13]. Vasquez JCM, Rivera ASG, Gil HS, Mifsut RS, Complication rate in 200 consecutive sinus lift procedures: guidelines for prevention and treatmentJ Oral Maxillofac Surg 2014 72:892-901. [Google Scholar]
[14]. Al-Hashdi AA, Taiyeb Ali TB, Yunus N, Short dental implants: an emerging concept in implant treatmentQuintessence Int 2014 45:499-514. [Google Scholar]
[15]. Nisand D, Renouard F, Short implant in limited bone volumePeriodontal 2000 2014 66:72-96. [Google Scholar]
[16]. Himmlova L, Dostalova T, Kacovsky A, Konvickova S, Influence of implant length and diameter on stress distribution: A finite element analysisJ Prosthet Dent 2004 91:20-25. [Google Scholar]
[17]. Tawil G, Younan R, Clinical evaluation of short, machined-surface implants followed for 12 to 92 monthsInt J Oral Maxillofac Implants 2003 18:894-901. [Google Scholar]
[18]. Misch CE, Short dental implants: a literature review and rationale for useDent Today 2005 24:64-68. [Google Scholar]
[19]. Galvao FFSA, Almeida-Junior AA, Faria-Junior NB, Caldas SGFR, Reis JMSN, Margonar R, Predictability of short dental implants: A literature reviewRSBO 2011 8:74-80. [Google Scholar]
[20]. Fugazzotto PA, Beagle JR, Ganeles J, Jaffin R, Vlassis J, Kumar A, Success and failure rates of 9mm or shorter implants in the replacement of missing maxillary molars when restored with individual crowns: preliminary results 0- 84 months in function. A retrospective studyJ Periodontol 2004 75:327-32. [Google Scholar]
[21]. Castro DS, Araujo MA, Benfatti CA, Araujo Cdos R, Piattelli A, Perrotti V, Comparative histological and histomorphometrical evaluation of marginal bone resorption around external hexagon and Morse cone implants: an experimental study in dogsImplant Dent 2014 23:270-76. [Google Scholar]
[22]. Maeda Y, Satoh T, Sogo M, In vitro differences of stress concentrations: a short communicationJ Oral Rehabil 2006 33(1):75-78. [Google Scholar]
[23]. Griffin TJ, Cheung WS, The use of short, wide implants in posterior areas with reduced bone height: A retrospective investigationJ Prosthet Dent 2004 92:139-44. [Google Scholar]
[24]. Hagi D, Deporter DA, Pilliar RM, Arenovich T, A targeted review of study outcomes with short (≤7mm) endosseous dental implants placed in partially edentulous patientsJ Periodontol 2004 75:798-804. [Google Scholar]
[25]. Gentile MA, Chuang SK, Dodson TB, Survival estimates and risk factors for failure with 6x5.7mm implantsInt J Oral Maxillofac Implants 2005 20:930-37. [Google Scholar]
[26]. Renouard F, Nisand D, Short implants in the severely resorbed maxilla: a 2- year retrospective clinical studyClin Implant Dent Relat Res 2005 7:104-10. [Google Scholar]
[27]. Goené R, Bianchesi C, Hüerzeler M, Del Lupo R, Testori T, Davarpanah M, Performance of short implants in partial restorations: 3-year follow-up of osseotite implantsImplant Dent 2005 14:274-78. [Google Scholar]
[28]. Renouard F, Nisand D, Impact of implant length and diameter on survival ratesClin Oral Implants Res 2006 17:35-51. [Google Scholar]
[29]. Arlin ML, Short dental implants as a treatment option: results from an observational study in a single private practiceInt J Oral Maxillofac Implants 2006 21:769-76. [Google Scholar]
[30]. Blanes RJ, Bernard JP, Blanes ZM, Belser UC, A 10-year prospective study of ITI dental implants placed in the posterior region II: Influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone lossClin Oral Implants Res 2007 18:707-14. [Google Scholar]
[31]. Anitua E, Orive G, Short implants in maxillae and mandibles: a retrospective study with 1 to 8 years of follow-upJ Periodontol 2010 81:819-26. [Google Scholar]
[32]. Romeo E, Bivio A, Mosca D, Scanferla M, Ghisolfi M, Storelli S, The use of short dental implants in clinical practice: literature reviewMinerva Stomatol 2010 59:23-31. [Google Scholar]
[33]. Birdi H, Schulte J, Kovacs A, Weed M, Chuang SK, Crown to implant ratios of short length implantsJ Oral Implantol 2010 36:425-33. [Google Scholar]
[34]. Telleman G, Raghoebar GM, Vissink A, den Hartog L, Huddleston Slater JJ, Meijer HJ, A systematic review of the prognosis of short (<10 mm) dental implants placed in the partially edentulous patientJ Clin Periodontol 2011 38:667-76. [Google Scholar]
[35]. Sun HL, Huang C, Wu YR, Shi B, Failure rates of short (≤10mm) dental implants and factors influencing their failure: a systematic reviewInt J Oral Maxillofac Implants 2011 26:816-25. [Google Scholar]
[36]. Yilmaz B, Seidt JD, McGlumphy EA, Clelland NL, Comparison of strains for splinted and non- splinted screw- retained prosthesis on short implantsInt J Oral Maxillofac Implants 2011 26:1176-82. [Google Scholar]
[37]. Mijiritsky E, Mazor Z, Lorian A, Levin L, Implant diameter and length influence on survival: interim results during the first 2 years of function of implants by a single manufacturerImplant Dent 2013 22:394-98. [Google Scholar]
[38]. Anitua E, Pinas L, Orive G, Retrospective study of short and extra short implants placed in posterior regions: Influence of crown to implant ratio on marginal bone lossClin Implant Dent Relat Res 2015 17:102-10. [Google Scholar]
[39]. Thoma DS, Haas R, Tutak M, Garefa A, Schincaglia GP, Hammerle CHE, Randomized controlled multicentre study comparing short dental implants (6mm) versus longer dental implants (11-15mm) in combination with sinus floor elevation proceduresJ Clin Periodontol 2015 42:72-80. [Google Scholar]
[40]. Gonçalves TM, Bortolini S, Martinolli M, Alfenas BF, Peruzzo DC, Natali A, Long-term short implants performance: systematic review and meta- analysis of the essential assessment parametersBraz Dent J 2015 26:325-36. [Google Scholar]