Left Pulmonary Agenesis with Right Lung Bronchiectasis in an Adult
Prabhat Kumar1, Ghazal Tansir2, Gargi Sasmal3, Juhi Dixit4, Ratnakar Sahoo5
1 Senior Resident, Department of Medicine, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
2 Postgraduate Resident, Department of Medicine, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
3 Postgraduate Resident, Department of Medicine, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
4 Postgraduate Resident, Department of Medicine, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
5 Professor, Department of Medicine, PGIMER and Dr. Ram Manohar Lohia Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Prabhat Kumar, Senior Resident, Department of Medicine, OPD Block, PGIMER and Ram Manohar Lohia Hospital, New Delhi-110001, India.
E-mail: drkumar.prabhat@gmail.com
Pulmonary agenesis is a rare congenital anomaly characterized by the absence of pulmonary parenchyma and vasculature. Bilateral pulmonary agenesis is incompatible with extrauterine life. Unilateral agenesis is often associated with other congenital cardiovascular, genitourinary and gastrointestinal malformations. Right lung agenesis is more frequently associated with congenital anomalies and has poor prognosis as compared to left lung agenesis. Diagnosis is often made in childhood but can be delayed, if the clinician is not aware about this entity. Chest radiograph in unilateral lung agenesis shows opaque hemithorax and these patients are often confused with other common causes of opaque hemithorax like collapse, pleural effusion and diaphragmatic hernia. We report a case of left lung agenesis with right lung bronchiectasis in a middle-aged adult who was treated for tuberculous pleural effusion and was referred to our institute for persistent symptoms despite treatment.
Cor-pulmonale, Opaque hemithorax, Respiratory failure
Case Report
A 40-year old lady presented to us with the chief complaint of gradually progressive shortness of breath for one year, with increased severity over the past four months. This complaint was accompanied by development of intermittent swelling over both lower limbs for one year. She also had fever and productive cough for 7 days. The fever was continuous, not associated with chills and rigors and was relieved with antipyretic medications. Her cough was associated with production of non-foul smelling, mucopurulent sputum. There was no history of hemoptysis, chest pain, palpitations, urinary complaints, pain abdomen or jaundice.
She reported occurrence of such episodes of fever and cough in the past since her childhood for which she had taken over the counter medication multiple times. She also gave history of being treated for tuberculosis 15 years back by a private practitioner. Multiple attempts of pleural fluid tapping had been made during that period, and despite no fluid being aspirated, she was given 9 months of anti-tubercular treatment empirically. However, no documents were available. Her symptoms had aggravated for last 4 months and she was again started on anti-tubercular medications by a local doctor. As her symptoms kept on worsening, she was referred to our institute for further evaluation.
On examination, her oral temperature was 99°F, Blood Pressure (BP) was 110/70mmHg and her pulse was regular with a rate of 96/minute. Her respiratory rate was 18 per minute; her SpO2 was 88% at room air. She had bilateral pitting pedal oedema with raised Jugular Venous Pressure (JVP). Respiratory system examination revealed drooping of the left shoulder and flattening of the left side of the chest on inspection. There was reduced respiratory movement over the left mammary region. On palpation, expansion was reduced over the left hemithorax. The trachea was shifted to the left side and on auscultation; air entry was decreased over the left side of the chest. On the right side, there were harsh vesicular breath sounds with coarse inspiratory crackles and rhonchi over all the area. On cardiovascular examination, the apex was localized 2cm lateral to the mid-clavicular line at the 5th intercostal space. Auscultation revealed a loud P2 and no murmurs were heard.
Blood investigations included an Erythrocyte Sedimentation Rate (ESR) of 22mm/hr, haemoglobin of 16.2mg/dl and a packed cell volume of 49.0%. Her Total Leukocyte Count (TLC) was 17000/cumm with 85% polymorphs, 13% lymphocytes and 2% eosinophils. Her kidney function tests and serum electrolytes were normal. Direct and indirect bilirubin levels were 0.2mg/dl each; however, her SGOT and SGPT levels were 888 IU/L and 643 IU/L respectively. Arterial Blood Gas (ABG) analysis was suggestive of compensated type II respiratory failure with a pH of 7.351, PaCO2 of 58.0mmHg, PaO2 of 68mmHg and HCO3- of 31.3mEq/L.
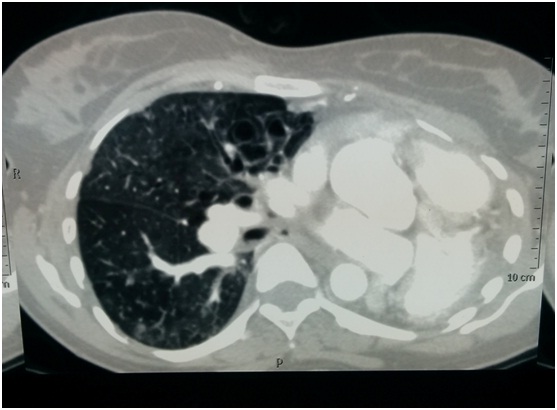
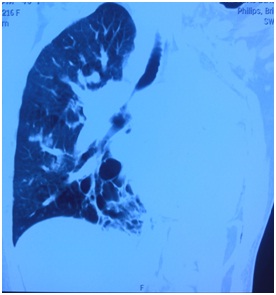
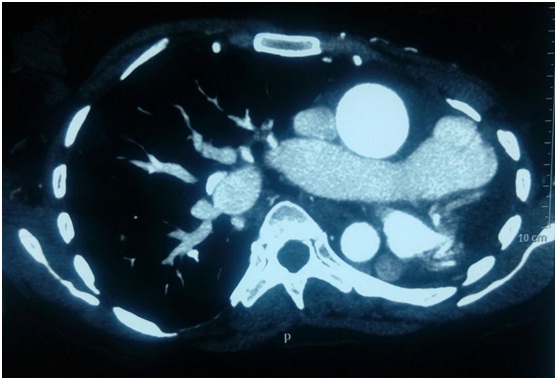
A chest X-ray (PA view) was performed on which the left hemithorax appeared opaque and there was ipsilateral mediastinal shift along with crowding of ribs. The right lung showed bronchiectatic changes predominantly in the middle and lower zones [Table/Fig-1]. Based on clinical evaluation and the appearance on imaging, a provisional diagnosis of a post tubercular damaged lung probably with underlying collapse was made. A Computed Tomography (CT) scan of thorax was done for confirmation which showed absence of lung parenchyma on the left side, with shifting of mediastinum towards the left. The left main bronchus was not visualised. There were cystic bronchiectatic changes with air fluid levels in basal segments of right lower lobe and medial segment of right middle lobe with ground glass haziness and ill-defined nodule in right upper lobe. There was no pleural effusion or lymphadenopathy [Table/Fig-2,3]. CT pulmonary angiography was also carried out, on which the left main pulmonary artery and superior and inferior pulmonary veins were not visualised [Table/Fig-4,5]. On bronchoscopy too, the left main bronchus was not visualised [Table/Fig-6].
Chest X ray showing opaque left hemithorax with mediastinal shift to left.

Transverse section of CT chest showing left lung agenesis and right lung bronchiectasis.
Coronal section of CT chest showing compensatory expansion of right lung with right lower lobe bronchiectasis.
CT pulmonary angiography showing absent pulmonary vasculature on left side.
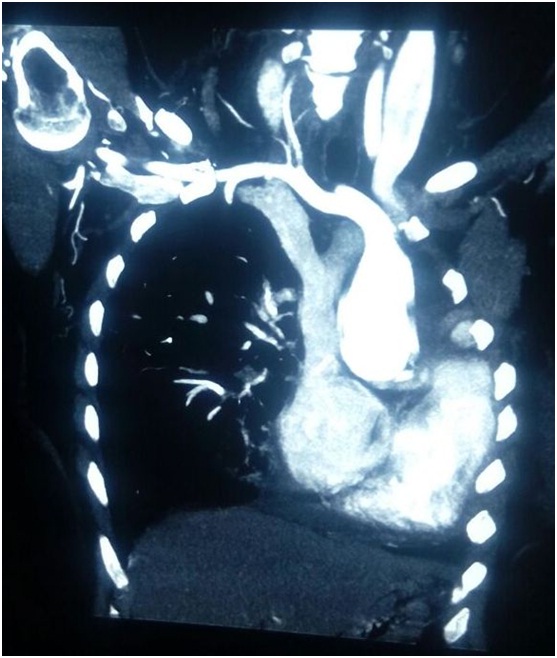
Absent left pulmonary artery and elongated main pulmonary artery.
Absent left bronchus on bronchoscopy.

Two Dimensional Echocardiography (2D ECHO) showed dilated right atrium and ventricle with a D-shaped left ventricular cavity. There was mild tricuspid regurgitation and mild pulmonary arterial hypertension with right ventricular systolic pressure of 45mmHg. USG abdomen and pelvis was normal. Sputum cultures were sterile and smear for Acid Fast Bacilli (AFB) was negative.
The patient was diagnosed as left lung agenesis and right lung bronchiectasis with cor pulmonale, mixed respiratory failure and right sided pneumonia. She was managed with antibiotics, bronchodilators, diuretics, oxygen inhalation and intermittent Bilevel Positive Airway Pressure (BiPAP) therapy. The patient was symptomatically better and afebrile at discharge. She was advised to follow-up regularly and the possible need for domiciliary oxygen was explained.
Discussion
In 1673, De Pozze described the first ever case of pulmonary agenesis in a female cadaver, and Muhamed reported the first case of unilateral lung agenesis from India in 1923 in an autopsy [1]. Pulmonary agenesis is a rare congenital anomaly with an incidence between 0.0034% and 0.0097% [2]. The aetiology is elusive and is believed to be due to certain genetic factors, vitamin A or folate deficiency and viral infections [3]. Males are affected more commonly than females.
Left sided lung agenesis is present in 70% cases and is associated with a more favourable outcome [4]. Right lung agenesis is more frequently associated with cardiovascular anomalies and has a worse prognosis due to rightward mediastinal shift which distorts bronchial and vascular structures [5]. Almost 50% cases of lung agenesis have various congenital anomalies. Cardiovascular anomalies (patent ductus arteriosus, patent foramen ovale, scimitar syndrome), gastrointestinal (tracheoesophageal fistulas, duodenal atresia), facial (cleft lip, mandibular hypoplasia), skeletal (absent rib, hemivertebrae) and genitourinary (horse shoe kidney) are few commonly associated anomalies [6]. Most of these patients with associated anomalies present in childhood and are diagnosed earlier. However, those with only lung agenesis, can remain asymptomatic for several years or can have recurrent lower respiratory tract infections and diagnosis can be delayed due to confusion with other common entities.
In 1912, Schneider originally classified lung agenesis in three groups which was later modified and made more practical by Boyden in 1955 [7]. Depending upon the degree of defect, lung agenesis patients can be classified into three groups. Group 1 (Agenesis): Complete absence of bronchus, lung and pulmonary vasculature; Group 2 (Aplasia): Rudimentary bronchus is present but lung parenchyma and vessels are absent; Group 3 (Hypoplasia): Hypoplastic lung, bronchus or vasculature is present. In our case, patient had Type 1 left lung agenesis without any other anomaly and hence, had a better prognosis.
Diagnosis is made by radiological investigations. Chest X-ray shows opaque hemithorax with ipsilateral mediastinal shift and compensatory hypertrophy of normal lung. Other differentials include collapse, pleural effusion, pneumonectomy, destroyed lung and diaphragmatic hernia. CT scan can help in visualizing rudimentary bronchus and is the preferred imaging modality. Absent or rudimentary bronchus can be seen directly by bronchoscopy also. Pulmonary angiography is the confirmatory test for ipsilateral absence of pulmonary vasculature [8]. Bronchography is obsolete and is no longer recommended. Echocardiography is mandatory for ruling out cardiac anomalies and pulmonary hypertension. Pulmonary hypertension is a common complication of lung agenesis due to loss of pulmonary vasculature.
Bronchiectasis in other lung is rarely associated with lung agenesis and possible explanation for bronchiectasis is recurrent infection due to pooled secretions in bronchial stump or impaired drainage of lung secretions. Only few cases of lung agenesis with bronchiectasis of normal lung have been reported so far [9–10].
Treatment should be individualized; those who are asymptomatic need no treatment. Associated congenital anomalies should be corrected as per feasibility; lung infections should be treated with antibiotics. Also, bronchial stump resection can be done in lung aplasia patients with recurrent infections.
Conclusion
Lung agenesis is commonly misdiagnosed as collapse or pleural effusion. A high index of suspicion is needed for early diagnosis and lung agenesis should be always considered in patients with persistent opaque hemithorax on chest radiography.
[1]. Muhamed K.S.N, Absence of left lungInd Med Gaz 1923 58:262-64. [Google Scholar]
[2]. Mardini MK, Nyhan WL, Agenesis of the lung: Report of four patients with unusual anomaliesChest 1985 87:522-27. [Google Scholar]
[3]. Currarino G, Williams B, Causes of congenital unilateral pulmonary hypoplasia: a study of 33 casesPediatr Radiol 1985 15:15-24. [Google Scholar]
[4]. Oyamada A, Gasul BM, Holinger PH, Agenesis of the lungAm J Dis Child 1953 85(2):182-201. [Google Scholar]
[5]. Chou AK, Huang SC, Chen SJ, Huang PM, Wang JK, Wu MH, Unilateral lung agenesis-detrimental roles of surrounding vesselsPediatr Pulmonol 2007 42(3):242-48. [Google Scholar]
[6]. Mühlhausen GM, Arcil GG, Right lung agenesis in a newbornRev Chil Pediatr 1992 63(1):39-42. [Google Scholar]
[7]. Boyden E, Developmental anomalies of lungAm J Surg 1955 89:79-88. [Google Scholar]
[8]. Guven S, Koyuturk Y, Cerrah Celayir A, Karadeniz L, Celikoglu S, An unusual cause of respiratory distress: Unilateral pulmonary agenesisArch Dis Child 2001 84(3):F197 [Google Scholar]
[9]. Koseoglu N, Ucan ES, Cavdar C, Right lung agenesis and left lung bronchiectasisRespir Med 2005 1:110-12. [Google Scholar]
[10]. Roy PP, Datta S, Sarkar A, Das A, Das S, Unilateral pulmonary agenesis presenting in adulthoodRespir Med Case Rep 2012 5:81-83. [Google Scholar]