Cavernous Sinus Thrombosis (CST) is a rare, life-threatening condition that may result from the direct spread of infection from the nose, ears, teeth or sinuses. It is most commonly caused by Staphylococcus aureus and Streptococcus sp. We present a case of CST caused by Strepotococcus mitis and Staphylococcus lugdunensis. Early surgical intervention with aggressive medical management is needed as the syndrome carries a high mortality. To our knowledge this is the first case of CST associated with these two organisms.
Magnetic resonance imaging, Streptococcal infections, Sinusitis
Case Report
A 79-year-old woman with a past medical history of diabetes mellitus, hypertension, and dementia was brought in by her son with acute onset of altered mental status and a 3 day history of progressively worsening swelling and discharge from her right eye. The patient had no history of trauma or a recent surgical procedure. There was no history of fever, chills, nausea or vomitings. Vital signs were significant for a temperature of 96.80F, blood pressure of 143/66mm Hg and heart rate of 82 beats/minute.
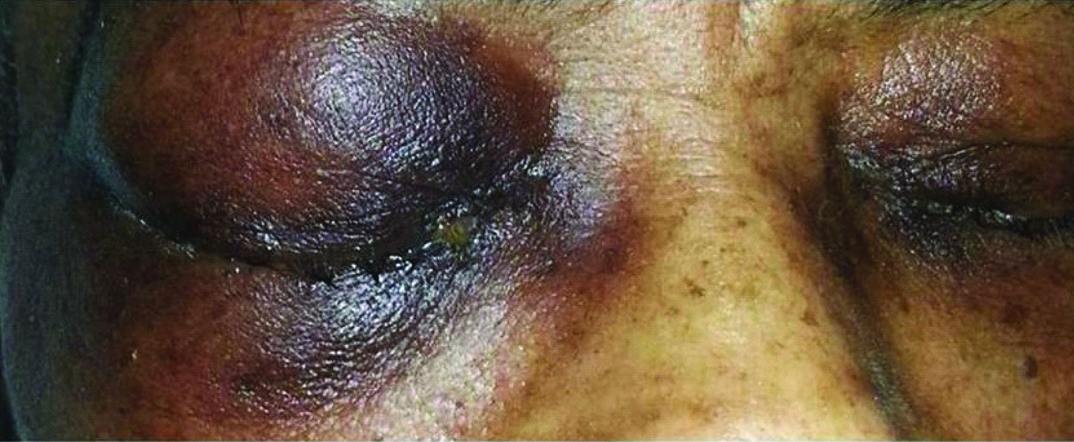
On physical examination the patient was lethargic, responsive only to painful stimuli. The cardio pulmonary examination was significant for normal heart sounds, with a 2/6 systolic murmur and the lungs were clear to auscultation. Eye examination showed proptosis of the right eye, peri-orbital swelling with chemosis, and conjunctival injection. A yellow serous discharge was noted [Table/Fig-1]. Pupils were hyper pigmented, reactive to light with no spontaneous movement. There was no evidence of any cranial nerve palsy.
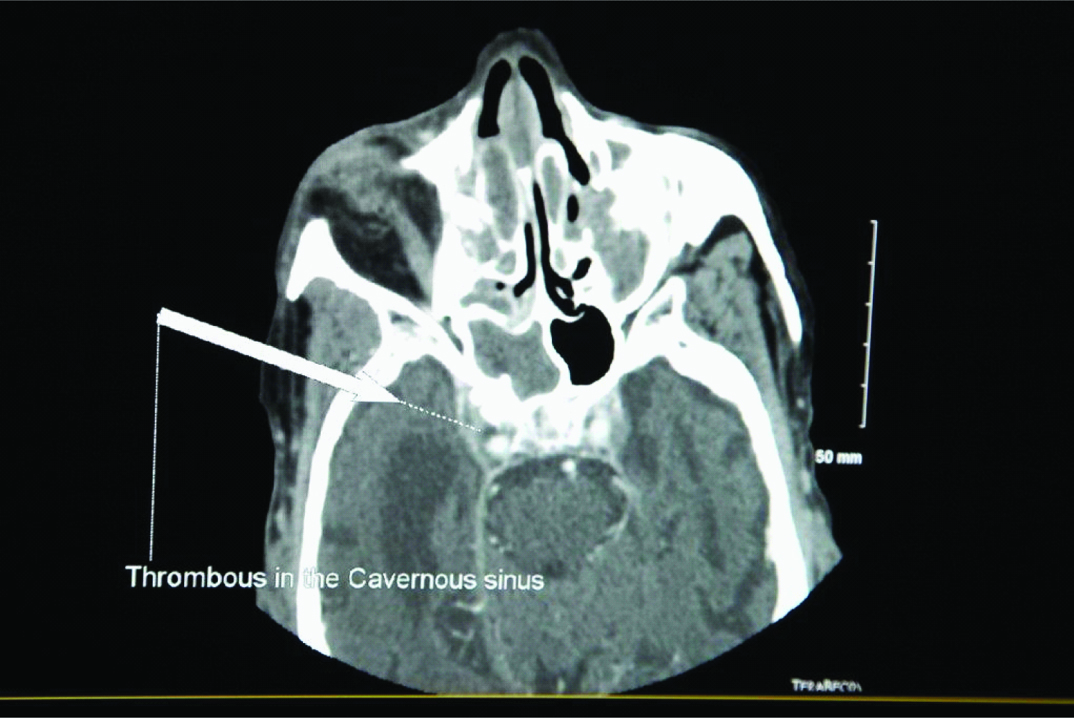
Computerized Tomography (CT) scan of the brain and orbits with contrast showed pre-septal edema of the right orbit with mild right -sided proptosis, total opacification of left and right maxillary sinuses and right-sided sphenoid sinus [Table/Fig-2]. Brain Magnetic Resonance Imaging (MRI) with contrast and venography showed CST with thrombosis of the right-sided superior ophthalmic vein with secondary proptosis and extensive mucosal sinusitis with suspected abscesses within the right maxillary and sphenoid sinuses [Table/Fig-3].
Examination of eye with peri-orbital swelling, chemosis with yellow serous discharge).
CT scan of the brain and orbits with contrast showing pre-septal edema of the right orbit with mild right -sided proptosis, total opacification of left and right maxillary sinuses, and right-sided sphenoid sinus).
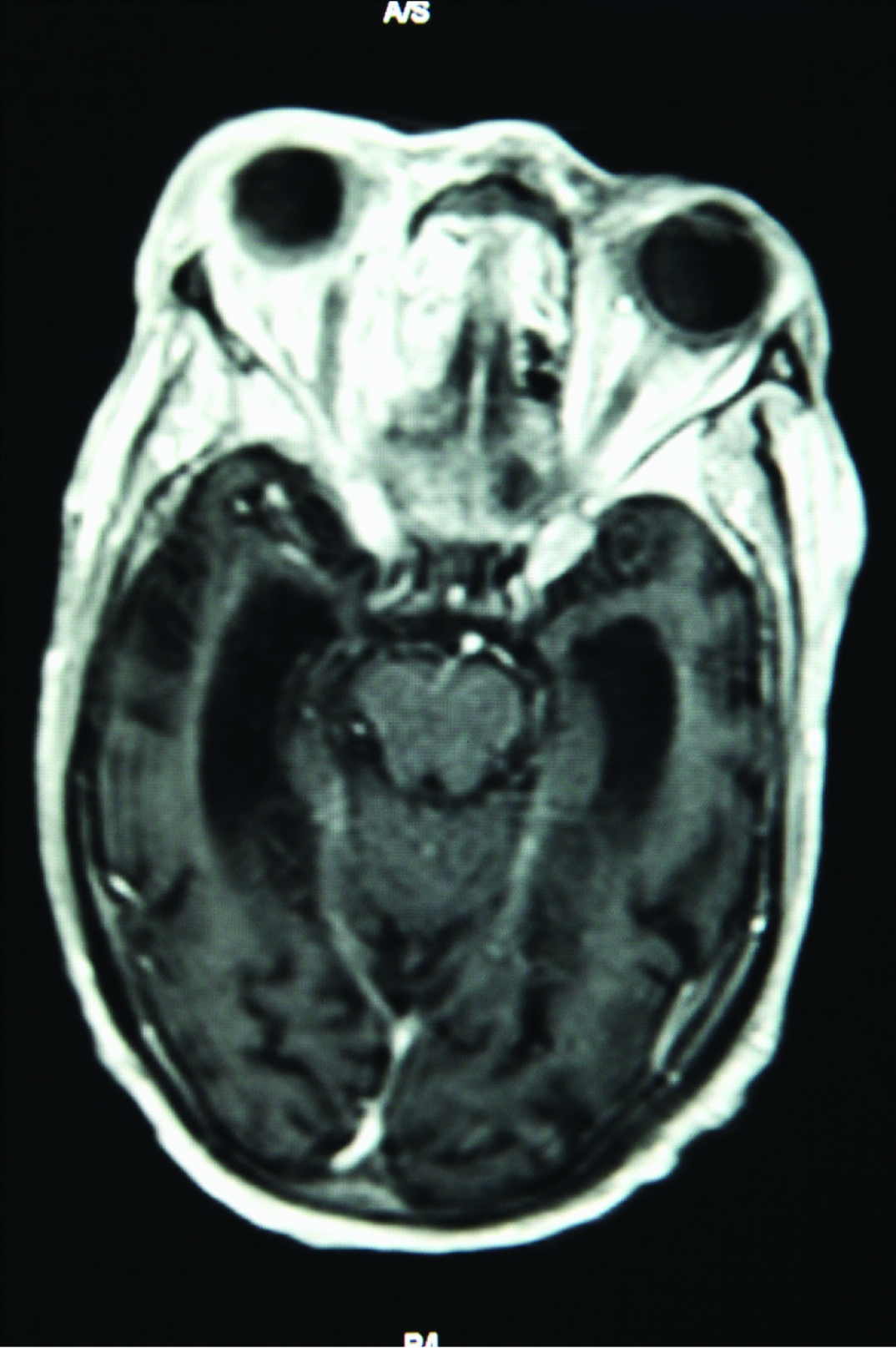
MRI of brain with contrast and venography revealing cavernous sinus thrombosis).
The patient underwent resection of the right concha bullosa, bilateral maxillary antrostomy, bilateral total ethmoidectomies, right sphenoidectomy, excision and drainage of bilateral middle turbinates, and drainage of sinus abscesses. In addition, the patient also underwent bilateral endoscopic frontal sinusotomies with debridement and bilateral endoscopic orbital decompression. Intraoperative deep cultures of the right maxillary sinus grew Streptococcus mitis and Staphylococcus lugdunensis, which were incubated in CO2 incubator for 370C on tryptic sheep agar blood plate. Streptococcus mitis was identified by remel RapID STR system and Staphylococcus lugdunensis was identified by microscan Walkaway 96 plus (Siemens, Illinois). The sensitivity panel of the S. mitis was unable to be done as the organism did not grow in the identification and sensitivity panel. S.lugdunensis was sensitive to penicillin, oxacillin, clindamycin, vancomycin, levofloxacin, trimethoprim-sulfamethoxazole and rifampicin identified by microscan Walkaway 96 plus (Siemens, Illinois).
The patient was treated with intravenous ceftriaxone 2gm every 12 hours for 5 days which was then changed to intravenous cefepime 2gm every 12 hours after the availability of culture results to cover against both the organisms. The patient was anticoagulated with intravenous heparin which was later changed to coumadin. The patients’ mental status improved gradually with significant reduction of peri-orbital swelling. Finally the patient was discharged on intravenous cefepime at the same dose to complete six weeks of antibiotics, but was lost to follow-up.
Discussion
CST is a rare but serious complication of an infectious process in adjacent anatomical sites [1]. The cavernous sinuses have extensive direct and indirect vascular connections to the nasal, ethmoidal and sphenoid sinuses making them vulnerable to septic thrombosis resulting from an infection of the sphenoid and ethmoid sinuses [1].
Infections arising at other locations such as the face, nose, tonsils, soft palate, teeth and ears have also been associated with CST but are much less common [1,2]. Orbital infection is rarely complicated by septic thrombosis of the cavernous sinus however, orbital cellulitis may be difficult to differentiate from the ocular manifestations of CST [3].
Staphylococcus aureus (S.aureus) is the most commonly isolated organism and is implicated in two thirds of the cases, Pneumococcus and other streptococcal species have been implicated in most of the remaining cases [2]. Gram- negative bacilli and anaerobic bacteria are uncommonly isolated. Fungal infections have also been described [1,2].
Clinical manifestations include fever, headache, diplopia, exophthalmos with 3rd or 5th cranial nerve involvement [1]. The infection can rapidly spread leading to altered mental status, meningitis, brain abscess, and coma if not treated immediately [4].
CST is usually diagnosed by imaging such as CT scan or MRI [5]. Blood cultures are positive in about 70% cases [6]. Cerebrospinal fluid findings show leukocytosis with normal opening pressure, glucose and protein similar to aseptic meningitis.
Empiric antibiotic, with activity against S.aureus; continued for 2-4 weeks with aggressive surgical debridement have been advocated [4]. The use of anticoagulants is controversial with unclear benefit [7]. Prognosis is poor with mortality of 20-30% even with appropriate medical and surgical management [2].
S.lugdunensis is a coagulase-negative staphylococcus, the organism is a commensal of the human skin [8,9]. It has been described as a cause of invasive infections such as intravascular, endocarditis joint infections [9,10]. The organism has been isolated from nasal swabs in 6% of adults who have a nasal carriage of staphylococci [11,12]. Sinusitis due to S.lugdunensis has been rarely documented. Mathews et al., described a patient with right sided necrotizing maxillary and ethmoidal sinusitis, the patient was also described as having periorbital cellulitis, conjunctivitis and disseminated varicella-zoster virus infection [13]. The patient underwent endoscopic sinus exploration and tissue from the sinus grew S.lugdunensis which was initially identified as S.aureus. The patient was treated with amoxicillin -clavulanate for 12 days with marked improvement and then switched to clindamycin for a total of 6 weeks.
S.mitis is a member of the viridans group of streptococci and is part of the flora of the oropharynx, gastrointestinal system and the female genital system. Upper respiratory infections including sinusitis are uncommonly encountered in clinical practice. Kutlu et al., described a case of alcoholic patient admitted to the hospital with change in mental status, fever, headache and confusion [12]. Spinal tap revealed cloudy cerebro-spinal fluid with high WBC and high protein. The cultures from CSF were identified as S. mitis. He was treated with ampicillin for 14 days. The authors thought maxillary sinusitis was the source of the infection but the organism was not recovered from the sinus.
Karssemakers et al., reported of a patient who presented with progressive facial swelling a week after dental extraction. MRI was significant for intracranial abscess with bilateral CST. The cultures from the abscess grew Streptococcus anginosis, was treated with intravenous antibiotics for 3 weeks with complete recovery [14].
The case described herein is unique. Polymicrobial infection of the cavernous sinus has not been previously described. To our knowledge, S.lugdunensis and S.mitis have not been previously reported as a cause of CST, it is possible that S.lugdunensis as a cause of CST has been previously underreported due to being misidentified as has been the case as reported by Mathews et al., [13]. S.lugdunensis and Streptococcus mitis should be considered in the list of organisms causing sphenoid sinusitis complicated by CST.
Conclusion
As CST has high mortality, early surgical intervention with immediate empiric antibiotics is indicated to reduce the mortality. Obtaining intra-operative cultures can guide to taper to appropriate antibiotics.
[1]. Southwick FS, Septic thrombosis of the major dural venous sinusesCurr Clin Top Infect Dis 1995 15:179-203. [Google Scholar]
[2]. Ebright JR, Pace MT, Niazi AF, Septic thrombosis of the cavernous sinusesArch Intern Med 2001 161(22):2671-76. [Google Scholar]
[3]. Atfeh MS, Khalil HS, Orbital infections: five-year case series, literature review and guideline developmentJ Laryngol Otol 2015 129(7):670-76. [Google Scholar]
[4]. Laupland KB, Vascular and parameningeal infections of the head and neckInfect Dis Clin North Am 2007 21:577-79. [Google Scholar]
[5]. Hurley MC, Heran MK, Imaging studies for head and neck infectionsInfect Dis Clin North Am 2007 21:305-53. [Google Scholar]
[6]. Ebright JR, Pace MT, Niazi AF, Septic thrombosis of the cavernous sinusesArch Intern Med 2001 161:2671-76. [Google Scholar]
[7]. Bhatia K, Jones NS, Septic cavernous sinus thrombosis secondary to sinusitis: Are anticoagulants indicated? A review of the literatureJ Laryngol Otol 2002 116:667-76. [Google Scholar]
[8]. Frank K, Del Ponjo JL, Patel R, From clinical microbiology to infection pathogenesis: how daring to be different works for Staphylococcus lugdunensisClin Microbiol Rev 2008 21:111-33. [Google Scholar]
[9]. Bocher S, Tonning R, Skow L, Prag J, Staphylococcus lugdunensis, a common cause of skin and soft tissue infections in the communityJ Clin Microbiol 2009 47:946-50. [Google Scholar]
[10]. Liu PY, Staphylococcus lugdunensis infective endocarditis: a literature review and analysis of risk factorsJ Microbiol Immunol Infect 2010 43:478-84. [Google Scholar]
[11]. Ohara-Nemoto Y, Haraga S, Kimura Nemoto TK, Occurrence of staphylococci in the oral cavities of healthy adults and nasal oral trafficking of the bacteriaJ Med Microbiol 2008 57:95-99. [Google Scholar]
[12]. Kutlu S, Sacar S, Cevahir N, Turgut H, Community acquired Streptococcus mitis meningitis: a case reportInt J of Infect Dis 2008 12(6):e107-08. [Google Scholar]
[13]. Matthews PC, Lazarus R, Prothroe A, Milford C, Bowler CJW, Acute necrotizing sinusitis caused by Staphylococcus lugdunensisJ Clin Microbiol 2011 49(7):2740-42. [Google Scholar]
[14]. Karssemakers LH, Forouzanfar T, Schulten EA, Karagozoglu KH, Bilateral conjunctival swelling after dental extractionLancet Infect Dis 2015 15(6):746 [Google Scholar]