Accessory Upper Subscapular Nerve – The Neurotisation Tool
Vishwajit Ravindra Deshmukh1, Rabindra Prasad Mandal2, Harisha Kusuma3, Neerja Rani4
1 Senior Resident, Department of Anatomy, AIIMS, New Delhi, India.
2 Student, Department of Anatomy, AIIMS, New Delhi, India.
3 Senior Resident, Department of Anatomy, AIIMS, New Delhi, India.
4 Assistant Professor, Department of Anatomy, AIIMS, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Neerja Rani, Room. 1040, Department of Anatomy, First floor, AIIMS, New Delhi, India.
E-mail: neerja.sirohi@gmail.com
During the routine dissection classes for undergraduate students, uncommon variation in relation to the upper subscapular nerve of posterior cord of brachial plexus was observed. Normally upper subscapular nerve takes origin from the posterior cord, but in this case report, it arises in triplet fashion, just above the circumflex scapular artery. All these accessory nerves were supplying upper part of the subscapularis muscle. As per our knowledge, this is a rare variation of brachial plexus. Many variations are encountered in the formation of brachial plexus. The normal and the abnormal origin of nerves are important considering neurotisation surgeries as well as during the infraclavicular nerve block for various axillary and upper limb surgeries.
Brachial plexus, Infraclavicular blocks, Neurotisation surgeries, Posterior cord, Upper subscapular nerve
Case Report
During routine dissection classes conducted for first-year MBBS students, branching pattern of brachial plexus was studied in the Department of Anatomy, AIIMS, New Delhi, India. The variation of upper subscapular nerve of the posterior cord of brachial plexus in the right upper limb was encountered in a male cadaver, aged 55 years. The cadaver was donated to AIIMS and the cause of death was not known. The cadaver has no pathological lesions, traumatic lesions, or surgical procedures in the neck and axillary region. In the present study, the area between the scapular region and upper end of humerus with attached muscles along with posterior axillary wall was examined for variation, after abducting arm at 900. Cords of brachial plexus were seen lying between flexor muscle of upper limb and scapular muscles.
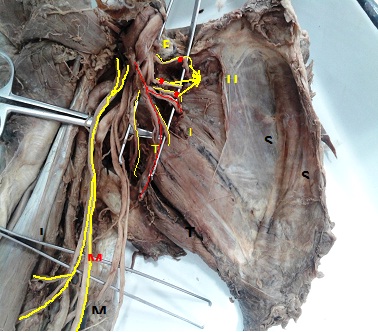
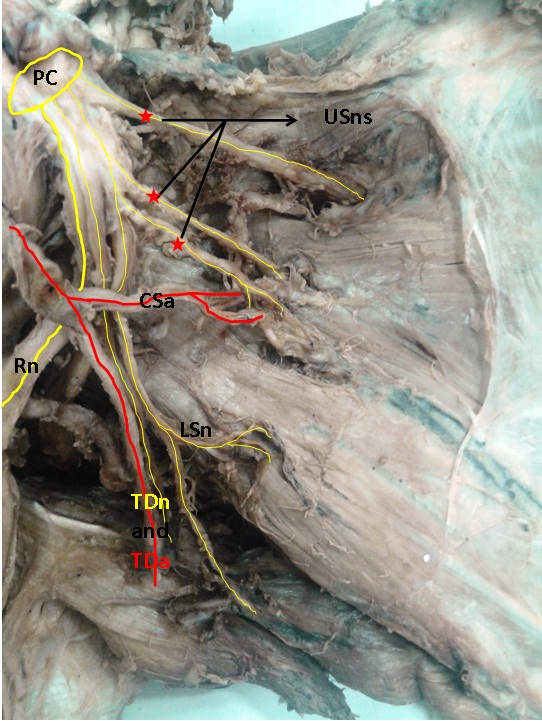
In the posterior cord, variability in the formation of subscapular nerve in relation to subscapular artery was seen [Table/Fig-1]. Three accessory subscapular nerves were observed to take origin above the bifurcation of subscapular artery. These accessory nerves, one nerve originating directly from the posterior cord, other from lower subscapular nerve and the remaining third, midway between them. All these accessory nerves supply upper part of the subscapularis muscle. Lower subscapular nerve seems to take origin from the posterior cord as separate nerve, below the circumflex scapular artery. This nerve supplies lower part of subscapularis muscle and teres major [Table/Fig-2]. On the other hand, in the left axilla, the branching pattern of posterior cord and its relation to subscapular artery was normal.
Origin of upper subscapular nerve (*) along with accessory nerves and lower subscapular nerve. PC-Posterior cord, USn-Upper subscapular nerve, LSn-Lower subscapular nerve, TDn-Thoracodorsal nerve, SSm-Subscapularis muscle, SAm-Serratus anterior muscle, TMm-Teres major muscle, LBBm-Long head of bicep brachi, MCn -Musculocutaneus nerve, MN-Median nerve.
Branches of posterior cord (PC) of brachial plexus. USns (*)-Upper subscapular nerves (Three separate upper subscapular nerves from the posterior cord), LSn-Lower subscapular nerves, CSa-Circumflex scapular artery, TDn/TDa-Thoracodorsal nerve and artery, RN-Radial nerve.
Musculocutaneous nerve takes origin from the main trunk of the median nerve [Table/Fig-1]. After originating, it is further dividing into branches, which supplies muscles of the anterior compartment of arm and continues as the lateral cutaneous nerve of arm.
Discussion
Brachial plexus predominantly supplies upper limb and is formed by ventral rami of the lower four cervical (C5-C8) and the first thoracic (T1) nerve. C5 and C6 cervical rami unite to form upper trunk, C8 and T1 rami join to form lower trunk and the C7 ramus continues as the middle trunk. Trunks will divide into anterior and posterior division, which rearrange themselves and forms three cords (medial, lateral and posterior) [1].
During the embryonic stage, upper limb bud lies in the vicinity of the lower five cervical and upper two thoracic segments. When the limb bud begins to develop, the ventral primary rami of the spinal nerves invade into the mesenchyme of the limb bud. Initially, each ventral ramus enters with isolated dorsal and ventral nerves for the extensor and flexor muscles respectively. Immediately after the nerves enter the limb bud, they establish intimate contact with the differentiating mesodermal condensations and the initial contact between the nerve and the muscle cells is necessary for their complete functional and anatomical differentiation [2]. It has been observed, that at the appropriate time during development, the end organs secrete either a trophic substance (netrin-1 and netrin-2) that attracts correct growth cones or trophic substance (BDNF) or Insulin-like Growth Factor (IGF) that supports the viability of growth cones that happen to take right path [3]. Thus, inappropriate secretion of these growth factors may lead to unusual formation of brachial plexus [4].
The upper subscapular nerve originated from posterior cord and supplies subscapularis muscle, which are a medial rotator and adductor of the humerus (Infraspinatus and teres minor are lateral rotators of humerus). Spasticity and contracture of subscapularis muscle, plays a major role on flexor synergy pattern usually present in spastic hemiplegia, which can lead to painful shoulder [5]. It also helps to stabilize and prevent displacement of the head of humerus in the glenoid fossa during shoulder movements. To our knowledge, limited data is available regarding the variation of upper subscapular nerves and its relation with circumflex scapular artery. Thus, variations in the branching pattern of brachial plexus have clinical and surgical importance during neurotisation surgeries or neurovascular graft surgeries [6].
Numerous variations have been described by various authors in the branching pattern of brachial plexus. Previously, it was noticed that lower subscapular nerve, originated from posterior cord, has high variable branching pattern and percentage of variation is more in lower subscapular nerve. Muthoka et al., found lower subscapular nerve originating from axillary nerve [7]. Fazan et al., and Chaudhary et al., also observed the unusual origin of lower subscapular nerve as a branch of axillary nerve [8,9]. According to Tubbs RS, the lower subscapular nerve originated as the single nerve in 93.6% cases and two independent nerve trunk in 6.4% cases [10]. However, in the current study, lower subscapular nerve takes origin from posterior cord of brachial plexus.
In our case report, we found three accessory upper subscapular nerves arising from the posterior cord of brachial plexus supplying subscapularis muscle, above the bifurcation of subscapular artery. While other authors quoted that the upper subscapular nerve originated from the posterior cord in 97% of cases and from the axillary nerve in 3% cases. The upper subscapular nerve originated as single, double and triple nerves in 90.3%, 8%, 1.6% cases respectively [10]. According to Kim et al., upper subscapular nerve consists of three branches (80%), and four branches (20%) in Korean population [11]. In the previous studies, as mentioned above, authors have shown the branching pattern of upper and lower subscapular nerves but they have not mentioned the relation of these nerves with circumflex scapular artery.
Due to variant relation of artery and nerves, there could be chances of impingement of vessels leading to ischemia and loss of functional anatomy of muscle. Thus, the knowledge of variation of the upper subscapular nerve and its relation with vessels is important for anatomist because it may be the reason for nerve palsy syndromes. This nerve is also important for the radiologist, surgeons and anaesthesiologists because it has gained importance due to wide use in clinical and surgical procedures in the axilla, scapular fracture, shoulder dislocation and infraclavicular nerve blocks. We also found that musculocutaneus nerve is taking origin from the median nerve, which is formed by the two roots coming from the lateral and median cord. Knowledge of these accessory nerves is important, considering neurotisation procedures [12].
Conclusion
Knowledge of anatomical variation in the branching pattern of brachial plexus is important to note during neck and the axilla dissection. The unusual distributions are prone to damage while managing neck and axillary tumours. Also, the presence of accessory nerves is important for neurosurgeons for neurotisation surgeries and brachial plexus repair. It is also helpful for anaesthesiologists to know the variation for improving guidance during infraclavicular nerve blocks.
[1]. Standring S, Gray’s anatomy. Pectoral girdle, Shoulder region, Axilla. The Anatomical basis of clinical practice 2008 40th EdLondonElseveir Churchill:780-81. [Google Scholar]
[2]. Saddler TW, Muscular system. Langman’s Medical Embryology 2006 10th EdPhiladelphiaLippincott Williams and Wilkins:146-47. [Google Scholar]
[3]. Larsen WJ, Development of the peripheral nervous systemIn: Essentials of Human Embryology 1998 2nd EdNew YorkChurchill Livingstone Inc:69-79. [Google Scholar]
[4]. Gaur S, Katariya SK, Vaishnani H, A cadaveric study of variation of posterior cord of brachial plexusInt J Biol Med Res 2012 3(3):2214-17. [Google Scholar]
[5]. Menezes CC, ricenti SV, Mendes FMP, Anatomical and clinical study of the subscapular nervesJ Morphol Sci 2010 27(2):74-76. [Google Scholar]
[6]. Haninec P, Samal F, Tomas R, Direct repair (nerve grafting), neurotization, and end-to-side neurorrhaphy in the treatment of brachial plexus injuryJ Neurosurg 2007 106:391-99. [Google Scholar]
[7]. Muthoka JM, Sinkeet SR, Shahbal SH, Matakwa LC, Ogeng’o JA, Variations in branching of the posterior cord of brachial plexus in a Kenyan populationJournal of Brachial Plexus and Peripheral Nerve Injury 2011 6:1 [Google Scholar]
[8]. Fazan VPS, Amadeu ADS, Caleffi AL, Filho OAR, Brachial plexus variations in its formation and main branchesActa Cir Bras 2003 18(5):1-8. [Google Scholar]
[9]. Chaudhary P, Singla R, Kalsey G, Arora K, Branching pattern of the posterior cord of the brachial plexus- A cadaveric studyJ Clin Diagn Res 2011 5(4):787-90. [Google Scholar]
[10]. Tubbs RS, Loukas M, Shahid K, Anatomy and quantitation of the subscapular nervesClin Anat 2007 20(6):656-59. [Google Scholar]
[11]. Kim JH, Woo JS, Hur MS, Lee KS, Anatomical studies of the upper and lower subscapular nervesKorean J Phys Anthropol 2014 27(4):219-23.(in Korean) [Google Scholar]
[12]. Bertelli JA, Ghizoni MF, Results and current approach for brachial plexus reconstructionJ Brachial Plex Peripher Nerve Inj 2011 16:2 [Google Scholar]