Role of Endoscopic Ultrasound for the Diagnosis of Isolated Gastric Cavernous Haemangioma
Jinlong Hu1, Hua Sao2, Siyu Sun3
1 Endoscopy Center, Shengjing hospital of China Medical University, Shenyang, China.
2 Endoscopy Center, Shengjing hospital of China Medical University, Shenyang, China.
3 General Surgery Department, Shengjing Hospital of China Medical University, Shenyang, China.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mr. Siyu Sun, Endoscopy Center, Shengjing Hospital of China Medical University, Shenyang-110004, China.
E-mail: sunsy@sj-hospital.org
Isolated gastric cavernous haemangioma is extremely rare in the stomach. Historically, endoscopy, computed tomography and MRI had been used to diagnose gastric cavernous haemangioma. Biopsy, is not an option due to its vascular nature and submucosal location. We report an isolated gastric cavernous haemangioma that was diagnosed by end-oscopic ultrasound in a 25-year-old male and treated by laparotomy. The final diagnosis of cavernous haemagioma was confirmed by post-operative pathology. There was no recurrence during 3-month follow-up period.
Gastric submucosal tumor, Gastric tumor, Laparotomy
Case Report
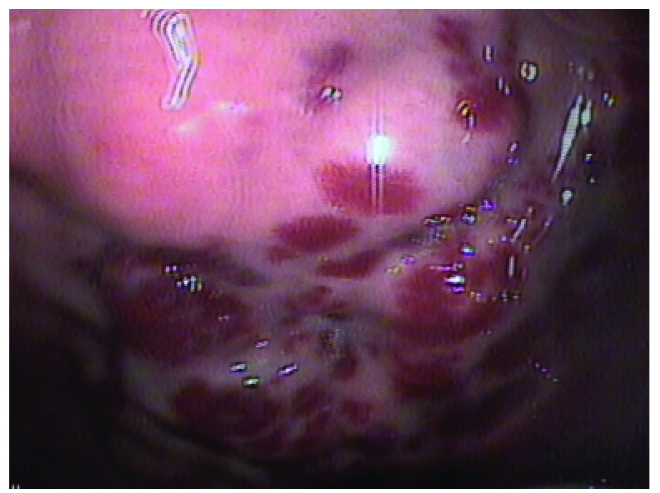
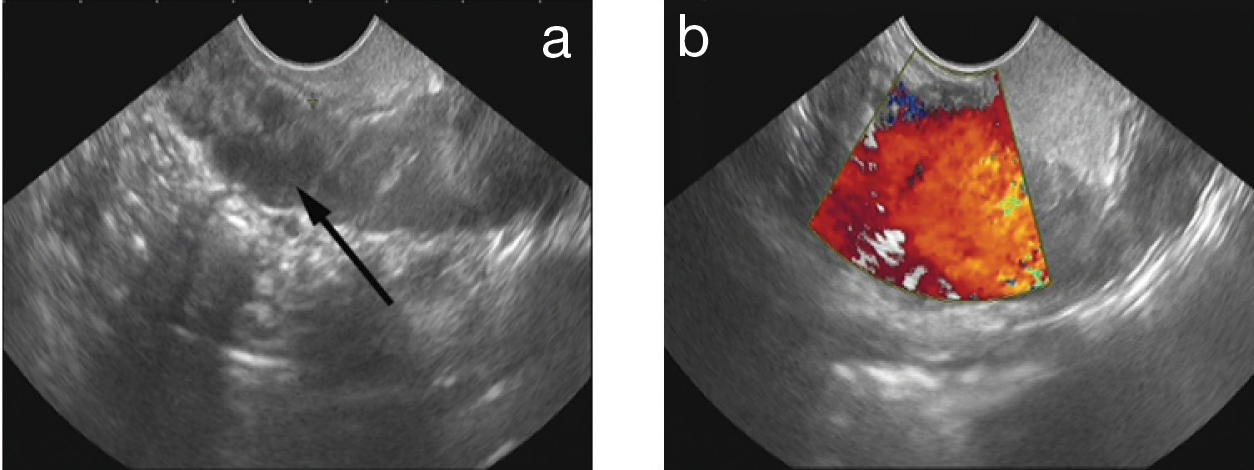
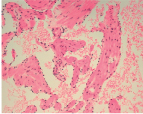
A 25-year-old male was referred to the department of surgery with intermittent melena and epigastric distension over the past 6 months. He denied history of jaundice, foreign body ingestion and adminstration of non-steroidal anti-inflammatory drugs. There were no associated skin lesions. Gastroscopy performed 10 years ago due to gastric pain was normal. On admission, laboratory tests were unremarkable, but haemoglobin was 9.6g/dl. Gastroscopy revealed a large vascular lesion located at the antrum-corpus junction on the greater gastric curvature [Table/Fig-1]. The linear endoscopic ultrasound demonstrated thickness of submucosal and propria muscularis layer with Doppler signal in it [Table/Fig-2a,b]. The provisional diagnosis was haemangioma. Contrast-Enhanced Computed Tomography (CECT) showed a mixed attenuation mass containing focal calcifications located on greater gastric curvature in the left upper abdomen [Table/Fig-3]. A vascular malformation was seen on the greater gastric curvature at laparotomy [Table/Fig-4] and a wedge resection was performed. Gastric cavernous haemangioma was diagnosed by post-operative pathology [Table/Fig-5]. The patient suffered no complications and recurrence during 3-month follow-up by gastroscopy and CT scan.
Polypoidal vascular lesion was seen on the great curvauture of the stomach
(a) Endoscopic ultrasound showed the thickness of lamina propria and submucosa of gastric lesion (Black arrow). (b) There was a doppler signal in the lesion.
Contrast-enhanced computer tomography demonstrated a mass of mixed attenuation in the left upper abdomen (Black arrow) and calcification (White arrow) in the mass.

Intra-operative findings: A vascular tumour in the external surface of the great curvature of stomach.

Gastric cavernous haemangioma was diagnosed by postoperative pathology.
Discussion
Gastric cavernous haemangioma is an extremely rare cause of gastrointestinal haemorrhage. Until now, there was no report that it can transform into malignancy, but the correct diagnosis is of utmost importance to the choice of treatment. This benign tumour can be missed, if only an upper gastrointestinal barium study is performed [1]. Endoscopic visualization of a blood filled haemangioma with the appearance of red nodules or vascular congestion can help make the diagnosis, but sometime only a mass like a submucosal tumour can be seen [2,3]. Pre-operative pathology is limited, due to submucosal localization and dense vascular nature of such lesions. But Malay Sharma et al., reported they got biopsy from a small rectal haemangioma without haemorrhage [4]. Radiological examinations, such as CT scan and MRI, suggest the possible diagnosis, which show the location and relationship of the lesion to surrounding structures. The lesion appears either as enhancing linear blood vessels or caput meduase, a radial orientation of small vessels that resemble the hair of Medusa from Greek mythology [2]. Calcification could be seen inside gastric cavernous haemangioma [3]. CT scanning and MRI, however, cannot distinguish gastric cavernous haemangioma from mesenchymal tumours, if the blood vessel signal is weak. On CT scanning, a gastrointestinal stromal tumour was suspected in our case at first by the radiologist. As Endoscopic Ultrasound (EUS) has been used by many other authors to detect varied gastric lesions [5–8], we report EUS can very well be used for the detection of gastric cavernous haemangiomas as well. When gastric cavernous haemangioma is like a submucosal tumour in gastroscopy or is difficult to diagnose by CT scan or MRI, EUS with doppler can show its origination and nature, differentiating it from gastric varices and mesenchymal tumours.
Endoscopic resection of a gastric cavernous haemangioma has been reported [9], but the lesion was limited to the mucosa and submucosa. Surgical excision is the only option for most patients. Cavernous haemangiomas may appear in various parts of the human body, including the liver, spleen, colon, bone, soft tissues, central nervous system, and mediastinum [10]. It is, however, extremely uncommon in the stomach.
Conclusion
In conclusion, preoperative diagnosis of Cavernous haemangiomas is of great importance to the choice of treatment. Endoscopy, CT and MRI are usually used to diagnose gastric cavernous haemangioma. However, it is sometimes difficult to diagnose. EUS can show its origin and nature, playing an important role in the establishment of a definitive diagnosis.
[1]. Samarji WN, Torrance HB, Diffuse capillary haemangioma of the stomachJ R Coll Surg Edinb 1973 18:167 [Google Scholar]
[2]. Zong L, Chen P, Shi GH, Gastric cavernous haemangioma: A rare case with upper gastrointestinal bleedingOncol Lett 2011 2:1073 [Google Scholar]
[3]. Yamaguchi K, Kato Y, Maeda S, Cavernous haemangioma of the stomach: a case report and review of the literatureGastroenterol Jpn 1990 25:489 [Google Scholar]
[4]. Sharma M, Adulqader A, Shifa R, Endoscopic ultrasound for cavernous haemangioma of rectumEndosc Ultrasound 2014 3:63 [Google Scholar]
[5]. Rana SS, Sharma R, Sharma V, An unusual cause of gastric submucosal bulge on endoscopyEndosc Ultrasound 2014 3:198 [Google Scholar]
[6]. Machicado J, Shroff J, Quesada A, Gastritis cystica profunda: Endoscopic ultrasound findings and review of the literatureEndosc Ultrasound 2014 3:131 [Google Scholar]
[7]. Salah W, Faigel DO, When to puncture, when not to puncture: Submucosal tumoursEndosc Ultrasound 2014 3:98 [Google Scholar]
[8]. Guo J, Liu Z, Sun S, Endosonography-assisted diagnosis and therapy of gastrointestinal submucosal tumoursEndosc Ultrasound 2013 2:125 [Google Scholar]
[9]. Arafa UA, Fujiwara Y, Shiba M, Endoscopic resection of a cavernous haemangioma of the stomachDig Liver Dis 2002 34:808 [Google Scholar]
[10]. Kinoshita T, Naganuma H, Yajima Y, Venous haemangioma of the mesocolonAJR Am J Roentgenol 1997 169:600 [Google Scholar]