HbA1c is an established marker of long term glycemic control in patients with Diabetes Mellitus (DM), and elevated HbA1c levels are associated with an increased risk for further microvascular and macrovascular disease [1]. Studies have consistently shown that optimal glycemic control (defined by as HbA1c ≤ 7%) results in a lower incidence of microvascular complications in both type 1 and type 2 DM [2]. Moreover, a recent report found that increase in HbA1c levels was also predictive of cardiovascular disease and mortality in patients without diabetes mellitus [3].
There have been few studies which have shown HbA1c to be predictive of CAD in non-diabetes, but only in limited studies HbA1c has been correlated with angiographically proven CAD using SYNTAX score. The SYNTAX (Synergy between PCI with Taxus and Cardiac Surgery) Score (SS) was developed as part of the SYNTAX trial with the objective to characterize and objectively quantify the severity and extent of CAD [4].
So, in this study we aimed to evaluate the correlation between HbA1c level and severity of CAD in non diabetic patients using SYNTAX score in a cohort of proven CAD on angiography at Gauhati Medical College, which is a major tertiary care hospital of North Eastern India.
Materials and Methods
The patients admitted to Cardiology Department, Gauhati Medical College, Gauhati, Assam, India, from June 2014 to June 2015, were included in the study. Patients with probable CAD who underwent. Coronary Angiography (CAG), non-diabetic patients (no previous history of diabetes and HbA1c level less than 6.5%) with proven CAD, fulfilling inclusion and exclusion criteria, were included for the study. It is a single centre, cross-sectional study.
Prior ethical clearance from the appropriate authorities was taken.
A proforma was predesigned and validated by Institutional Ethics Committee. Written informed consent was taken from the study participants. Study consisted of history, study of angiographic report and relevant biochemical investigations.
It consisted of patient details like hospital number, name, age, gender, history of diabetes, smoking, dyslipidemia, hypertension and other co-morbidities.
Patients were considered as hypertensive according to JNC 8 (The Eight Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure) criteria, diabetic as per ADA (American Diabetes Association) criteria, and dyslipidemia according to NCEP (National Cholesterol Education Program) criteria. In addition use of anti-hypertensive, anti-diabetic or lipid lowering medications were used as criteria for hypertension, diabetes and dyslipidemia respectively. Either current or past history of tobacco smoking for 6 months was considered as smoking positive.
Details of the angiography were obtained and weighed using SYNTAX score. The SYNTAX scores were calculated with the help of professional website tool: http://www.syntaxscore.com/.
Serum concentration of HbA1c was determined by immunoturbidometric method.
Inclusion criteria
All non-diabetes patients (no previous history of diabetes and HbA1c level less than 6.5%) with proven CAD on angiography were included in the study and CAD is defined as 50% reduction in luminal diameter by visual assessment of epicardial coronary arteries (≥50% obstruction in ≥1 coronary artery) [5].
Exclusion criteria
1. Patients with history of diabetes or HbA1c level greater than 6.5%.
2. Patients with <50% reduction in luminal diameter of epicardial coronary arteries on angiography were excluded from the study.
3. Patients with history of prior revascularization Percutaneous Coronary Intervention (PCI) or Coronary Artery Bypass Grafting (CABG) and known patients with haemoglobinopathies, anaemia or history of recent blood transfusion were excluded from the study.
Statistical Analysis
Severity of coronary artery disease was assessed using SYNTAX score and the number of coronary vessels diseased. Non- diabetic patients were divided in to four quartiles of HbA1c.
Data were presented as frequencies and percentages for categorical variables and mean ± standard deviation (SD) for continuous variables, unless otherwise indicated. Differences between groups were assessed by using the chi-square and ANOVA. Correlation between continuous variables was determined by Pearson correlation coefficients. Linear regression analysis was performed to show association between severity of CAD and HbA1c levels. Multivariate logistic regression was used to show HbA1c level as independent predictor of severity of CAD.
A p<0.05 was considered as statistically significant.
The analysis was carried out using SPSS Version 16.
Results
A total of 346 patients were included in the study. Mean age was 58.1±10.4 years. 91.9% (318) were males, 44.8% (155) were hypertensives, 29.2% (101) were smokers and 34.7% (120) were dyslipidemic. Patients were divided into four groups (interquartiles) according to HbA1c levels, less than 4.8%, 4.8% to 5.1%, 5.1% to 5.6%, and 5.6% to 6.5%. These groups had 25.4% (88), 28.6% (99), 21.09% (73), 24.8% (86) patients respectively. Among non-diabetics mean HbA1c was 5.1%. We compared different quartiles of HbA1c among non- diabetics with regard to SYNTAX score and number of diseased vessels. We used ANOVA and post hoc tests to analyse the difference between quartiles.
On analysis we found that CAD severity by SYNTAX score as well as number of vessels involved was significantly different among quartiles (p-values <0.001 and <0.001 respectively) [Table/Fig-1]. Increase in HbA1c level was strongly correlated with disease severity and higher SYNTAX score [Table/Fig-2]. A significant increase was noted in the mean number of diseased vessels (p-value < 0.001) as HbA1c level increases. Mean SYNTAX score was also significantly increased with increased HbA1c levels (<4.8, 4.8-5.1, 5.1- 5.6 and 5.6 to <6.5 respectively). In SYNTAX subgroups (<23, 23-32 and >32), mean HbA1c values were 4.9±0.4, 5.7±0.3 and 6.0±0.92 respectively.
Comparison of HbA1c quartiles among non diabetic patients.
| HbA1c Quartiles | | <4.8% | 4.8-5.1% | 5.1-5.6% | 5.6-6.5% | Total | p-value | Test value |
|---|
| Gender | Female | 6(1.7%) | 5(1.4%) | 8(2.3%) | 9(2.6%) | 28(8.1%) | 0.410 | 2.881 |
| Male | 82(23.7%) | 94(27.2%) | 65(18.8%) | 77(22.3%) | 318(91.9%) |
| Hypertension | | 37(10.7%) | 38(11.0%) | 34(9.8%) | 46(13.3%) | 155(44.8%) | 0.200 | 4.636 |
| Smoking | | 13(3.8%) | 35(10.1%) | 15(4.3%) | 38(11.0%) | 101(29.2%) | 0.000 | 22.663 |
| CAD | SVD | 58(16.8%) | 54(15.6%) | 17(4.9%) | 21(6.1%) | 150(43.4%) | 0.000 | 61.934 |
| DVD | 25(7.2%) | 30(8.7%) | 31(9.0%) | 28(8.1%) | 114(32.9%) |
| TVD | 5(1.4%) | 15(4.3%) | 25(7.2%) | 37(10.7%) | 82(23.7%) |
| Diagnosis | CSA | 41(11.8%) | 39(11.3%) | 35(10.1%) | 34(9.8%) | 149(43.1%) | 0.698 | 3.843 |
| UA/NSTEMI | 20(5.8%) | 24(6.9%) | 12(3.5%) | 17(4.9%) | 73(21.1%) |
| STEMI | 27(7.8%) | 36(10.4%) | 26(7.5%) | 35(10.1%) | 124(35.8%) |
| Dyslipidemia | | 30(8.7%) | 26(7.5%) | 29(8.4%) | 35(10.1%) | 120(34.7%) | 0.151 | 5.305 |
| SYNTAX Score | <23 | 84(24.3%) | 98(28.3%) | 58(16.8%) | 11(3.2%) | 25172.5%) | 0.000 | 2.178 |
| 23-32 | 4(1.2%) | 1(0.3%) | 12(3.5%) | 46(13.3%) | 63(18.2%) |
| >32 | 0 | 0 | 3(0.9%) | 29(8.4%) | 32(9.2%) |
N=346(100%), Pearson Chi square test was used to find significance in the different groups.
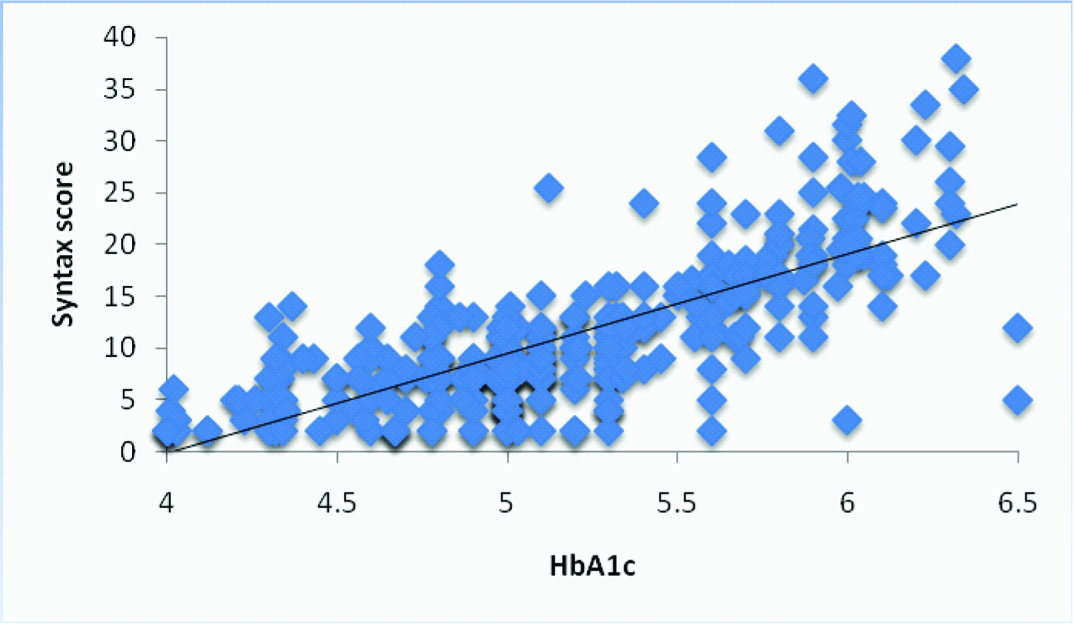
Linear regression analysis between HbA1c and SYNTAX score in non diabetic patients.
Linear regression analysis was done
R- 0.657, p <0.001
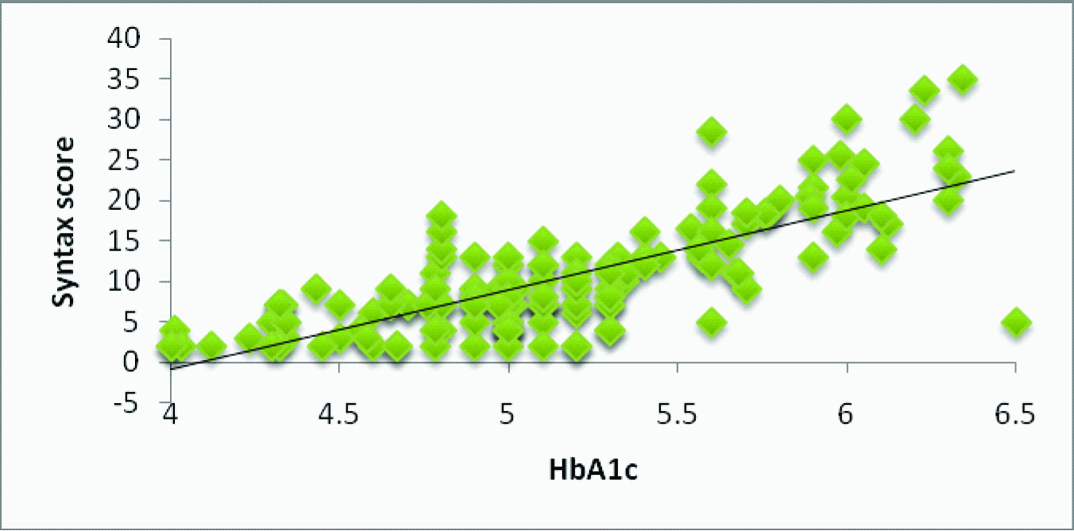
In subgroup analysis where only chronic stable angina patients were considered, there was significant linear correlation between HbA1c and severity of CAD by SYNTAX score (R-0.623, 0.820; p<0.001) and number of vessels involved (R-0.456, 0.35; p<0.001) [Table/Fig-3,4].
Multivariate analysis in non-diabetes.
| SYNTAX score >22 | B | Std. Error | Sig. | Exp (B) | 95% Confidence Interval for Exp (B) |
|---|
| Lower Bound | Upper Bound |
|---|
| Intercept | -4.324 | 0.706 | 0.000 | | | |
| Hypertension | 0.238 | 0.293 | 0.415 | 1.269 | 0.715 | 2.252 |
| Smoking | 0.898 | 0.317 | 0.005 | 2.455 | 1.320 | 4.567 |
| Dyslipidemia | 0.582 | 0.303 | 0.054 | 1.790 | 0.989 | 3.240 |
| HbA1c>5.1 | 3.444 | 0.485 | 0.000 | 31.314 | 12.101 | 81.029 |
| Male | 0.116 | 0.499 | 0.817 | 1.123 | 0.422 | 2.987 |
| Age>60 | 0.275 | 0.301 | 0.361 | 1.317 | 0.730 | 2.376 |
Multivariate analysis in non-diabetes, only HbA1c >5.1% was independent predictor of severity of disease by involving three vessels.
| CADThree vessels involvement (TVD) | B | Std. Error | Sig. | Exp (B) | 95% Confidence Interval for Exp(B) |
|---|
| Lower Bound | Upper Bound |
|---|
| Intercept | -2.491 | 0.548 | 0.000 | | | |
| Dyslipedemia | 0.241 | 0.279 | 0.388 | 1.273 | 0.737 | 2.198 |
| Smoking | 0.170 | 0.294 | 0.563 | 1.185 | 0.666 | 2.108 |
| Male | 0.148 | 0.490 | 0.763 | 1.159 | 0.444 | 3.030 |
| Hypertension | 0.074 | 0.273 | 0.786 | 1.077 | 0.631 | 1.839 |
| Age>60 yrs | 0.214 | 0.276 | 0.437 | 1.239 | 0.722 | 2.127 |
| HbA1c >5.1 | 1.632 | 0.292 | 0.000 | 5.115 | 2.888 | 9.060 |
Age, gender, hypertension and dyslipidemia did not show significant difference among quartiles; however, smoking was found to be an independent predictor of severity of CAD by SYNTAX score only in non-diabetics (p <0.05) [Table/Fig-5].
Linear regression analysis between HbA1c and SYNTAX score in non diabetic patients with chronic stable angina subgroup.
R-0.623; p<0.001
Linear regression was done.
Discussion
This is one of the first study from North Eastern India, where correlation between HbA1c level and severity of CAD in non-diabetic patients using SYNTAX score was attempted. In our study, increasing HbA1c level was strongly correlated with disease severity, number of diseased vessels and higher SYNTAX score, in a graded fashion (p<0.001) in non-diabetics. In our study in non-diabetics, linear regression analysis showed that HbA1c values significantly correlated with the SYNTAX score.
With increasing HbA1c levels, a significant increase was noted in the mean number of diseased vessels (p-value < 0.001). Similarly there was a linear correlation between HbA1c and number of vessels involved (R-0.402 and 0.429; p<0.001) in non-diabetics. Ghaffari et al., studied coronary angiographic findings and multi-vessel involvement based on HbA1c quartiles in non-diabetics. Patients with HbA1c >5.8% had twice more chance of having triple-vessel diseases [odds ratio (OR) = 2.21, 95% CI 1.34–3.65; p = 0.002] in non diabetics [6]. Kowalska et al., in a cohort of non-diabetic men referred for CAG, demonstrated that the number of diseased vessels significantly correlated with increasing levels of HbAlc [7]. Ikeda et al., showed that HbAlc is significantly associated with the complexity of coronary lesions. This association was even observed in non-diabetic adults [8].
In our study, we also calculated the SYNTAX score and tried to correlate disease severity with HbA1c. In non-diabetics, mean SYNTAX score significantly increased with increased HbA1c levels (SYNTAX scores were 6.5, 7.8, 11.5 and 20.22 in patients with HbA1c levels <4.8, 4.8-5.1, 5.1- 5.6 and 5.6 to <6.5 respectively). In SYNTAX subgroups (<23, 23-32 and >32), mean HbA1c values were 4.9±0.4, 5.7±0.3 and 6.0±0.92 respectively. In similar study by Garg et al., mean SYNTAX score was significantly increased with increasing HbA1c level (9.9% ± 12.2%, 12.9%±12.7%, 15.4%±15.2%, 19±15.5% in patients with HbA1c levels less than 5.5%, 5-5.7%, 5.8-6.1% and >6.1% respectively with p trend less than 0.001 [9]. Ayhan et al., showed that HbA1c levels correlated with Gensini score in premature coronary atherosclerotic patients (<40years old) in both diabetic and non-diabetics [10].
Our study utilized SYNTAX score to correlate disease severity with HbA1c. Most of the other studies have been done using Califf score [6] or Gensini score [10] or number of diseased vessels [8]. Garg et al., however utilized SYNTAX score to correlate disease severity with HbA1c [9]. But compared to their study we tried to study correlation of HbA1c with severity of CAD using lower quartile of HbA1c. We even showed correlation of HbA1c quartile of <4.8, 4.8-5.1 and 5.1-5.6 with severity of CAD in non-diabetics.
Multivariate logistic regression analysis showed that HbA1c >5.1% is an independent predictor of SYNTAX score >22 in non-diabetic population (OR = 1.604, 95% CI 1.045–2.462; p < 0.001).
Ghaffari et al., studied multivariate logistic regression analysis showed HbA1c >5.8% as an independent predictor of Califf scores >6 (OR = 3.17, 95% CI 1.79–5.69; p = 0.001) [6]. In study by Kaya et al., multivariate analysis, high levels of HbA1c were observed to be independent predictors of severe atherosclerosis [11].
In our study, age, gender, hypertension and dyslipidemia did not show significant correlation with severity of SYNTAX scores, in non-diabetics (p>0.05). However, smoking was found to be independent predictor of severity of CAD by SYNTAX score only in non-diabetics (p <0.05).
Similarly in a study by Ayhan et al., linear multivariate regression analysis (including age, sex, HbA1c levels, smoking, DM and hypertension as dependent parameters), only HbA1c was found to be an independent risk factor for the presence of severe CAD [10]. In study, Garg et al., found that on stepwise logistic regression analysis age >60, male gender, BMI of >23, and current smoking were independent predictors of CAD. But dyslipedemia was not a risk factor in the study [9]. Contrary to study by Garg et al., we failed to observe age, gender, hypertension and dyslipidemia to be independent predictor of severity of CAD by SYNTAX score. This could be because of study population itself. Our study population consisted of predominant males and small female population and 97% of total smokers were males. Moreover, smoking has been found to be a predominant risk factor for CAD in North-Eastern India. In our study on Acute Coronary Syndrome (ACS), from North Eastern India, we have observed smoking to be predominant risk factors with 45.02% of study population being smokers [12]. In another study from North-Eastern India, consumption of tobacco and smoking was found to be strongest risk predictor of myocardial infarction [13]. However, similar to our study, in a study by Ayhan et al., age, sex, DM and hypertension were not found to be an independent risk factor for the presence of severe CAD [10].
Limitation
Our study population consisted of predominant males and small female population, and this was mainly because of the demographic profile of the admitted patients.
First, because the patients enrolled in our study were candidates with proven CAD, so our findings are relevant to high-risk group. Therefore, the diagnostic thresholds derived from high-risk populations may not be generalized to lower risk groups. Second, given the observational, cross-sectional design of our study, the directionality of the association cannot be determined. Third, we used a single baseline measurement of HbA1c. Hence, we cannot evaluate the effects of changes in this parameter over long-term. So a prospective long term study would be ideal for analyzing prognostic importance and outcomes.
Conclusion
From this clinical study, we can conclude that a significant correlation exists between level of HbA1c and severity of CAD by SYNTAX score as well as number of vessels involved in non-diabetics and HbA1c is a simple and reliable measure to predict the severity of CAD, which can be used as complimentary to traditional risk factors to predict the severity of CAD.
N=346(100%), Pearson Chi square test was used to find significance in the different groups.