Hymenolepis diminuta Infection in a School Going Child: First Case Report from Uttarakhand
Pratima Gupta1, Priyanka Gupta2, Bhanu Kiran Bhakri3, Neelam Kaistha4, Balram Ji Omar5
1 Professor and Head, Department of Microbiology, AIIMS, Rishikesh, Uttarakhand, India.
2 Senior Resident, Department of Microbiology, AIIMS, Rishikesh, Uttarakhand, India.
3 Assistant Professor, Department of Paediatrics, AIIMS, Rishikesh, Uttarakhand, India.
4 Additional Professor, Department of Microbiology, AIIMS, Rishikesh, Uttarakhand, India.
5 Associate Professor, Department of Microbiology, AIIMS, Rishikesh, Uttarakhand, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Pratima Gupta, Professor and Head, Department of Microbiology, AIIMS, Rishikesh, Uttarakhand, India.
E-mail: drpratima68@gmail.com
Hymenolepis diminuta (H.diminuta) is prevalent worldwide, and a few hundred human cases have been reported till date. It is primarily a rodent parasite and humans (usually children) can act as accidental hosts. Infections are usually asymptomatic but abdominal pain, irritability, pruritis, mild diarrhoea and eosinophilia are among the existing symptoms in a few of the reported cases. Here, we report a case of an 11-year-old female child from Bijnor, who presented to us with complaints of abdominal pain, fatigue and irregular episodes of fever. Routine stool examination showed characteristic eggs of H.diminuta. Patient was given a single oral dose of praziquantel (25 mg/kg) and she improved. This case is presented to emphasize that till date there are very few reports on H.diminuta and there is limited data regarding its treatment protocols (dose and duration). Furthermore, albendazole which is commonly used drug for deworming helminthic infections is less effective in these infections.
Praziquantel, Rat tapeworm, Rodent, Zoonosis
Case Report
An 11-year-old female child presented to the paediatric OPD at AIIMS, Rishikesh with irregular episodes of fever, dull aching abdominal pain and fatigue. Fever was of low grade and it was not associated with chills and rigor. A significant history of pica was present since almost a year and there was no history of loose motions and visible blood or worms in stool. There was no past history of jaundice or bleed from any site. There was a similar episode in the past, two weeks back which was treated as a case of typhoid by some private practitioner, but the symptoms persisted following which she was brought to AIIMS, Rishikesh.
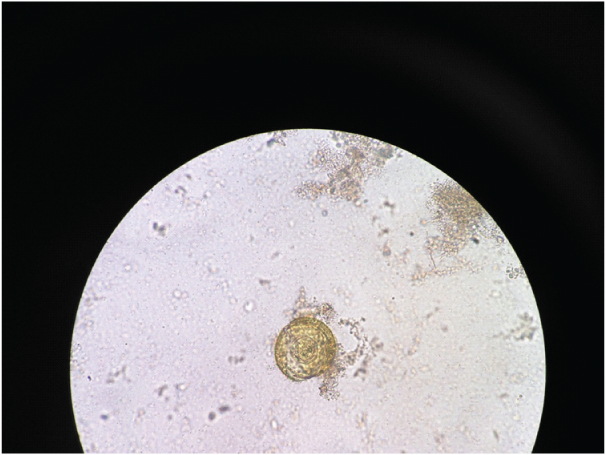
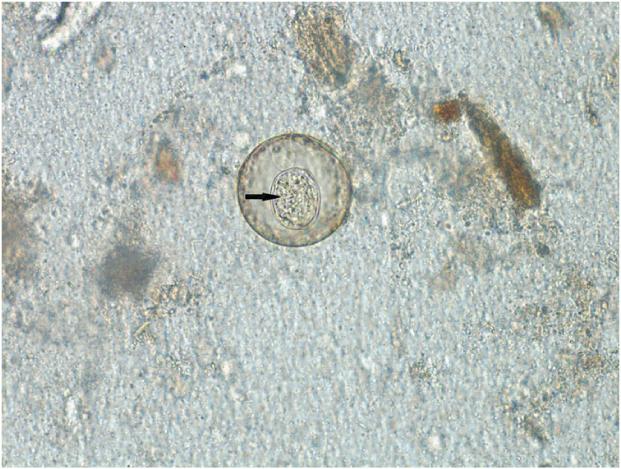
On general examination, mild pallor was present. There was no icterus, lymphadenopathy. Rest of the general examination was insignificant. Systemic examination did not reveal any relevant finding. On investigation, anaemia was present (haemoglobin - 8.6 g/dl) and Total leukocyte count was 8900/cu mm and differential leukocyte count (N65,L30E2M3) was within normal limits. Eosinophilia was not evident. Serum bilirubin (0.1mg/dl), liver enzymes (SGOT-22IU/L, SGPT-42IU/L), serum urea (10.5mg/dl) and creatinine (0.8 mg/dl) were within normal range. Chest X-ray and ultrasound abdomen were also normal. Her urine routine microscopy was normal and culture did not yield any pathogenic bacteria. Her stool routine examination revealed -yellowish brown coloured eggs which were nearly 60-65 micrometre in size with three pair of hooklets, two distinctive sheath and no polar filaments [Table/Fig-1,2]. Since the eggs were bigger in size as compared with eggs of H. nana and there was absence of polar filaments they were further identified as eggs of H. diminuta. Similar picture was seen on repeat stool sample.
Egg of H.dimunita in normal saline mount of stool under 200x magnification.
Egg of H.dimunita in normal saline mount of stool under 400x magnification.
She was prescribed praziquantel single dose of 25mg/Kg along with iron and folic acid tablets. On follow up after two weeks, she was relieved from her symptoms to a great extent and her repeat stool examination was negative for parasitic elements.
Discussion
H. diminuta belongs to kingdom Animalia, Phylum Platyhelminthes, Class Cestoda with genus Hymenolepsis and Species diminuta. It is a rat tapeworm which infects rats and mice. Tapeworm eggs are passed in the rat’s feces and coprophilic arthropods are infected when they eat the eggs which then develop into a cysticercoid stage. The rat gets infected when it eats an infected arthopod, man can similarly be infected accidentally. This tapeworm is more commonly found in areas where large amounts of grain or other dry food products are stored, because they act as food for these arthropods and rodents [1,2]. Though H.diminuta infection in humans is rare it has been reported throughout the world in temperate to tropical conditions of poor sanitation, typically occurring in isolated cases [2–4]. The diagnosis of H diminuta infection is usually accidental while conducting a field survey. Rates of parasitization in different surveys showed to range between 0.001% and 5.5% [2,5,6].
In India Chandler et al., (1927) in their survey reported 23 cases of H. diminuta after examining nearly 10,000 stool samples [7]. Few isolated cases have been reported from the eastern, western and southern parts of India, but till date no case has been reported from Uttarakhand [5–10]. To the best of our knowledge, this is the first case from this part of India.
Cases of infections with H. nana are more frequently seen due to person to person transmission whereas H. diminuta requires an intermediate host for its transmission [1]. Till date, few hundreds of cases of H. diminuta infection in humans have been reported worldwide and are spread due to poor food hygiene and infestation by cockroaches, beetles and rodents [2,3,11]. In our case too, the child probably ingested some arthropod containing the cysticercoid larva.
Almost all the cases have been documented in children who belong to lower socioeconomic status [2,3,5,9,11]. H.diminuta infection is usually asymptomatic but may present with abdominal pain, mild diarrhoea, irritability and pruritis and rash [2,12]. Our case also presented with similar complaints. Usually eosinophilia is seen associated with helminthic infestations but in our case it was not evident and similar finding was noted by Tiwari et al., [5]. A study by Schulte et al., has shown that parasites usually induce high grade blood eosinophilia only during the tissue invasive stages of their development [11,13].
The recommended protocols for treating such helminthic infestations are either praziquantel (10 mg/kg) as a single dose or at a higher dose (25g/kg) for 5 consecutive days or niclosamide in the doses of 1-2 gm given for 5-15 days [4,14]. Due to better safety profile of praziquantel, it was used in single dose in our case. On follow up patient became asymptomatic and stool examination was also negative for parasitic elements.
It may be noted that most deworming prescriptions or programmes use albendazole commonly, however most tapeworms can more effectively be destroyed by praziquental/niclosamide [6].
Conclusion
To conclude, accidental ingestion of food contaminated with arthropods can cause H. diminuta infections in human beings. These infections are not so common but still a matter of concern since commonly used anti helminthic drugs are not effective against cestodes and there is no standardized treatment protocols for them. Thus, each and every case report of H. diminuta infection should be reported along with their clinical presentation and treatment protocols and larger field surveys should be carried out especially in children who have received prior anti helminthic treatment.
[1]. Parija SC, Cestodes: Cyclophyllidean tapewormsTextbook of Medical Parasitology 2013 4th edNew DelhiAll India Publishers and Distributors:212Ch. 11 [Google Scholar]
[2]. Tena D, Pérez Simón M, Gimeno M, Pérez Pomata MT, Illescas S, Amondarain I, Human infection with Hymenolepis diminuta: Case report from SpainJ Clin Microbiol 1998 36:2375-76. [Google Scholar]
[3]. Stafford E, Sudomo M, Marsi S, Brown RJ, Human parasitosis in Bali, IndonesiaSoutheast Asian J Trop Med Public Health 1980 11:319-23. [Google Scholar]
[4]. Patamia I, Cappello E, Castellano-Chiodo D, Greco F, Nigro L, Cacopardo B, A human case of Hymenolepis diminuta in a child from eastern SicilyKorean J Parasitol 2010 48:167 [Google Scholar]
[5]. Tiwari S, Karuna T, Rautaraya B, Hymenolepis diminuta. Infection in a Child from a Rural Area: A Rare Case ReportJournal of Laboratory Physicians 2014 6(1):58-59. [Google Scholar]
[6]. Chai JY, Praziquantel treatment in trematode and cestode infections: an updateInfection & Chemotherapy 2013 45:32-43.doi: 10.3947/ic.2013.45.1.32 [Google Scholar]
[7]. Chandler AC, The distribution of H. diminuta infections in India and discussion of its epidemiological significanceIndian J Med Res 1927 14:973 [Google Scholar]
[8]. Watwe S, Dardi CK, Hymenolepis diminuta in a child from rural areaIndian J Path Microbiol 2008 51:149-50. [Google Scholar]
[9]. Kalaivani R, Nandhini L, Seetha SK, Hymenolepis diminuta infection in a school-going child: A rare case reportAustralas Med J 2014 7(9):379-81. [Google Scholar]
[10]. Sane SY, Irani S, Jain N, Shah KN, Hymenolepis diminuta a rare zoonotic infection report of a caseIndian J Pediatr 1984 51:743-45. [Google Scholar]
[11]. Foresi C, Data on the epidemiology of hymenolepiasis in ItalyArch Ital Sci Med Trop Parasitol 1967 48:251-62. [Google Scholar]
[12]. Schulte C, Krebs B, Jelinek T, Nothdurft HD, Von Sonnenburg F, Loscher T, Diagnostic significance of blood eosinophilia in returning travellersClin Infect Dis 2002 34(3):407-11. [Google Scholar]
[13]. Fryatt RJ, Teng J, Harries AD, Siorvanes L, Intestinal helminthiasis in expatriates returning to Britain from the tropics: a controlled studyTrop Geogr Med 1990 42:119-22. [Google Scholar]
[14]. Tanowitz HB, Weiss LM, Wittner M, Diagnosis and treatment of intestinal helminths. Common intestinal cestodesGastroenterologist 1993 1:265-73. [Google Scholar]