Carcinoma of Maxillary Sinus Masquerading as Odontogenic Infection
Ashir Kolikkal Ramachamparambathu1, Manoj Vengal2, Abdulla Mufeed3, Nizaro Siyo4, Anis Ahmed5
1 Reader, Department of Oral Medicine and Radiology, KMCT Dental College, Calicut (D), Kerala, India.
2 Professor, Department of Oral Medicine and Radiology, KMCT Dental College, Calicut (D), Kerala, India.
3 Reader, Department of Oral Medicine and Radiology, MES Dental College, Perinthalmanna, Malappuram, Kerala, India.
4 Professor, Department of Orthodontics, KMCT Dental College, Calicut (D), Kerala, India.
5 Reader, Department of Oral Medicine and Radiology, Indira Gandhi Institute of Dental Sciences, Kothamangalam, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Abdulla Mufeed, Reader, Department of Oral Medicine and Radiology, MES Dental College, Perinthalmanna, Malappuram, Kerala, India.
E-mail: abmufid@yahoo.co.in
Malignant tumours of maxillary sinus are rare. They are usually diagnosed in the late stages when they perforate the sinus walls. The presence of large air space in the maxillary sinus facilitates asymptomatic growth of the sinus malignancy. The clinical presentation of these tumours depends on the sinus wall involved by the disease. The medial wall is usually the first to become eroded, leading to nasal obstruction, epistaxis or discharge. Rarely, symptoms of maxillary sinus carcinoma can resemble dental infection and the affected patients may visit dental clinic seeking treatment. This report presents a case of carcinoma of maxillary sinus mimicking odontogenic infection. Computed tomographic findings explained the reason for the present lesion to masquerade as an inflammatory condition. The importance of advanced imaging modalities for prompt identification of such lesions is discussed.
Asymptomatic, Computed tomography, Squamous cell carcinoma
Case Report
A 53-year-old male presented at the dental out-patient department with pain and swelling on the right side of the face of one month duration. Pain started after biting hard food on the grossly decayed tooth on the same side. The tooth was extracted for the same reason by a local dentist but the pain aggravated with the development of a swelling in the region. There was no significant response to antibiotics. Patient did not experience any bleeding or discharge from the swelling. The past medical, dental and personal history was unremarkable except for the habit of smoking bidis (A traditional form of tobacco commonly used among villagers in India) for the past 30 years. On examination, a diffuse swelling was evident over the mid face extending superiorly from the lower border of the orbit and inferiorly along the angle of mouth [Table/Fig-1]. The skin over the swelling was erythematous, stretched and shining. The lesion was bony hard in consistency; tender and local temperature was elevated. Intra-orally, the edentulous ridge of maxilla from right canine to right third molar region had healed satisfactorily. However, a diffuse swelling was seen on the slope of the edentulous ridge with obliteration of sulcus in relation to maxillary right second and third molar [Table/Fig-2]. Based on the history and clinical findings, a differential diagnosis of infected residual cyst and chronic osteomyelitis of right posterior maxilla was considered.
Diffuse swelling on the mid-facial region.

Swelling along the edentulous ridge with vestibular obliteration.

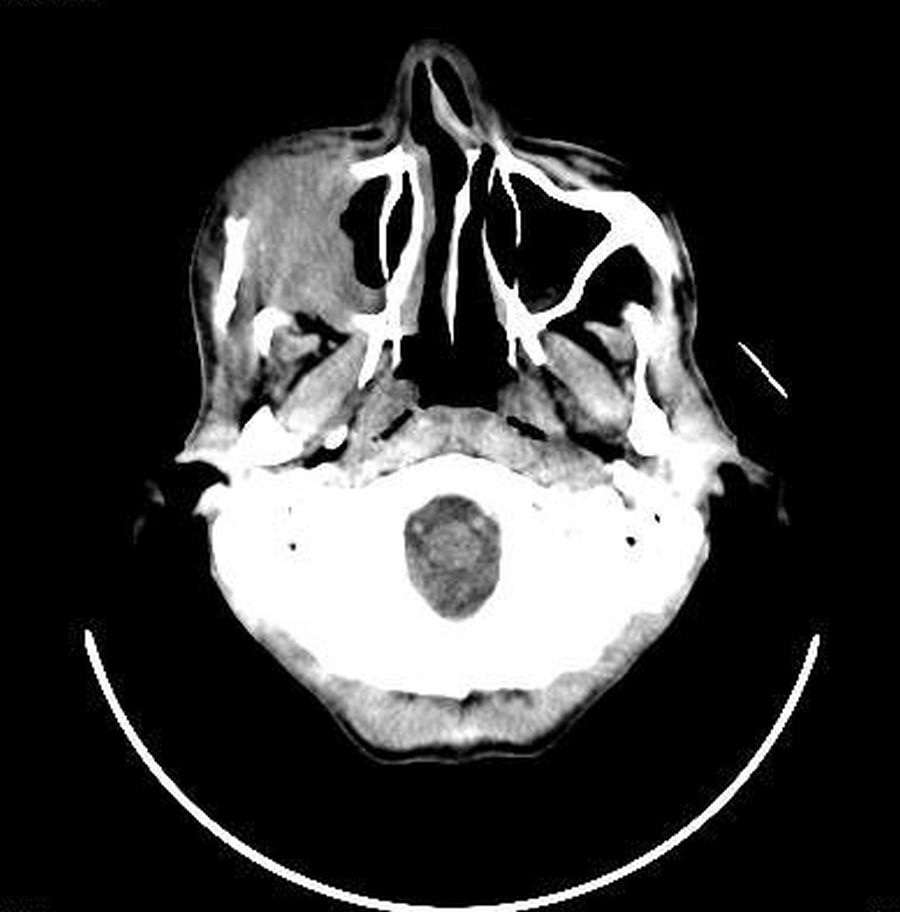
An Intraoral Periapical Radiograph (IOPAR) of the right maxillary posterior region was obtained which showed diffuse radiolucency with loss of continuity of the floor of sinus. Para Nasal Sinus (PNS) view exhibited diffuse haziness of the right maxillary sinus [Table/Fig-3]. Contrast enhanced Computed Tomography scan (CT) revealed lobulated infiltrative soft tissue attenuation mass lesion in the right maxillary sinus causing erosion of the floor, anterior and lateral wall of sinus with extension to maxillary region [Table/Fig-4,5].
Para nasal sinus view showing diffuse haziness of the right maxillary sinus.

Axial CT showing soft tissue infiltration and destruction of bony margins.
The 3D reconstruction showing aggressive bone destruction.

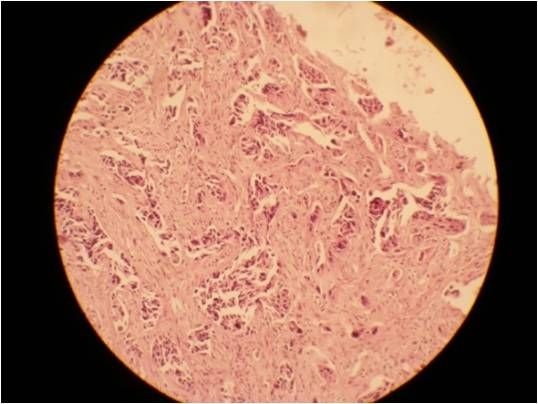
Incisional biopsy of the lesion was performed through intraoral approach and the specimen was subjected to histopathological analysis. Microscopically the sections showed malignant epithelial islands in the superficial connective tissue, the margins showed severe dysplastic epithelium [Table/Fig-6]. A final diagnosis of poorly differentiated Squamous Cell Carcinoma (SCC) of the right maxillary sinus was given.
Histopathology showing malignant epithelial islands in the connective tissues.
Excision of the lesion with partial maxillectomy was perfomed. Patient was discharged with medications and instructions for follow-up. He was advised post-operative radiotherapy.
During the follow-up visits, the patient had significant improvement and had no recurrence. The intra-oral defect was rehabilitated with a palatal obturator.
Discussion
Malignant tumours of maxillary sinus are rare accounting to only 1.5% of all head and neck cancers [1]. Despite of their statistically low incidence, these neoplasms have an overall grave outlook [2]. The most common risk factors for maxillary sinus cancer are smoking and history of chronic sinusitis. Other risk factors including air pollution or occupational exposure to chemical substances, such as formaldehyde, chromium, nickel, have also been found to be associated with an increased risk for the maxillary sinus cancer [3]. Maxillary sinus carcinomas are almost twice as common in men as in women, and nearly 95% occur in patients over the age of 40 years [4]. In a majority of patients, it is diagnosed in the advanced stages [5,6]. The early symptoms of these lesions are inconsistent and are often misdiagnosed as dental infections, chronic sinusitis, nasal polyp or lacrimal gland obstructions [7].
The present case reported with pain in relation to decayed tooth, which aggravated and developed into swelling in the right maxillary region following extraction. Unlike inflammatory lesions of odontogenic origin, carcinoma of maxillary sinus usually presents with epistaxsis, nasal obstruction or discharge, epiphora, diplopia, proptosis, orbital pain and sometimes paraesthesia in case of nerve involvement. When these classic signs are not present, the possibility of a malignant tumour is usually excluded [8,9]. Although the present case was detected in its advanced stage none of above features of carcinoma maxillary sinus was noticed except for non-specific features like pain and swelling.
The conventional radiographs like IOPAR and PNS could not depict the destructive lytic changes associated with the present cancerous mass. On the other hand, CT scan showed a large mass filling the right maxillary sinus causing erosion of the anterior wall, lateral wall and the floor of sinus with extension to maxillary region. The medial wall of sinus was maintained intact.
The reason for delay in clinical symptoms in sinus malignancy is due to the presence of large air space which allows asymptomatic expansion of the tumour [10]. Symptoms are produced only when the malignancy erodes walls of the maxillary sinus. Symptoms depend on the wall perforated by the disease. If the medial wall of the sinus is eroded nasal obstruction, epistaxis or discharge can occur. Cancer causing erosion of the floor produces dental signs and symptoms like unexplained pain, enlargement of alveolar ridge or palate and loose teeth. When the lesion penetrates the lateral wall, facial and vestibular swellings become apparent [11]. Superior extension of the malignancy in the maxillary sinus can result in the displacement or protrusion of the eyeball [11]. Skull base invasion and intracranial extension can cause headache [2]. The CT findings of erosion in the floor and lateral wall of the maxillary sinus explained the reason for the present lesion to mimic odontogenic infection and because of the absence of medial wall involvement the common symptoms of maxillary sinus malignancy were absent.
The site of occurrence of maxillary sinus carcinoma is significant in prognosis and treatment planning. Maxillary sinus can be divided coronally into three zones, suprastructure, mesostructure and infrastructure. Tumours involving mesostructure and infrastructure require partial or total maxillectomy whereas tumours involving suprastructure have poor prognosis and require total maxillectomy. If orbital periosteum is involved orbital exenteration is needed. Ohngren divided the maxillary antrum into posterosuperior and anteroinferior segments by drawing a line on a lateral view of the face from the medial canthus to the angle of the mandible. He suggested that tumours limited to the anterioinferior segment had better prognosis [2,11].
The primary objectives during radiographic examination for maxillary sinus malignancy include visualization of tumour densities, bone destruction, and bone defects so as to determine the extent of carcinoma. "Aggressive bone destruction" is characteristic in patients suffering from SCC [2].
The incidence of lymph node metastasis is low in maxillary sinus carcinoma, but if present it has a poor prognosis. Lymph node involvement was absent in the present case and this can be related to the poor lymphatic drainage of maxillary sinus. However, invasion of the tumour to the adjacent structures with rich lymphatic network, such as the oral cavity and nasopharynx, increases lymph node metastases [7]. Patients with neck metastasis at presentation must undergo a neck dissection. A prophylactic treatment of the neck in patients with N0 (no node involvement) tumours is controversial. A few authors have emphasized the indication for prophylactic neck treatment. On the other hand, some authors drew the opposite conclusion, that it is useless to treat the N0 neck [12,13]. Morphological evaluation of lymph node can be done by Ultrasound, CT and MRI, while PET provides metabolic data of the metastatic lymphnodes. CT-PET has shown to have a high sensitivity in diagnosing the primary tumour and regional lymph node metastases. CT with contrast is superior for the evaluation of the bony walls of the maxillary sinus and skull base. The estimation of the tumour vascularity and its relation to the carotid artery can also be done with contrast CT. MRI is superior in distinguishing tumour from adjacent inflammatory disease [2,14]. However, micrometastases, if present cannot be diagnosed by the above methods [12,13]. With improved imaging technology and superior tumour mapping permits more realistic treatment planning with regard to cure versus palliation.
Surgery remains the primary treatment modality, combined chemotherapy and radiation therapy has a significant role in patients with advanced disease [15]. A majority of maxillary sinus tumours are diagnosed in their advanced stage, leading to poorer prognosis. The complexity of the anatomy of the maxillary sinus and its proximity to vital structures like eyes, brain, and cranial nerves makes the complete surgical removal challenging, which can lead to treatment failure. The other issues in the treatment of maxillary sinus cancer include the functional aspects such as eyesight and the cosmetic aspects, which make patients reluctant for surgical resection [6]. In the present case, a combination of surgery and post-operative radiotherapy with reconstruction for function and aesthetics was considered as the treatment.
Conclusion
Maxillary sinus carcinomas are rare but have a poor prognosis due to the delay in diagnosis and limitations in the treatment due to the close proximity of sinus to the vital structures. The delay in diagnosis may be attributed to the fact that the clinical signs and symptoms of carcinoma of maxillary sinus may masquerade an inflammatory condition. The clinical presentation depends on maxillary sinus wall through which it progreses. Early identification of clinically silent malignant neoplasms of sinuses requires advanced imaging modalities.
[1]. Ashraf M, Biswas J, Dam A, Bhowmick A, Jha JK, Sing V, Results of treatment of squamous cell carcinoma of maxillary sinus: A 26-year experienceWorld J Oncol 2010 1:28-34. [Google Scholar]
[2]. Som PM, Brandwein M, Sinonasal cavities. Tumours and tumour like conditions. In: Som PM, Hugh D, editorsHead and neck imaging 2003 4th edSt. LouisMosby Year Book:262-71. [Google Scholar]
[3]. Won HS, Chun SH, Kim B, Chung SR, Yoo IR, Jung CK, MS, JH. Treatment outcome of maxillary sinus cancerRare Tumours 2009 1(2):e36 [Google Scholar]
[4]. Santos MR, Servato JP, Cardoso SV, De Faria PR, Eisenberg AL, Dias FL, Squamous cell carcinoma at maxillary sinus: clinicopathologic data in a single Brazilian institution with review of literatureInt J Clin Exp Pathol 2014 7(12):8823-32. [Google Scholar]
[5]. Bhattacharyya N, Factors affecting survival in maxillary sinus cancerJ Oral Maxillofac Surg 2003 61:1016-21. [Google Scholar]
[6]. Manrique RD, Deive LG, Uehara MA, Manrique RK, Rodriguez JL, Santidrian C, Maxillary sinus cancer review in 23 patients treated with postoperative radiotherapyActa Otorrinolaringol 2008 59(1):6-10. [Google Scholar]
[7]. Vasudevan V, Kailasam S, Radhika MB, Venkatappa M, Devaiah D, Shrihari TG, Well-differentiated squamous cell carcinoma of maxillary sinusJournal of Indian Academy of Oral Medicine and Radiology 2012 24(3):250-54. [Google Scholar]
[8]. Hone SW, O’Leary TG, Maguire A, Burns H, Timon CI, Malignant sinonasal tumours: The Dublin Eye and Ear Hospital experienceIr J Med Sci 1995 164(2):139-41. [Google Scholar]
[9]. Selden HS, Manhoff DT, Hatges NA, Michel RC, Metastatic carcinoma to the mandible that mimicked pulpal/periodontal diseaseJ Endod 1998 24(4):267-70. [Google Scholar]
[10]. Dulguerov P, Jacobsen MS, Allal AS, Lehmann W, Calcaterra T, Nasal and paranasal sinus carcinoma: Are we making progress?Cancer 2001 92(12):3012-29. [Google Scholar]
[11]. St. Pierre S, Baker S, Squamous cell carcinoma of the maxillary sinus: analysis of 66 casesHead and Neck Surg 1983 5:508-13. [Google Scholar]
[12]. Kazi M, Awan S, Junaid M, Qadeer S, Hassan NH, Management of sinonasal tumours: prognostic factors and outcomes: a 10 year experience at a tertiary care hospitalIndian J Otolaryngol Head Neck Surg 2013 65(1):S155-59. [Google Scholar]
[13]. Cantu G, Bimbi G, Miceli R, Mariani L, Colombo S, Riccio S, Lymph node metastases in malignant tumours of paranasal sinusesArch Otolaryngol Head Neck Surg 2008 134(2):170-77. [Google Scholar]
[14]. Tian L, Li YZ, Mo YX, Liu LZ, Xie CM, Liang XX, Nasopharyngeal carcinoma with paranasal sinus invasion: the prognostic significance and the evidence-based study basis of its T-staging category according to the AJCC staging systemBMC Cancer 2014 14:832 [Google Scholar]
[15]. Al-Zaabi K, Al Riyami M, Al-Abri R, A unilateral maxillary sinus tumourOman Med J 2013 28(3):220-21. [Google Scholar]