Coronary Artery Disease (CAD) is a major cause of mortality and morbidity worldwide. With epidemiologic, demographic and health transition, India is facing problems with both communicable as well as non communicable diseases. In the most productive age group of 25-69, cardiovascular disease is the leading cause of death responsible for 25% of all deaths in males as well as females across the country [1].
The surge in the CAD to epidemic levels can be controlled and decreased by control of well established modifiable risk factors like smoking, alcohol, physical inactivity, low consumption of fruits and vegetables, overweight and obesity, increased blood pressure, impaired fasting glucose and dyslipidaemia [2,3].
Until now maximum data are from western countries regarding CAD. The health status of Purvanchal area of Uttar Pradesh, India is different from other states of India as this area is more backward with less health awareness and more poverty. It is important to study the patient characteristics, risk factors and presentation of patients with ACS to provide data unique to this region that will help to improve primary, secondary as well as tertiary preventive efforts and to address problems unique to Indian population. With no studies reported from this region in naïve patients presenting for first time with acute coronary syndrome and a billion plus population in this country it is important to have large registries and data analysis. This study was therefore undertaken with the following aims and objectives:
Materials and Methods
Design: Prospective, observational, descriptive, cohort study.
Setting: An academic tertiary care centre hospital with interventional cardiac care unit.
Duration: Study was conducted from March 2012 to April 2013.
Inclusion Criteria
All patients fulfilling diagnostic criteria for ACS and exclusion criteria.
Age ≥ 18 years.
Genders-both sexes
Diagnostic criteria for ACS
It includes STEMI, NSTEMI or unstable angina (UA).
Cases of chest pain/ discomfort with elevation of ST segment in Electrocardiogrphic (ECG) leads/presumed new onset Left Bundle Branch Block (LBBB) in ECG, were categorized as STEMI.
Cases of angina at rest without ST segment elevation were categorized as NSTEMI if their cardiac Troponin T (Trop T) levels exceeded 0.1 nanogram/ml and as UA if their Trop T levels were lower.
Angina that occurred at rest and was prolonged, usually lasting ≥10 min consistent with pain or discomfort of myocardial ischemic origin.
ECG criteria for STEMI
New or presumed new ST-segment elevation, new LBBB, or isolated inferobasal (posterior) MI.
ST-segment elevation at the J point in two contiguous leads with the cutpoints ≥ 0.1 mv in all leads other than V2/ V3, where ≥ 0.2 mV in men age ≥ 40 y, ≥ 0.25mV in men age <40 y, or ≥ 0.15 mV in women.
ST-segment depression ≥ 0.1 mV in at least two contiguous leads of V1 through V3 with upright T waves.
ST-segment elevation ≥ 0.05 mV in leads V7 through V9 or ≥ 0.1 mV in men age < 40 y (inferobasal {posterior} infarction).
ST-segment elevation ≥ 0.05 mV (≥ 0.1 mV in men age <30 y) in leads V3R, V4R (right ventricular infarction).
ST-segment elevation ≥ 0.1 mV in lead a VR with concomitant ST-segment depression ≥ 0.05 my in at least two contiguous leads.
Exclusion Criteria
Any history or records of, or suggestive of, previous angina, angina equivalent or MI or coronary revascularisation (more than two weeks old).
Patients with prior cardiac pathology like valvular heart disease, cardiomyopathy, pericardial disease or cor pulmonale.
Patients who did not undergo angiography.
Study Details: Only those patients were included in the study cohort who fulfilled the inclusion and exclusion criteria. Detailed history was taken. Structured questionnaires were administered and physical examinations were undertaken. The baseline clinical characteristics analysed in each group were the age, gender, hypertension, diabetes mellitus, dyslipidemia, smoking status, personal and family history of cardiovascular history, duration of chest pain before hospitalization, time of occurrence of the ACS, symptoms, Killip class and treatment received. Body mass index was calculated any time before discharge. Echocardiography was done at the time of admission with bed side echocardiogram machine (Sonosite).
The details of the area of myocardium infarcted, the Killip class, complications and whether thrombolytic therapy was received or not were analysed.
Angiographic findings were noted. Persons doing and reporting angiography were not aware of the process and thus blinded to the study. Coronary artery with more than 50% of occlusion was taken as significant.
A comparison of clinico-investigational parameters was done
between males and females
between STEMI and NSTEMI/ UA
between diabetics and non-diabetics
Ethical considerations - As the study was observational and descriptive and involved no intervention, the ICU and patient data were collected with the usual guarantees of confidentiality.
Statistical Analysis
Statistical analysis was done using patient related variables as well as process of care variables. Patient related variables included age, gender, and diagnosis at the time of hospital admission, signs and symptoms, associated risk factors, Killip class while process of care variable included investigation parameters like lipid profile, electrocardiogram, echocardiography and angiography.
The above mentioned factors were evaluated in both groups STEMI and NSTEMI. Patient characteristics and process of care variables were compared gender wise, in diabetics and number of coronary vessel involvement.
The data was studied and statistically treated. The univariate analysis was done using chi-square/fischer’s test. Results between two groups were compared using unpaired t-test. Test of significance was set <0.05.
Terminologies
Acute MI - Evidence of myocardial necrosis in a clinical setting consistent with myocardial ischemia.
Detection of the rise and/or fall of cardiac biomarkers (preferably cTn) with at least 1 value above the 99th percentile and with at least one of the following symptoms of ischemia [4].
New or presumed new significant ST-T changes or new LBBB.
Development of pathological Q waves on the ECG.
Imaging evidence of new loss of viable myocardium or new regional wall motion abnormality.
Identification of an intracoronary thrombus by angiography or autopsy.
Prior Angina- If angina existed for more than two weeks before admission.
Diabetes- History of diabetes diagnosed and/or treated by a healthcare provider.
Documentation of Haemoglobin Alc ≥ 6.5%; or
Fasting plasma glucose ≥ 126mg/dl or 2-h plasma glucose ≥200 mg/dL during an oral glucose tolerance test; or a patient with classic symptoms of hyperglycaemia or hyperglycaemic crisis, a random plasma glucose ≥ 200mg/dl.
Hypertension- History of hypertension diagnosed and treated with medication, diet and/or exercise or prior documentation of blood pressure ≥ 140mmHg systolic and/or 90mmHg diastolic for patients without diabetes or chronic kidney disease, or prior documentation of blood pressure ≥ 130mmHg systolic or 80mm Hg diastolic on at least two occasions for patients with diabetes or chronic kidney disease or currently undergoing pharmacological therapy for treatment of hypertension.
Dyslipidemia- Total cholesterol >200 mg/dL or LDL ≥ 130 mg/dL or HDL <40 mg/dL in men and <50 mg/dL in women or currently receiving antilipidemic treatment.
Killip Class
Class 1: absence of rales over the lung fields and absence of S3.
Class 2: rales over ≤ 50 % of the lung fields or the presence of an S3.
Class 3: rales over >50% of the lung fields.
Class 4: shock.
Results
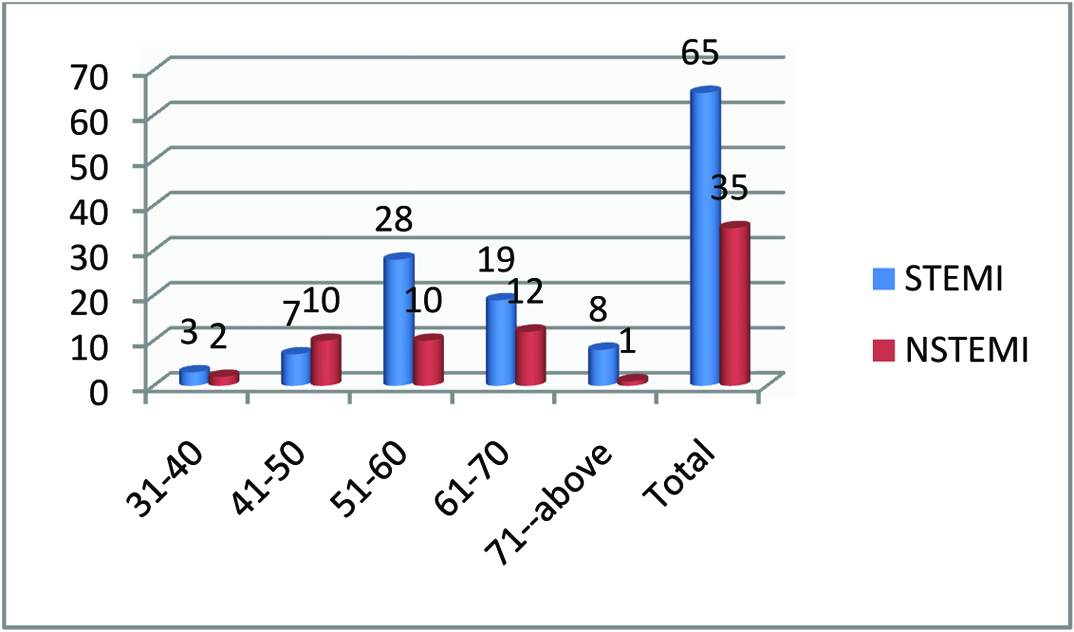
In the present study, 100 patients with ACS were analysed. Patients were divided into two categories as STEMI and NSTEMI. Of the total 65% of the patients presented with STEMI and 35% patients presented with NSTEMI.
Mean age of presentation was 58.9 years. A total of 69% patients were in the age group of 51-70 years, 27% patients were in the younger age category i.e., below 50 y of age. [Table/Fig-1] shows the age distribution among STEMI and NSTEMI subgroups.
There was a preponderance of males with 75% patients were males and 25% were females. Median time to reach hospital was 24 hours. A 27% of patients reached hospital early within 6 hours whereas 39% patients reached after 24 hours. Patients with STEMI presented earlier as compared to patients in NSTEMI group which was statistically significant (p-0.08). In the NSTEMI group 51.4% patients presented after 24 hours whereas in STEMI 32.3% came to hospital after 24 hours [Table/Fig-2].
Duration from symptom onset to hospitalisation.
| Duration (hours) | STEMI (n=65) | NSTEMI (n=35) |
|---|
| 0-6 | 22 (33.8%) | 5 (14.3%) |
| 6-12 | 6 (9.2%) | 5 (14.3%) |
| 12-24 | 16 (24.6%) | 7 (20%) |
| >24 | 21 (32.3%) | 18 (51.4%) |
Out of 65 patients presenting with STEMI 28, received fibrinolytic therapy with average duration of 7.2 hours. In these 57% patients did not receive thrombolytic therapy due to delayed presentation in most patients. Reasons for delayed presentation were atypical symptoms, negligence on part of patient or family, long distance from health care facility, non availability of medication and delayed referral from primary care practitioner.
Risk Factors
The [Table/Fig-3,4] show the distribution of various risk factors studied. The distribution of the risk factors was not significantly different in the two groups. Twenty one patients were obese with BMI more than 30. Mean LDL was low, triglycerides were high and HDL was low in both subgroups but there was no statistical difference. Also, presence of elevated BMI was not statistically different between STEMI and NSTEMI.
Distribution of risk factors between STEMI vs NSTEMI.
| Risk factor | STEMI (n=65) | NSTEMI (n=35) | p-value |
|---|
| Diabetes mellitus | 16 (24.6%) | 7 (20%) | 0.17 |
| Hypertension | 13 (20%) | 8 (22.9%) | 0.18 |
| Smoking | 11 (16.9%) | 5 (14.3%) | 0.21 |
| Family history | 7 (10.8%) | 4 (11.4%) | 0.25 |
| STEMI (mean+/- SD) | NSTEMI (mean+/- SD) | p-value |
|---|
| BMI | 27.69 +3.50 | 26.34+3.17 | 0.33 |
| Triglycerides | 150.57+52.92 | 160.91+74.49 | 0.12 |
| LDL | 115.77+35.06 | 114.14+30.19 | 0.19 |
| HDL | 39.71+9.26 | 39.97+10.76 | 0.34 |
| Total cholesterol | 185.22+42.50 | 185.86+38.41 | 0.44 |
Symptoms
[Table/Fig-5] shows the distribution of symptoms in patients presenting with STEMI and NSTEMI.
Distribution of symptoms in patients presenting with STEMI and NSTEMI.
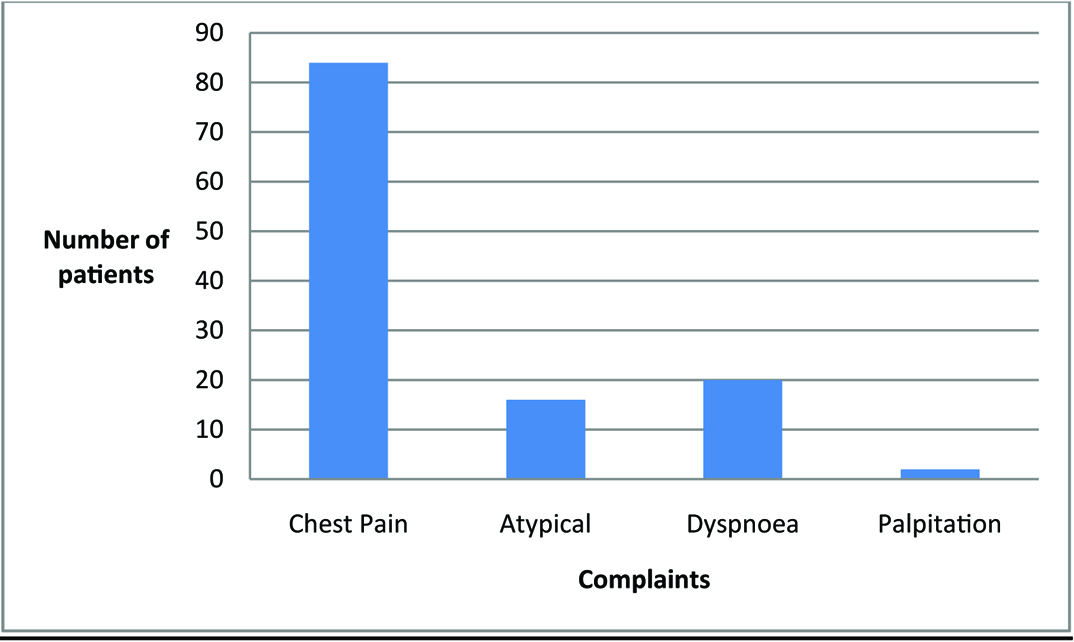
Atypical complaints included radiation of chest pain to atypical sites like right side of chest and abdomen, fatigue and feeling of weakness and feeling of suffocation without chest pain. Classical angina showed increased trend in patients with STEMI with a p-value 0.08 with more patients in NSTEMI having atypical complaints.
Distribution of Coronary Vessels Involvement
Overall 47% patients had single vessel disease, 33% had double vessel disease and 20% had all three major coronary vessels involved. Patients with NSTEMI were associated with more severe disease with 31.4% of patients having triple disease in contrast to 13.8% having triple vessel disease in STEMI group. The difference was statistically significant with a p-value of 0.03 [Table/Fig-6].
Coronary vessel involvement on coronary angiography.
| Number of vessels on coronary angiogram | STEMI (n=65) | NSTEMI (n=35) |
|---|
| Single vessel disease | 32 (49.2%) | 15 (42.9%) |
| Double vessel disease | 24 (36.9%) | 9 (25.7%) |
| Triple vessel disease | 9 (13.8%) | 11 (31.4%) |
[Table/Fig-7,8] shows the distribution of coronary vessel involvement with age and sex. Younger patients had predominantly single vessel disease with a trend towards multivessel involvement with increasing age. There was a significant association of age with number of vessels involved (p=0.023). Similarly female sex was also associated with more extensive disease on angiography (p=0.04)
Coronary vessel involvement on coronary angiography with age.
| Number of vessels on coronary angiogram | 31-40 y | 41-50 y | 51-60 y | 61-70 y | 71-above y |
|---|
| Single vessel disease | 4 (8.5%) | 9 (19.1%) | 19 (40.4%) | 12 (25.5%) | 3 (6.4%) |
| Double vessel disease | 0 (0%) | 4 (12.1%) | 13 (39.4%) | 12 (36.4%) | 4 (12.1%) |
| Triple vessel disease | 1 (5%) | 4 (20%) | 6 (30%) | 7 (35%) | 2 (10%) |
Coronary vessel involvement on coronary angiography with sex.
| Number of vessels on coronary angiogram | Male | Female |
|---|
| Single vessel disease | 38 (80.9%) | 9 (19.1%) |
| Double vessel disease | 24 (72.7%) | 9 (27.3%) |
| Triple vessel disease | 13 (65%) | 7 (35%) |
LV Systolic Function
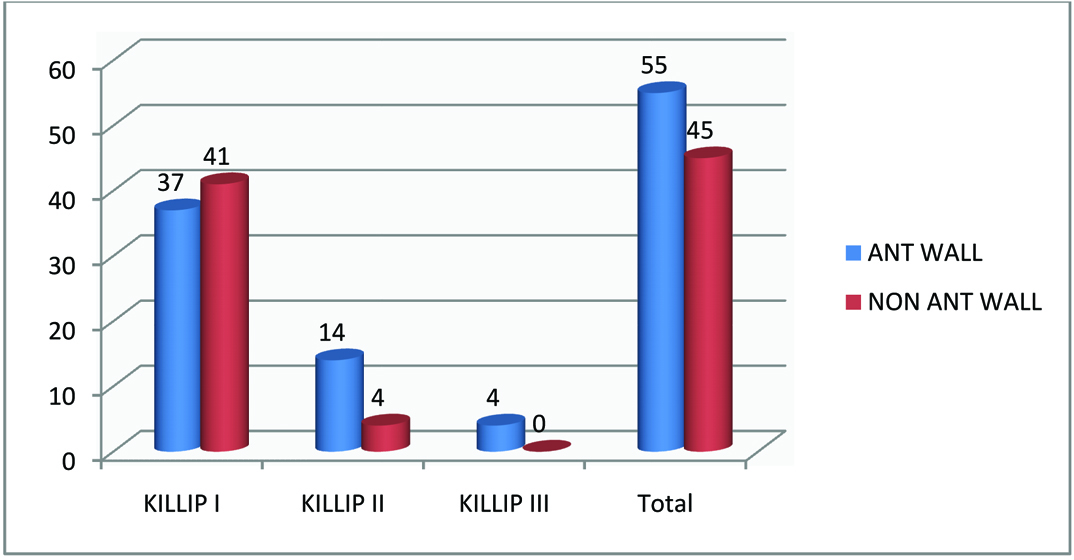
Moderate to severe LV dysfunction was seen in 38.5% patients with STEMI while in NSTEMI group only 20% had moderate to severe LV dysfunction. While only 3.1% patients in STEMI group had normal LV function, in NSTEMI group 34.3% patients had preserved LV ejection fraction. Patients presenting with anterior wall regional wall abnormality had more severe Killip class as compared to non anterior wall involvement [Table/Fig-9].
Patients presenting with anterior wall regional wall abnormality had more severe Killip class as compared to non anterior wall involvement.
Diabetic Sub-population
Diabetics had a significant delay in presentation with a p-value 0.003 with 56.5% of diabetics presenting after 24 hours. Only 4.3% patients had preserved ejection fraction post ACS. Maximum number of patients had mild to moderate LV dysfunction. The result was significant as shown by p-value. As compared to non diabetics triple vessel disease was more associated with diabetes with a p-value of 0.01 [Table/Fig-10].
Characteristics in diabetics versus non diabetics.
| | Diabetic (n=23) | Non diabetic (n=77) | |
|---|
| Duration of presentation | < 6 hours | 2 (8.7%) | 25 (32.5%) | p=0.003 |
| 6-12 hours | 2 (8.7%) | 9 (11.7%) |
| 12-24 hours | 6 (26.1%) | 17 (22.1%) |
| >24 hours | 13 (56.5%) | 26 (33.8%) |
| LV systolic function | >55% | 1 (4.3%) | 13 (16.9%) | p=0.024 |
| 45-55% | 9 (39.1%) | 32 (41.6%) |
| 31-44% | 12 (52.2%) | 32 (41.6%) |
| <30% | 1 (4.3%) | 0 (0%) |
| Number of coronary vessels involved | Single vessel disease | 8 (34.8%) | 39 (50.6%) | p=0.01 |
| Double vessel disease | 6 (26.1%) | 27 (35.1%) |
| Triple vessel disease | 9 (39.1%) | 11 (14.3%) |
Discussion
This is one of the first reported studies on ACS from the Purvanchal area of Uttar Pradesh. We recorded more cases of STEMI than non-STEMI or UA with longer delays before admission to hospital. About 65% of patients in this study had STEMI which is in contrast to western reports including the European Heart Surveys where non-STEMI predominates [5–7]. However, few Indian studies have documented predominance of STEMI in ACS [8–10].
Mean age of the patients in our study was 58.9 years which is 5 years earlier than western studies [6,7]. However this is consistent with other Indian studies which support the finding that Indians get Coronary Artery Disease (CAD) earlier by 5-10 years [8–10]. The mean age in the CREATE registry was 57 years while that in the Kerala registry was 60.4 years [8,9].
Our study showed that patients with STEMI took longer to reach hospital with a median of 24 hours. The median time taken by patients is much higher than reported in other registries [6,7]. One study however reported the mean duration of symptoms before hospitalisation in STEMI patients of 11.37 hours [11]. Patients with non-STEMI presented still later to hospital with a statistically significant difference as compared to STEMI patients. Lack of ambulance with long distance from health care facility in peripheral locations, economic reasons, a lack of awareness of the importance of the symptoms, delay by local practitioner and non availability of medication were the reasons for delayed presentation.
In our study out of 65 patients with STEMI, 43% received thrombolysis. This is low as compared to other Indian studies [8]. However one study from north eastern India reported about 40% use of reperfusion therapy in STEMI patients [12]. One of the main reasons for high proportion of non thrombolysis was delayed presentation. A total of 32.3% patients in the STEMI group presented after 24 hours. Variations in the thrombolysis rates across India could indicate the lack of access to healthcare and economic conditions of that region.
Presence of at least one risk factor was seen in 54% of patients in our study. This is no surprise as INTERHEART study investigators concluded that abnormal lipids, smoking, hypertension, diabetes, abdominal obesity, psychosocial stress, decreased consumption of fruits and vegetables, moderate consumption of alcohol, and physical activity accounted for most of the risk of myocardial infarction worldwide collectively accounting for 90% of the Population Attributable Risk (PAR) in men and 94% in women [13]. The prevalence of diabetes and hypertension is lower as compared to other Indian studies [14]. Tobacco smoking is a known modifiable risk factor for CAD. In our study 16% patients were smokers. This is lower as compared to other Indian studies because of more incidence of tobacco chewing in this part of Uttar Pradesh. A total of 21% patients were obese with BMI more than 30. This prevalence is less as compared to INTERHEART South Asian cohort where they used waist: hip ratio to calculate obesity prevalence [13]. Mean LDL was low, triglycerides were high and HDL was low in both subgroups but there was no statistical difference. Similar lipid levels have been reported in other Indian studies. The lower HDL-C and higher triglyceride levels in both younger and older cases is seen in Indian population [15,16].
Among the risk factors there was no significant association of Diabetes Mellitus (DM), hypertension, smoking, lipid level or obesity for a particular group between STEMI vs NSTEMI. This is in contrast to other studies where they are more associated with NSTEMI [10]. This difference may be because we had not included any patient with prior angina or myocardial infarction in our study.
Single vessel involvement was most prevalent in both STEMI and NSTEMI groups similar to other studies [17,18]. Patients with NSTEMI had more severe disease on angiography with 31% of patients with NSTEMI having triple vessel disease. High incidence of multivessel disease has been observed in TACTICS-TIMI 18 study [19].
Atypical symptoms were more prominent in NSTEMI group. Patient presenting with STEMI had more LV dysfunction as compared to NSTEMI. Similar findings were seen in CREATE study and GRACE study groups [5,8].
Diabetic patients in our study were equally distributed in STEMI and NSTEMI subgroups. Diabetics had more atypical chest pain, more severe LV dysfunction and had trend towards positive family history of diabetes or cardiovascular disease. Hypertension was significantly associated with diabetes.
On angiography factors favouring or showing significant association with Triple vessel disease were female sex, higher age and presence of diabetes. Studies have shown high incidence of multivessel disease depending on baseline characteristics of the specific population especially diabetics [20,21].
Limitation
This study was a single centre study where patients were randomly selected. Due to single centre nature of study the practice patterns not necessarily represent practice at all hospitals in the country. However, the study is unique in the sense that no patient with prior coronary disease was included in this study. Second, one-month follow-up data were not available. We did not calculate 30 day mortality to assess survival difference. In many patients lipid profile was done after 48 hours which might have caused lower level of HDL and LDL cholesterol in this study.
Conclusion
Patients with ACS in India tend to be of younger age as compared to western countries. Patients with ACS have a higher rate of STEMI.
ACS was more common in males, both STEMI and NSTEMI; however female sex was associated with more vessel involvement.
More than 50% of patients had at least one risk factor among studied.
Less than 50% patients received thrombolytic treatment which calls for immediate attention toward CAD at community level.
Patient with anterior wall involvement had worse Killip score as well as myocardial dysfunction.
NSTEMI was associated with more severe coronary disease with more triple Vessel involvement.
NSTEMI patient presented late as compared to STEMI.
Diabetics had more severe disease and more LV dysfunction even though they had no prior history of angina or angina equivalent.
For a large populated country like India risk factors modification has the potential to prevent most premature cases of MI worldwide.