Direct laryngoscopy and laparoscopic cholecystectomy leads to haemodynamic stress responses in the form of tachycardia and hypertension. Plasma concentration of catecholamines increases [1] and there may be associated myocardial ischemia and cerebral haemorrhage [2]. Premedication in the form of vasodilators [3], adrenoreceptor blockers [4], calcium channel blockers [5,6] and opioids [7–10] were used earlier to attenuate these responses, with variable results.
Clonidine is an α-2 adrenoreceptor agonist with central sympatholytic effect. Premedication with clonidine blunts the haemodynamic stress responses to direct laryngoscopy and tracheal intubation. Clonidine also stabilizes blood pressure by increasing cardiac baroreceptor reflex sensitivity [11].
Pregabalin, a gabapentinoid compound appears to produce an inhibitory modulation of neuronal excitability particularly in neocortex, amygdala and hippocampus of CNS [12]. It possess analgesic, anticonvulsant and anxiolytic activity by reduction of neurotransmitter glutamate, nor-adrenaline, serotonin, dopamine and substance P [13].
The present study was designed as prospective, randomized, double blind clinical study to find out and compare efficacy of oral premedication with pregabalin 150mg and clonidine 0.3mg in attenuation of stress response of direct laryngoscopy and tracheal intubation.
Materials and Methods
The study was carried out over a period of one year from April 2013 to March 2014. Prior to commencement of the study ethical clearance was obtained from institutional ethical committee. Patients undergoing elective laparoscopic cholecystectomy were screened for eligibility and a written informed consent was obtained from the selected patients. This prospective, double blind, randomized study consisted of 80 patients aged between 20 to 60 years of either sex with ASA grade I and II.
Patients with severe systemic disorder like IDDM, uncontrolled hypertension, kidney or liver disease, severe respiratory disorder, seizure disorder, coronary artery disease or recent history of MI, concomitant use of TCA, SSRI, MAO inhibitors or opioids, patients who were taking pregabalin or gabapentine, patients with known hypersensitivity or allergy to pregabalin or clonidine or any other drug to be used, anticipated difficult airway, body weight >100 kg or obese and pregnant or breast feeding females were excluded from the study.
All the patients were randomly divided into two groups of 40 each using a computer generated random number table. Group A received 0.3mg (300μg) clonidine orally 60 min before surgery and group B received 150mg pregabalin orally 60 min before surgery. The study drugs containing clonidine and pregabalin were prepared and administered in a double blind fashion. Prior to surgery preanaesthetic evaluation was done including detailed history and examination of cardiovascular, respiratory and central nervous system. Airway examination was done for possibility of difficult intubation. The patients with anticipated difficult airway were excluded from the study. All the findings of history and examination were recorded on a predesigned and pretested proforma.
Routine investigations like complete blood counts, urine routine and microscopy, blood urea nitrogen, serum creatinine, fasting and post prandial blood sugar, x-ray chest PA view and ECG were done.
All patients were explained about the anaesthesia technique and written informed consent was taken. Patients were kept NPO 8 hours prior to surgery. Alprazolam 0.25mg tab. was given to all patients night before surgery.
In the morning of surgery NPO status was confirmed and patients were taken in the pre-anaesthetic room. Patient’s blood pressure both Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) and heart rate were recorded. The patients were randomly assigned into two groups. They received a coded oral preparation containing clonidine (0.3mg) or pregabalin (150mg). Group A received clonidine (0.3mg) whereas group B received pregabalin (150 mg) by the nursing staff with a sip of water, 60 minutes before the expected time of induction of anaesthesia.
In the operating room multipara monitor with ECG, NIBP, pulse oximetry were applied. Blood pressure (systolic, diastolic and mean) was obtained by noninvasive brachial oscillometry and heart rate was recorded from ECG (lead II) 5 min after the patient was placed on the operating table. Rhythm monitoring from a continuous visual display of ECG along with continuous monitoring of vital parameters were done. The level of sedation of patients was evaluated and was graded by Ramsey sedation score.
I.V. fentanyl 1 μg/kg was given. Pre-oxygenation was done for 3 minutes, then induction was done with i.v propofol 2 mg/kg followed by administration of i.v.vecuronium 0.1mg/kg to facilitate tracheal intubation. From the time of administration of propofol ventilation was controlled manually by Bain’s circuit using 100% oxygen. Blood pressure (systolic, diastolic and mean) and heart rate were recorded after giving i.v. drugs prior to laryngoscopy. Laryngoscopy and tracheal intubation was performed by an experienced anaesthesiologist and accomplished within 20 seconds with appropriate sized, cuffed endotracheal tube, 3 minutes after giving vecuronium. In case of unexpected difficult intubation the patient was excluded from the study.
BP (SBP, DBP and MAP) and heart rate were recorded immediately after intubation, then at 1 min, 3 min, 5 min, 10 min and 15 min after intubation.
Anaesthesia was maintained with minimum alveolar concentration (MAC) of 0.75% halothane and nitrous oxide 50% in oxygen. The patients’ lungs were mechanically ventilated with minute ventilation adjusted to maintain normocapnia (EtCO2 between 35 to 40mm Hg). Supplemental neuromuscular blockade was achieved with vecuronium 0.02 mg/kg to maintain relaxation.
Hypotension primarily was treated by increasing the intravenous infusion rate and additionally with i.v. mephenteramine 6mg. Bradycardia, defined as heart rate slower than 60 beats/min, was treated with i.v. atropine 0.3-0.6mg.
Halothane was discontinued at the end of surgery and residual neuromuscular block was antagonized with appropriate doses of neostigmine (0.05 mg kg-1) and glycopyrrolate (0.01 mg kg-1) after evaluating with peripheral nerve stimulator, when at least two responses to train of four stimulation were present. Following confirmation of recovery from anaesthesia and muscle relaxation, extubation was performed after thorough suctioning.
Level of sedation and postoperative pain score was assessed and patients were shifted to post anaesthesia care unit. Intramuscular diclofenac 75 mg was given whenever required for postoperative pain. Patients were observed for 2 hours for nausea, vomiting, bradycardia, hypotension, sedation and other side effects and then shifted to the ward. Any complications like dizziness, somnolence, diplopia, vomiting, confusion, pain, nausea and urinary retention were recorded and treated in first 24 hours postoperative period.
The statistical analysis was done using SPSS (Statistical Package for Social Sciences) Version 15.0 statistical Analysis Software. The values were represented in Number (%) and Mean±SD.
Results
All the patients in both groups were comparable with respect to demographic profile (age, gender and body weight) and no statistically significant difference in baseline haemodynamic variables of both the groups was found.
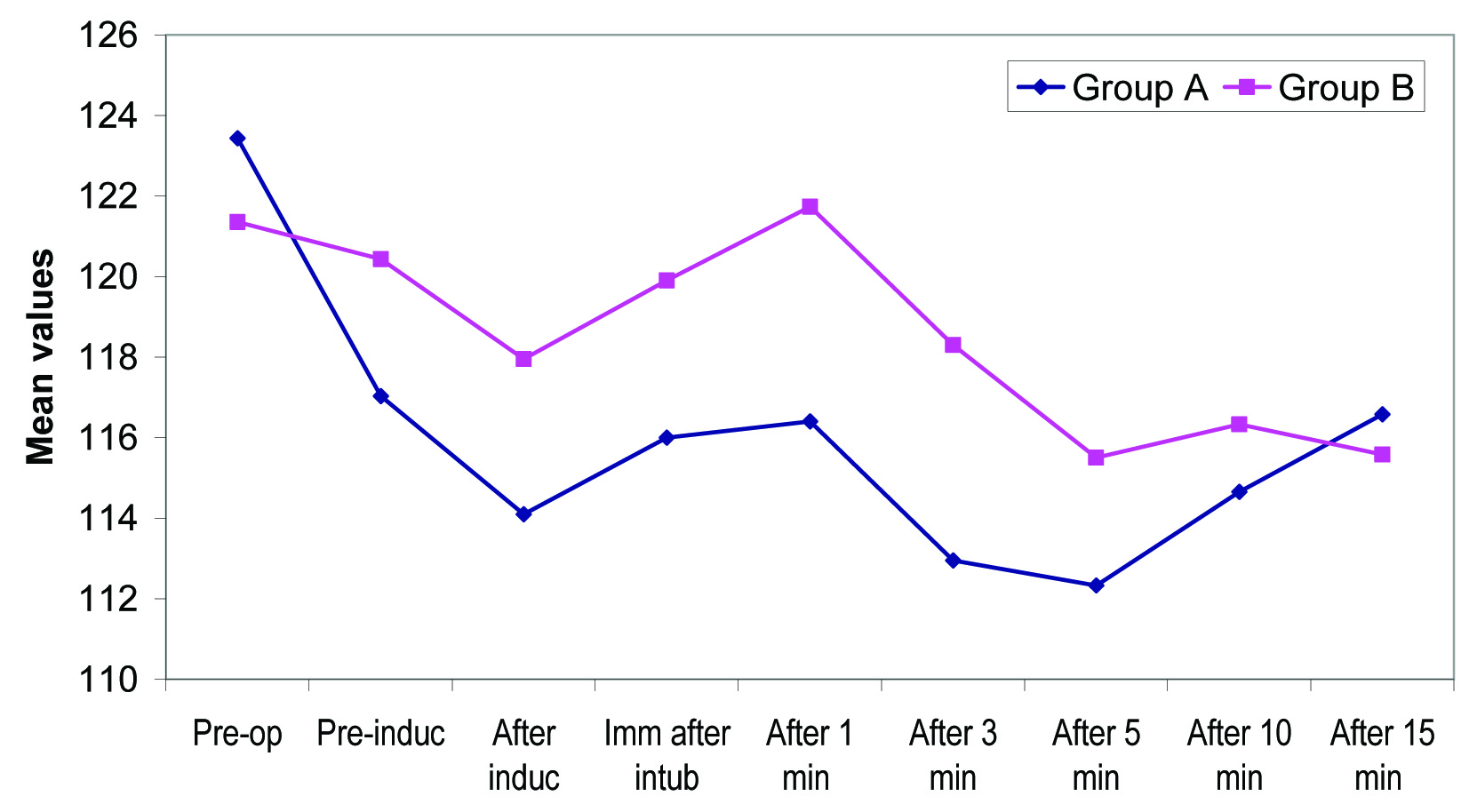
Pre-operative BP changes after premedication were statistically significant in groups. We found that after premedication systolic blood pressure was better controlled in Clonidine Group in comparision to Pregabalin Group throughout the study period which was statistically significant at 1 minute post-induction (p=0.032) and 3 minute post-induction (p=0.008) [Table/Fig-1].
Between group comparison of systolic blood pressure (mm Hg) at different time intervals.
| Time of observation | Group A (n=40) | Group B (n=40) | Statistical Significance |
|---|
| Mean | ±SD | Mean | ±SD | ‘t’ | ‘p’ |
|---|
| Preoperative | 123.43 | 9.95 | 121.35 | 5.79 | 1.140 | 0.258 |
| Pre-induction | 117.03 | 12.81 | 120.43 | 4.14 | 1.597 | 0.114 |
| After induction | 114.10 | 13.24 | 117.95 | 3.46 | 1.779 | 0.079 |
| Immediately after intubation | 116.00 | 15.54 | 119.90 | 4.00 | 1.537 | 0.128 |
| After 1 min | 116.40 | 14.94 | 121.73 | 3.97 | 2.178 | 0.032 |
| After 3 min | 112.95 | 11.72 | 118.30 | 4.36 | 2.706 | 0.008 |
| After 5 min | 112.33 | 13.89 | 115.50 | 4.52 | 1.375 | 0.173 |
| After 10 min | 114.65 | 13.66 | 116.33 | 4.35 | 0.739 | 0.462 |
| After 15 min | 116.58 | 13.35 | 115.58 | 3.59 | 0.458 | 0.648 |
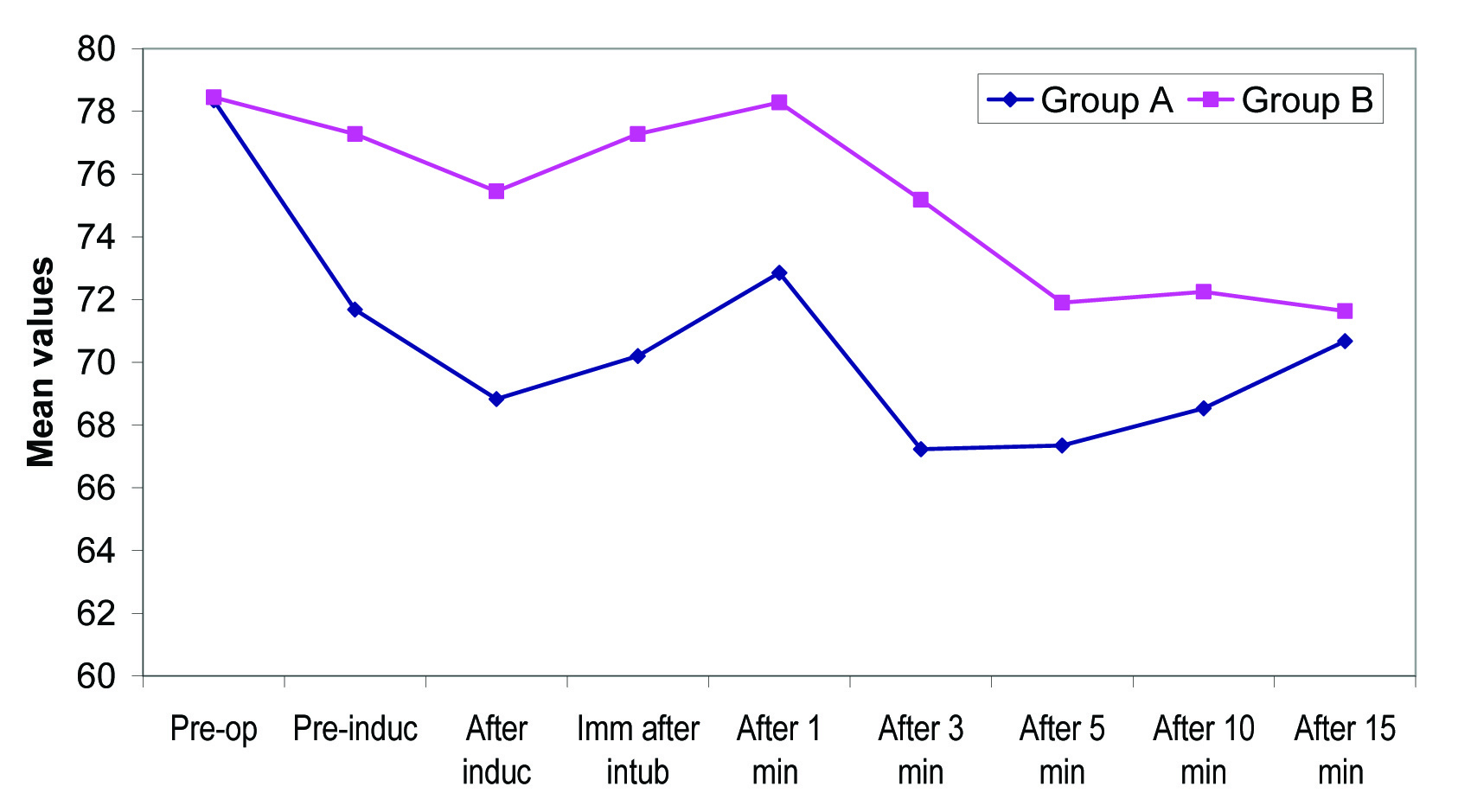
Diastolic blood pressure of Group A patients was lower than that of Group B patients at all the above periods of observation. This difference was found to be statistically significant at all the above periods of observation (p<0.05) except at baseline (preoperative), 10 minute postoperatively and 15 minutes postoperatively [Table/Fig-2].
Between group comparison of diastolic blood pressure (mm Hg) at different time intervals.
| Time of observation | Group A (n=40) | Group B (n=40) | Statistical Significance |
|---|
| Mean | ±SD | Mean | ±SD | ‘t’ | ‘p’ |
|---|
| Preoperative | 78.35 | 10.45 | 78.45 | 4.67 | 0.055 | 0.956 |
| Pre-induction | 71.68 | 11.36 | 77.28 | 3.33 | 2.993 | 0.004 |
| After induction | 68.83 | 11.47 | 75.45 | 3.18 | 3.521 | 0.001 |
| Immediately after intubation | 70.20 | 14.76 | 77.28 | 3.87 | 2.933 | 0.004 |
| After 1 min | 72.85 | 14.83 | 78.28 | 3.31 | 2.258 | 0.027 |
| After 3 min | 67.23 | 10.23 | 75.18 | 3.40 | 4.666 | <0.001 |
| After 5 min | 67.35 | 13.67 | 71.90 | 2.71 | 2.065 | 0.042 |
| After 10 min | 68.53 | 13.61 | 72.25 | 2.65 | 1.700 | 0.093 |
| After 15 min | 70.68 | 14.70 | 71.63 | 2.47 | 0.403 | 0.688 |
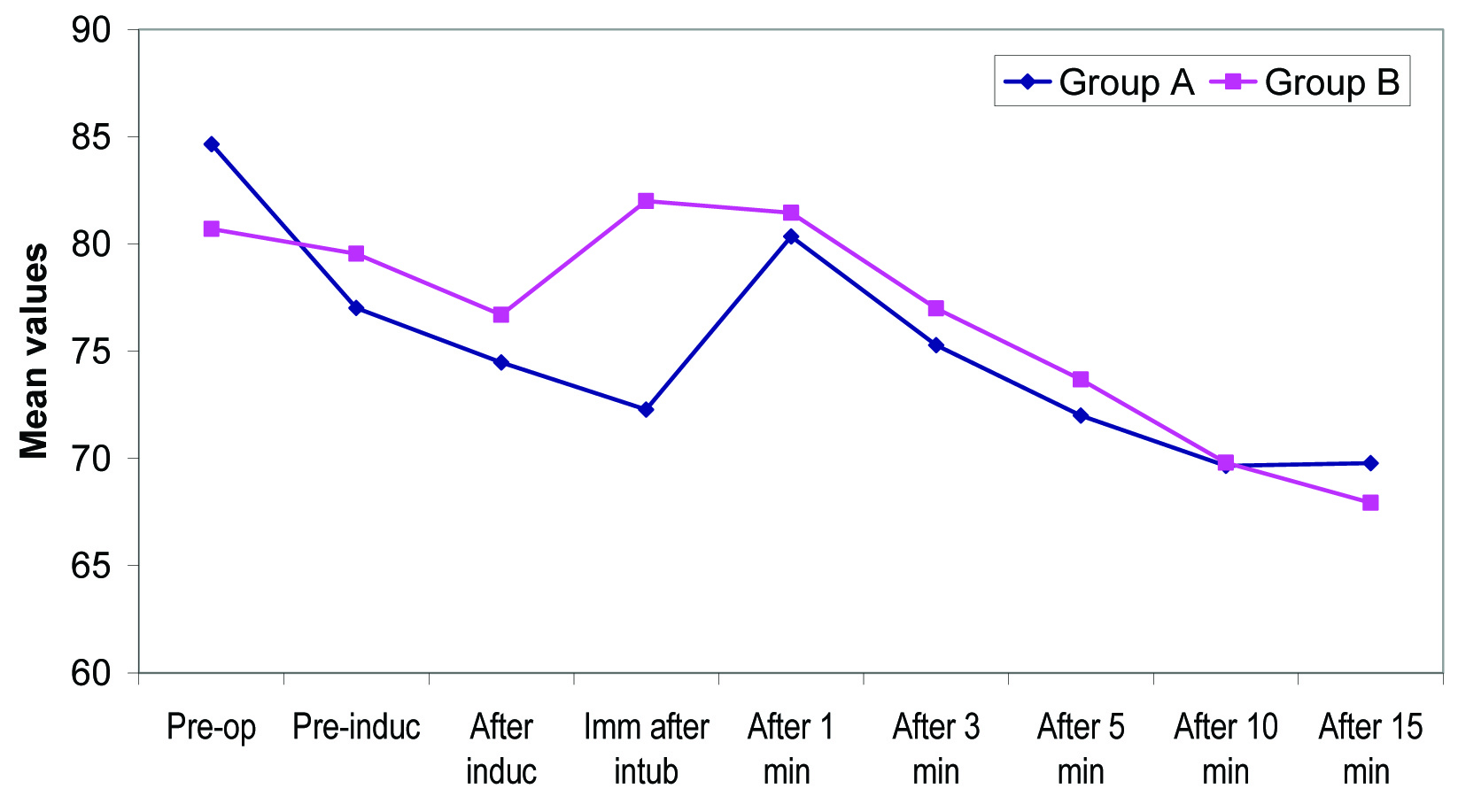
MAP of clonidine group was found to be lower than that of pregabalin group. This difference was found to be statistically significant at all the above periods of observation (p<0.05) except at 10 minute post-intubation (p=0.116; NS) and 15 minutes post-intubation (p=0.894; NS) [Table/Fig-3].
Between group comparison of mean arterial pressure (mm Hg) at different time intervals.
| Time | Group A (n=40) | Group B (n=40) | Statistical Significance |
|---|
| Mean | ±SD | Mean | ±SD | ‘t’ | ‘p’ |
|---|
| Preoperative | 93.00 | 9.78 | 92.75 | 4.81 | 0.145 | 0.885 |
| Pre-induction | 86.28 | 11.64 | 91.68 | 3.30 | 2.824 | 0.006 |
| After induction | 83.13 | 11.48 | 89.70 | 2.90 | 3.513 | 0.001 |
| Immediately after intubation | 85.45 | 14.45 | 91.55 | 3.46 | 2.597 | 0.011 |
| After 1 min | 86.73 | 14.58 | 92.78 | 3.17 | 2.564 | 0.012 |
| After 3 min | 81.75 | 10.18 | 89.60 | 3.22 | 4.650 | <0.001 |
| After 5 min | 81.90 | 13.43 | 86.38 | 2.74 | 2.065 | 0.042 |
| After 10 min | 83.38 | 13.79 | 86.90 | 2.61 | 1.589 | 0.116 |
| After 15 min | 86.00 | 13.97 | 86.30 | 2.50 | 0.134 | 0.894 |
At all the observation periods heart rate of clonidine group was found to be lower than that of pregabalin group and this difference was statistically significant only at time of intubation (p<0.001) and at rest observation periods this difference was not found to be statistically significant [Table/Fig-4].
Between group comparison of heart rate (per minute) at different time intervals.
| Time | Group A (n=40) | Group B (n=40) | Statistical Significance |
|---|
| Mean | SD | Mean | SD | ‘t’ | ‘p’ |
|---|
| Preoperative | 84.65 | 11.24 | 80.70 | 5.97 | 1.964 | 0.053 |
| Pre-induction | 77.02 | 15.80 | 79.55 | 5.43 | 0.956 | 0.342 |
| After induction | 74.48 | 16.72 | 76.70 | 5.64 | 0.797 | 0.428 |
| Immediately after intubation | 72.28 | 14.68 | 82.00 | 4.79 | 3.983 | <0.001 |
| After 1 min | 80.35 | 12.96 | 81.45 | 5.29 | 0.497 | 0.621 |
| After 3 min | 75.28 | 13.31 | 77.00 | 5.18 | 0.764 | 0.447 |
| After 5 min | 72.00 | 13.67 | 73.68 | 5.45 | 0.720 | 0.474 |
| After 10 min | 69.65 | 13.23 | 69.80 | 5.73 | 0.066 | 0.948 |
| After 15 min | 69.78 | 12.45 | 67.93 | 6.19 | 0.842 | 0.403 |
With respect to sedation scores in our study pre-operatively sedation score of clonidine group (1.73±0.45) was found to be lower as compared to that of pregabalin group (2.00±0.00) and difference in preoperative sedation score of the two groups was found to be statistically highly significant [Table/Fig-5].
Between group Comparison of Pre-operative and Post-operative sedation score.
| Time of observation | Group A (n=40) | Group B (n=40) | Statistical Significance(Mann-Whitney ‘U’ test) |
|---|
| Mean | ±SD | Mean | ±SD | ‘Z’ | ‘p’ |
|---|
| Preoperative | 1.73 | 0.45 | 2.00 | 0.00 | -3.549 | <0.001 |
| Postoperative | 2.20 | 0.41 | 2.73 | 0.55 | -4.306 | <0.001 |
Similarly, postoperative sedation score of clonidine group (2.20±0.41) was found to be lower than that of pregabalin group (2.73±0.55). Difference in postoperative sedation score of both the groups was found to be statistically significant [Table/Fig-5].
VAS scores of clonidine group at all the observational time periods were found to be higher than that of pregabalin group. It was also found that the difference in mean VAS score of both the groups was statistically significant upto time period 2-4 hours, thereafter (4-12 hours and 12-24 hours) difference was not found to be statistically significant. Change in VAS score was found to be statistically significant in both the groups at all the time intervals [Table/Fig-6].
Between group comparison of VAS score at different time intervals.
| Time | Group A (n=40) | Group B (n=40) | Statistical Significance(Mann-Whitney ‘U’ test) |
|---|
| Mean | ±SD | Mean | ±SD | ‘Z’ | ‘p’ |
|---|
| 5-15 min | 2.50 | 0.51 | 2.10 | 0.30 | 3.879 | <0.001 |
| 2 hours | 3.00 | 0.00 | 2.30 | 0.46 | 6.522 | <0.001 |
| 2-4 hours | 3.55 | 0.50 | 3.20 | 0.41 | 3.213 | 0.001 |
| 4-12 hours | 3.85 | 0.80 | 3.83 | 0.64 | 0.000 | 1.000 |
| 12-24 hours | 4.25 | 0.71 | 4.23 | 0.58 | 3.444 | 0.731 |
None of the patient from either of the groups required analgesia within 0-2 hours of surgery. Within 2-24 hours of surgery, requirement of analgesia was found in higher proportion of patients from clonidine group as compared to pregabalin group. This difference was not found to be statistically significant.
In Pregabalin Group higher proportion of patients (90.0%) did not face any side effect as compared to Clonidine Group (82.50%). Bradycardia was the most common side effect faced in both the groups, though proportion of patients facing bradycardia was higher for Clonidine Group (17.50%) as compared to that of Pregabalin Group (7.50%) but this difference was not found to be statistically significant. One (2.50%) patient of Pregabalin Group faced hypotension along with bradycardia.
The intragroup comparisons of the systolic and diastolic blood pressure, mean arterial pressure and heart rate are shown in [Table/Fig-7,8,9 and 10].
Intragroup change in systolic blood pressure (mm Hg) from baseline.
Intragroup change in diastolic blood pressure (mm Hg) from baseline.
Intragroup change in mean arterial pressure (mm Hg) from baseline.

Intragroup change in heart rate from baseline.
Discussion
This prospective randomized trial was conducted to compare the effects of oral clonidine (0.3mg) versus oral pregabalin (150mg) premedication on stress response to direct laryngoscopy and tracheal intubation in patients undergoing laparoscopic cholecystectomy.
Laryngoscopy and tracheal intubation are associated with haemodynamic stress responses due to sympathetic stimulation, which results in marked increase in heart rate, blood pressure, circulating catecholamines [1] and arrhythmias [27]. This can also lead to increased risk of myocardial ischemia during tracheal intubation [2]. These effects are transient but can be detrimental to the patients, especially in presence of coronary artery disease and cerebrovascular disease. Numerous studies have been done to find out ways to reduce or abolish the stress response. Many drugs like fentanyl [7], intranasal nitroglycerine [3], sublingual nifedipine [5], diltiazem [6], esmolol [4], alfentanyl [9,10], remifentanyl [10], lignocaine [28], dexmedetomidine [29,30] have been evaluated to reduce stress response with varying results.
The efficacy of clonidine in attenuating haemodynamic stress response has been studied previously in many studies and proved its effectiveness. Orally administered clonidine in preanaesthetic period provides haemodynamic stability and attenuates the stress response to laryngoscopy and tracheal intubation [14–23]. Mechanisms by which clonidine blunts the stress response of airway instrumentation are activation of central α2 adrenoreceptors which decreases peripheral sympathetic tone and stimulation of peripheral presynaptic α2 adrenoreceptors which leads to decreased norepinephrine release from nerve endings, hence reduced peripheral sympathetic tone.
Pregabalin is congener of gabapentine, an antiepileptic drug, acts by inhibiting membrane voltage-gated calcium channels in central nervous system. It does not interact with GABA receptors. It has analgesic, anticonvulsant, and anxiolytic properties. It is effective in controlling neuropathic pain. Effect of pregabalin on attenuating stress response to laryngoscopy and tracheal intubation was evaluated previously in few studies [24,25]. It was found to be very useful and effective premedicant to blunt haemodynamic stress response to tracheal intubation in all those studies.
Only few studies are available in literature regarding the comparison of efficacy of both these drugs in attenuating stress response to laryngoscopy and tracheal intubation. Gupta K et al., evalauted and compared these drugs and found that both the drugs provide haemodynamic stability during laryngoscopy without prolongation of recovery time and side effects [26]. The results of our study support the observations of Gupta K et al. According to them clonidine was found superior to pregabalin for attenuation of the haemodynamic stress responses to laryngoscopy and tracheal intubation but with increased incidence of intra-and postoperative bradycardia. No postoperative side effects were observed in premedicated patients.
Conclusion
We found that oral clonidine 0.3mg as well as oral pregabalin 150mg is effective in blunting haemodynamic stress response to laryngoscopy and tracheal intubation. Clonidine was found to be more effective than pregabalin in lowering of blood pressure and heart rate changes associated with laryngoscopy and tracheal intubation. Pregabalin gives better postoperative analgesia, more sedation and less bradycardia as compared to clonidine. To summarize, both the drugs are effective in attenuating stress response to laryngoscopy and tracheal intubation without much side effects and the added advantage of intra-operative and post-operative analgesia. Further studies are still needed to establish the efficacy and safety of these drugs in patients with co-morbid conditions and in patients of extreme age group.