Massive Pulmonary Embolism in a Patient Using Warfarin at Therapeutic Dose
Sunnetcioglu Aysel1, Esen Ramazan2, Arisoy Ahmet3
1 Assistant Professor, Department of Chest Diseases, Yuzuncu Yil University Medical Faculty, Van, Turkey.
2 Assistant Professor, Department of Hematology, Yuzuncu Yıl University Medical Faculty, Van, Turkey.
3 Assistant Professor, Department of Chest Diseases, Yuzuncu Yil University Medical Faculty, Van, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sunnetcioglu Aysel, Department of Chest Diseases, Yuzuncu Yil University School of Medicine, 65100, Van Turkey.
E-mail: izciaysel@mynet.com
Warfarin sodium is commonly used for the prevention and treatment of thromboembolism. The efficacy of warfarin therapy depends on maintaining the International Normalised Ratio (INR) within the target range for the indication. A 56-year-old male presented to the emergency department with dyspnea and chest pain, together with pain and swelling in both legs. The patient had been taking warfarin at the therapeutic dose since having undergone an aortic valve replacement four years ago. His vital signs were an arterial pressure of 60/30 heart rate of 138 beats per minute, respiratory rate of 30 per minute and oxygen saturation of 60%. Computed tomography of the chest revealed thrombosis of the right pulmonary artery and its segmental branches. On investigating the aetiology of the venous thromboembolism, the level of Antithrombin III (AT III) activity was found to be at 37% (normal range, 80–120%).
Antithrombin III, Thromboembolism, Vitamin K antagonists
Case Report
A 56-year-old male was admitted to the emergency department with one-week history of difficulty in breathing and chest pain, together with pain and swelling in both legs. The patient had been taking warfarin since having undergone an aortic valve replacement four years ago. He had a history of pulmonary embolism, seven years ago. He had no medical history of chemotherapy and/or hormone therapy and surgical interventions. He presented with an arterial pressure of 60/30 mmHg, a heart rate 138 beats/minute, respiratory rate of 30 breaths/minute, and oxygen saturation of 60%, temperature of 36.9°C. During physical examination, auscultation revealed decreased breath sounds bilaterally. Both lower extremities were edematous.
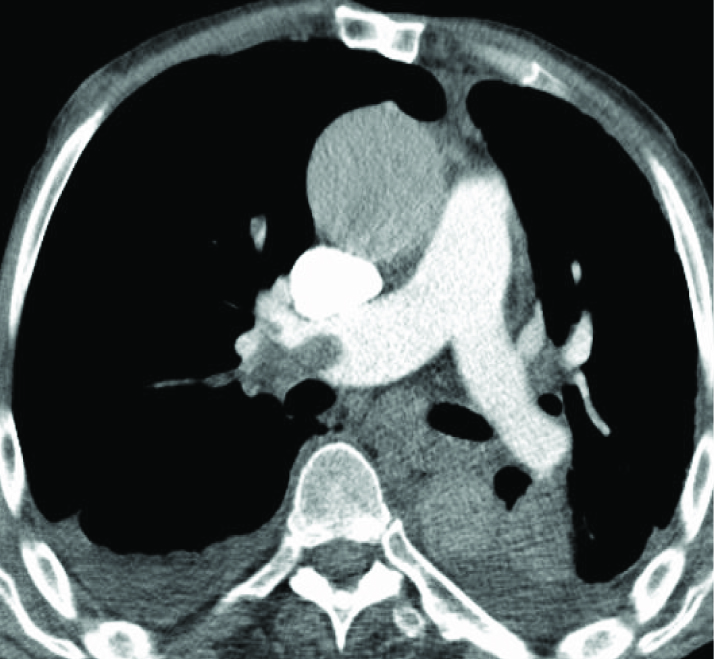
Initial laboratory values were as follows: haemoglobin (Hb), 11.9 g/dL; white blood cell count-8800/mL; platelet count-56.000/ mL; erythrocyte sedimentation rate, 10 mm/h; and C reactive protein, 30 mg/dL (normal range, 0-5); creatinin, 0.75 mg/dl; AST, 44 IU/L; ALT-17 IU/L; D-dimer, 20.2μg/mL; APTT-32 and INR, 2.59. Echocardiography revealed right heart dilatation, pulmonary hypertension, and paradoxical septal motion. Venous doppler ultrasound of the lower extremities showed total thrombosis of the vena saphena magna, superficial femoral vein, deep femoral vein, and popliteal vein, in both legs. Computed tomography of the chest revealed partial thrombosis of the right pulmonary artery and its segmental branches [Table/Fig-1]. The patient was diagnosed with massive pulmonary embolism and was admitted to the intensive care unit and warfarin was discontinued. Because of the thrombocytopenia, the patient was started on low-molecular-weight heparin. One day later, edema was observed in both upper extremities. Consequently, color doppler imaging of the venous system of the upper extremities was ordered. In the left and right cephalic veins, partial and total thrombosis was observed, respectively. On investigating the aetiology of the (VTE), it was found that activated protein C resistance and the antiphospholipid antibody titer were within normal limits, as were the concentrations of protein C, protein S, factor V Leiden, and prothrombin 20210 G–A. The level of AT III activity, as measured by chromogenic assay, was found to be at 37% (normal range, 80–120%). At one month after admission, AT III activity was at 38%. At five weeks after admission, the patient died due to respiratory failure.
Contrast-enhanced computed tomography scan showing massive pulmonary embolism; thrombus is are visible in the right main pulmonary artery.
Discussion
Warfarin sodium (Coumadin), one of a group of anticoagulants known as vitamin K antagonists, is used worldwide for a variety of purposes, including the prevention or treatment of Venous Thromboembolism (VTE), as well as of thromboembolic complications of cardiac valve replacement, atrial fibrillation, or myocardial infarction. Antithrombin III (AT III) is the major inhibitor of activated coagulation factors [1]. The primary target is thrombin, followed by the free factors X, IX, and VII. Deficiency of AT III is a significant risk factor for thromboembolic disease [2,3]. In cases of venous thrombosis, the goals of treatment are to decrease clot propagation, as well as to prevent the recurrence of thrombosis, to prevent the occurrence of pulmonary embolism, and to reduce the consequent potential for the development of pulmonary hypertension. Most patients requiring long-term anticoagulant therapy respond well to warfarin targeted to an INR of 2.0–3.0. However, in patients with cancer, on warfarin, report development of recurrent thrombosis even if the INR is maintained within the therapeutic range [4]. For patients with lupus anticoagulant activity or cardiolipin antibodies and requiring long-term anticoagulation, the optimal intensity of anticoagulation therapy is unknown. There are reports, based on retrospective analyses of observational studies, that thrombosis patients with antiphospholipid antibody syndrome are inadequately protected from recurrent episodes of VTE if the target of the treatment is an INR of 2.0–3.0 [5,6].
Approximately 30% of patients with deep venous thrombosis or pulmonary embolism have thrombophilia. Extensive evaluation is recommended in patients under 50 years of age with an idiopathic episode of deep venous thrombosis, as well as in those with recurrent thrombosis, a family history of thromboembolism, or thrombosis at an unusual site [7,8]. In this case, there was also thrombosis in both upper extremities.
Upper extremity deep vein thrombosis is a rare manifestation of venous thromboembolic disease. Some prothrombotic factors, such as factor V Leiden, prothrombin gene mutation (G20210A), hyperhomocysteinemia, AT III, protein C and protein S deficiency have also been stated as causative and/or predisposing factors [9]. In cases of thrombophilia, thrombosis is easily controlled by anticoagulant therapy, to progressive, intractable thrombosis, which is resistant to all forms of therapy.
Conclusion
Massive pulmonary embolism, a life-threatening manifestation of deep vein thrombosis, is a disorder that develops suddenly and can result in death if left undiagnosed. It is uncommon in patients using anticoagulant at the therapeutic dose. Hovewer, the present case shows that in patients with AT III deficiency receiving warfarin at the therapeutic dose can develop massive thromboembolism.
[1]. Kolde MJ, Haemostasis 2004 Basel: EdPentapharm Ltd:37-39. [Google Scholar]
[2]. Furie B, Pathogenesis of thrombosisJ.Biol.Chem 2009 267:255-63. [Google Scholar]
[3]. Zakai NA, Katz R, Jenny NS, Psaty BM, Reiner AP, Schwartz SM, Inflammation and haemostasis biomarkers and cardiovascular risk in the elderly: The cardiovascular health studyJ Thromb Haemost 2007 5:1128-35. [Google Scholar]
[4]. Prandoni P, Lensing AW, Piccioli A, Bernardi E, Simioni P, Girolami B, Recurrent venous thromboembolism and bleeding complications during anticoagulant treatment in patients with cancer and venous thrombosisBlood 2002 100(10):3484-88. [Google Scholar]
[5]. Khamashta MA, Cuadrado MJ, Mujic F, Taub NA, Hunt BJ, Hughes GRV, The management of thrombosis in the antiphospholipid-antibody syndromeN Engl J Med 1995 332:993-97. [Google Scholar]
[6]. Derksen RHWM, de Groot PG, Kater L, Nieuwenhuis HK, Patients with antiphospholipid antibodies and venous thrombosis should receive long term anticoagulant treatmentAnn Rheum Dis 1993 52:689-92. [Google Scholar]
[7]. Dykes AC, Walker ID, McMahon AD, Islam SI, Tait RC, A study of protein S antigen levels in 3788 healthy volunteers: influence of age, sex and hormone use, and estimate for prevalence of deficiency stateBr J Haematol 2001 113(3):636-41. [Google Scholar]
[8]. Khan S, Dickerman JD, Hereditary thrombophiliaThromb J 2006 4:15 [Google Scholar]
[9]. Joffe HV, Goldhaber SZ, Upper-extremity deep vein thrombosisCirculation 2002 106:1874-80. [Google Scholar]