An Unusual Case of Facial Hyperpigmentation Solved on Histopathology
Kiran Agarwal1, Vandana Puri2, Ruchika Kumar Goel3, Deepti Verma4
1 Director Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
2 Assistant Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
3 Senior Resident, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
4 Senior Resident, Department of Pathology, Lady Hardinge Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vandana Puri, Assistant Professor, Department of Pathology, Lady Hardinge Medical College, New Delhi-110001, India.
E-mail: drvandanapuri@gmail.com
Dear Editor,
Ochronosis is an uncommon condition and refers to accumulation of brownish yellow pigment in the connective tissue with a prevalence of 1/250,000–1,000,000 individuals [1].
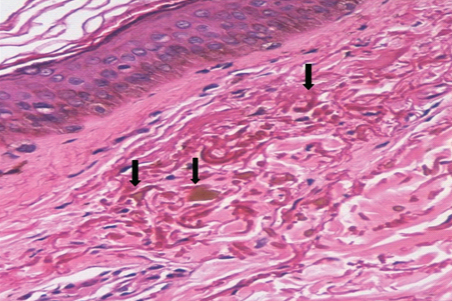
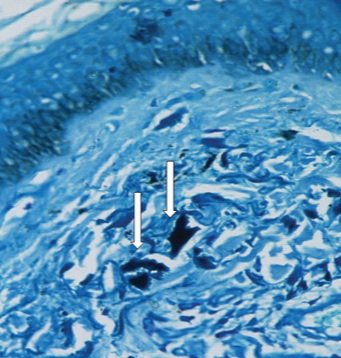
It can occur in two forms: exogenous and endogenous [2]. Endogenous ochronosis (alkaptonuria) is an autosomal recessive disease caused by absence of homogentisic acid oxidase. Exogenous ochronosis occurs due to hydroquinone therapy given for melasma. It can also develop secondary to phenol, resorcinol, mercury, picric acid and antimalarials [3]. A 31-year-old male presented with complaints of facial hyperpigmentation since 5 years. On physical examination, patient had bilateral slate grey to brownish pigmentation on the malar and periorbital area [Table/Fig-1]. Few discrete pinhead sized papules were present below the lower eyelids. There was no epidermal atrophy. A clinical diagnosis of melasma or photosensitivity was considered. Topical application of 2% hydroquinone cream was advised in view of most probable diagnosis of melasma but hyperpigmentation gradually worsened. Since patient did not show any improvement, a skin biopsy was done and sent for histopathological examination. Histopathologic sections revealed presence of “yellowish brown” pigment present within homogenized and swollen collagen bundles in the upper dermis [Table/Fig-2]. At places the collagen bundles were broken with ragged edges and formed irregular “banana- shaped” clumps. Mild pigment incontinence was observed in the upper dermis. The pigment stained blue black with methylene blue [Table/Fig-3]. There was no increase in pigment either in basal layer or other layers of epidermis. Based on the above findings a diagnosis of ochronosis was considered. No history of arthritis, renal disease, and hyperpigmentation of sclera, genitals, joints and axilla could be elicited from the patient. There was also no darkening of urine when left to stand. Hence, endogenous ochronosis was ruled out and a final diagnosis of exogenous ochronosis was given.
Subject showing brownish pigmentation on the malar and periorbital area.

Photomicrograph showing presence of “yellowish brown” pigment present within homogenized and swollen collagen bundles in the upper dermis (H&E x400).
The pigment stained blue black with methylene blue (H#x0026;Ex400).
Exogenous ochronosis commonly present as blue black macules on the malar areas, temples, inferior cheeks and neck. Three clinical stages of exogenous ochronosis have been described: (i) erythema and mild pigmentation; (ii) hyperpigmentation, black colloid milia and scanty atrophy; and (iii) papulonodules with or without surrounding inflammation [4]. The cause of exogenous ochronosis is still debatable. One theory proposed that topical hydroquinone inhibits homogentisic acid oxidase resulting in local accumulation of homogentisic acid that then polymerizes to form ochronotic pigment. Another hypothesis states that there is increased tyrosinase activity by hydroquinone [5].
Melasma mimics exogenous ochronosis, clinically thus clinically it is essential to have a biopsy proven diagnosis of melasma before beginning of treatment [6]. On microscopy it shows presence of increased pigment in all the layers of epidermis and abundant melanophages in dermis but no ochre colored pigment [2].
A wide number of treatment options are available for exogenous ochronosis but with variable efficacy. These include retinoic acid, sunscreen, cryotherapy, dermabrasion, CO2 laser and Q switched ruby laser [5]. The patient was put on retinoic acid and sunscreen lotion; however, there was only slight fading of the pigmentation.
This case was presented because of its rarity and to make dermatologists aware of importance of biopsy to differentiate hyperpigmentation of ochronosis from melasma. This case also emphasizes the judicious use of hydroquinone in treatment of melasma. An early diagnosis necessitates immediate discontinuation of hydroquinone, rather than increasing the concentration in an attempt to clear the dermatosis [7].
[1]. Keller JM, Macaulay W, Nercessian OA, Jaffe IA, New developments in ochronosis: review of the literatureRheumatol Int 2005 25:81-85. [Google Scholar]
[2]. Maize JC, Maize JC, Metcalf J, Metabolic diseases of skin. In David E Elder, Elenitsas R, Murphy GF, Xu XLever’s Histopathology of skin 2009 10th EdnLippincott Williams and Wilkins:425-458. [Google Scholar]
[3]. Merola JF, Meehan S, Walters RF, Brown L, Exogenous ochronosisDermatology Online Journal 2008 14:6 [Google Scholar]
[4]. Ladizinski B, Mistry N, Kundu RV, Widespread use of toxic skin lightening compounds: medical and psychosocial aspectsDermatol Clin 2011 29:111-23. [Google Scholar]
[5]. Touart DM, Sau P, Cutaneous deposition diseases. Part IIJ Am Acad Dermatol 1998 39:527-44. [Google Scholar]
[6]. Vallonthaiel AG, Kakkar A, Singh MK, Raman M, Ochronosis with subtle histological findingsIndian J Dermatol Venereol Leprol 2015 81:623-24. [Google Scholar]
[7]. Jain A, Pai SB, Shenoi SD, Exogenous ochronosisIndian J Dermatol Venereol Leprol 2013 79:522-23. [Google Scholar]