Intra Luminal Metastasis to Duodenum: A Histological Surprise
Kaushik Subramanian1, Tirou Aroul2, Sasikumar Kuppusamy3, Vijay Gunashekaran4
1 Surgical Consultant, Department of General Surgery, MGMC & RI, Pondicherry, India.
2 Professor and Head, Department of General Surgery, MGMC & RI, Pondicherry, India.
3 Surgical Consultant, Department of General Surgery, MGMC & RI, Pondicherry, India.
4 Junior Resident, Department of General Surgery, MGMC & RI, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kaushik Subramanian, C 123, Bhadra Nilaya, Amaravati Housing Colony, Harihar, Karnataka-577601, India.
E-mail: kaushik1886@gmail.com
Carcinoma cervix is one of the most common malignancies seen in women worldwide and more so in the Indian subcontinent. Carcinoma cervix is known for its orderly lymphatic spread. Skip metastasis or intraluminal metastasis is not a frequent occurrence. A 50-year-old diabetic and hypertensive female patient who was diagnosed to have carcinoma cervix (stage II A 2) Grade II to III and post radiotherapy (3 years back) presented to the surgical outpatient with dyspeptic symptoms and vague abdominal pain. On examination she was found to have a 1x1cm hard, fixed, left supraclavicular node and a palpable liver. Ultrasound abdomen revealed multiple retro peritoneal lymphadenopathy and Contrast Enhanced Computerised Tomography (CECT) abdomen revealed secondary deposits in the pancreatico-duodenal groove infiltrating the duodenal C-loop and pancreatic head, with multiple retroperitoneal nodes with necrosis. Fine needle Aspiration Cytology (FNAC) from left supraclavicular node revealed metastatic squamous cell carcinoma. Oesophagogastroduodenoscopy showed 2 sessile lesions in the anterior wall of duodenum with mucosa stretched and central umbilication with almost complete luminal obstruction. Biopsy from the duodenal lesion also turned out positive for metastatic squamous cell carcinoma. Gynaecological examination was negative for any local recurrence. Patient was managed symptomatically for dyspepsia and is currently undergoing chemotherapy. She is at present on regular follow-up and is asymptomatic for the bowel metastasis. Given the frequency of cancer cervix and the rarity of intra luminal metastasis, this case report serves to reiterate the fact that the abdomen is truly a pandora’s box.
Carcinoma, Cervix, Duodenal polyp, Intra abdominal metastasis, Squamous cell cancer
Case Report
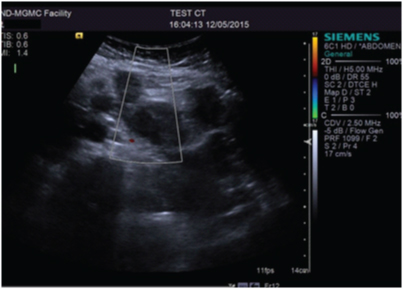
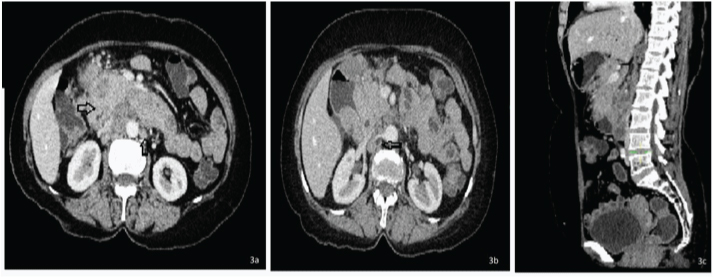
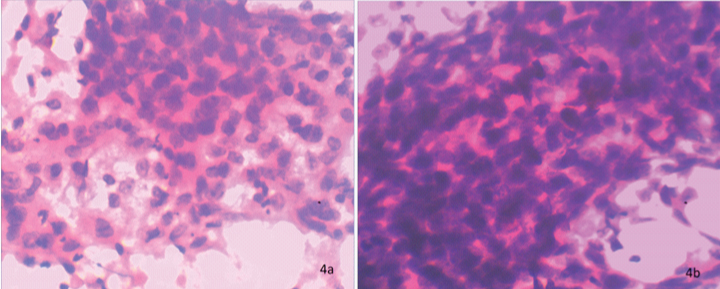
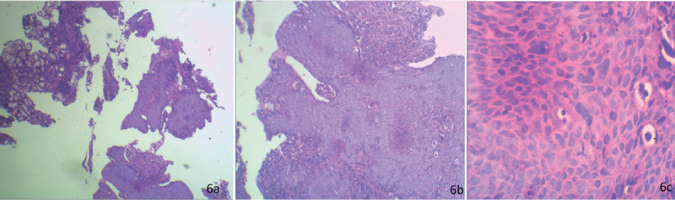
A 50-year-old postmenopausal lady, presented to the surgical outpatient department with vague upper abdomen pain, early satiety, increased frequency of belching, loss of appetite and weight of 1 month duration. She was on regular anti-hypertensives and oral hypoglycemic agents for her co-morbidities since the past 5 years. She was diagnosed as a case of squamous cell carcinoma cervix 2 years back (stage II A 2) (grade II-III) and was treated with 45Gray RT at a Regional Cancer Centre. She had successfully completed her radiotherapy course and was asymptomatic for her previous malignancy. The patient was well preserved and all her vital parameters were within normal limits. Signs of pallor were observed and a left supraclavicular node was noted on general physical examination. The node measured about 1x1 cm, was non tender, hard in consistency and was not mobile. No other cervical nodes were palpable on examination of the neck. Her ENT exam was unremarkable. Per abdomen examination revealed nontender hepatomegaly, 5cm below costal margin, hard in consistency. Examination did not reveal any free fluid. Per rectal examination also turned out to be normal. The rest of the abdomen and other systems were unremarkable. Her routine haematological and biochemical parameters were within normal limits except for the haemoglobin of 6.9 gm%. Chest X ray was normal [Table/Fig-1]. Ultrasound abdomen revealed multiple retro peritoneal lymphadenopathy [Table/Fig-2] and Contrast Enhanced Computerised Tomography (CECT) of the abdomen revealed secondary deposits in the pancreatico-duodenal groove infiltrating the duodenal C-loop and pancreatic head, with multiple retroperitoneal nodes with necrosis and multiple enhancing nodules of 10x5mm size in the posterior vaginal vault [Table/Fig-3a-c]. Fine needle Aspiration Cytology (FNAC) from left supraclavicular node revealed large clusters and sheets of pleomorphic, oval to spindle shaped cells with eosinophilic cytoplasm, vesicular nuclei, prominent nucleoli on necrotic background admixed with lymphocytes suggestive of metastatic squamous cell carcinoma [Table/Fig-4a&b]. Two sessile lesions in the anterior wall of duodenum with mucosa stretched and central umbilication with almost complete luminal obstruction were seen on oesophagogastroduodenoscopy [Table/Fig-5]. Biopsy from the duodenal lesion showed strips of pleomorphic squamous cells infiltrating into surrounding stroma, lymphoplasmacytic infiltration of lamina propria with absence of gland pattern, supporting the diagnosis of metastatic squamous cell carcinoma [Table/Fig-6a-c]. Gynaecological examination was negative for any local recurrence.
Chest X ray- The radiograph of the chest did not reveal any perihilar opacities. Bilateral lung fields were normal.

USG abdomen-Ultrasonography of the abdomen showed multiple hypoechoic lesions, largest measuring 1X1.2cms, in the retroperitoneum suggestive of enlarged lymph nodes, probably malignant aetiology.
Contrast enhanced Computerised tomography. 3a - CECT of the abdomen revealed secondary deposits in the pancreatico-duodenal groove infiltrating the duodenal C-loop and pancreatic head, with multiple retroperitoneal nodes with necrosis. 3b-CECTdemonstrates multiple pre and para aortic lymphadenopathy. 3c - Sagittal section shows multiple enhancing nodules of 10x5mm size in the posterior vaginal vault.
FNAC from left supraclavicular node- Photomicrograph of haematoxylin and eosin stained slide of Fine Needle Aspiration Cytology from left supraclavicular node revealed large clusters and sheets of pleomorphic, oval to spindle shaped cells with eosinophilic cytoplasm, vesicular nuclei, prominent nucleoli on necrotic background admixed with lymphocytes suggestive of metastatic squamous cell carcinoma. (10x and 40x respectively)
Esophagogastroduodenoscopy –Two sessile growths seen in anterior wall of duodenum with mucosa stretched and central umbilication with almost complete luminal obstruction.

Histopathology of the duodenal biopsy. 6a- Photomicrograph of haematoxylin and eosin stained slide of duodenal biopsy from the lesion under scanner view. (lens objective X4). 6b- Photomicrograph of haematoxylin and eosin stained slide of duodenal biopsy from the lesion under low power (lens objective X10) shows strips of pleomorphic squamous cells infiltrating into surrounding stroma, lymphoplasmacytic infiltration of lamina propria with absence of gland pattern, supporting the diagnosis of metastatic squamous cell carcinoma. 6c- Photomicrograph of haematoxylin and eosin stained slide of duodenal biopsy from the lesion under high power (lens objective X40) shows hyperchromatic, pleomorphic, squamous cells.
With this in mind we made a diagnosis of metastatic squamous cell carcinoma with probable primary being carcinoma cervix. Patient was managed symptomatically for dyspepsia and is currently undergoing chemotherapy. She is at present on, a regular follow-up and is asymptomatic for the bowel metastasis.
Discussion
Carcinoma cervix is the 2nd most common malignancy in females worldwide [1,2]. Its incidence in India is 19 to 44 per 1,00,000 women [3] and India accounts for nearly 1/3rd of global cervical cancer deaths [4]. Histologically, about 60-80% of them are squamous cell carcinoma, 5-15% is adenocarcinoma and adenosquamous carcinoma constitutes the minority [5].
Neoplasms of small bowel account for only 0.42% of total neoplasms and 2.3% of neoplasms of gastrointestinal tract [6]. Primary neoplasms of the small bowel are very rare, although ~75% of the entire length of the GI tract and 90% of the absorptive surface is contributed by small bowel.
Carcinoma of the cervix is one of the commonest malignancies seen in Indian subcontinent accounting for approximately 74,000 deaths per year [4]. It is one of most frequent malignancies seen in Indian women. Traditional teaching has been, that cancer cervix is a cancer of the fourth and fifth decade but the world is seeing a rapid earlier shift of cancer occurrence possibly due to an earlier age of sexual activity as also could be due to better and earlier detection methods available with us today [7].
Though being the largest endocrine organ of the body and the predominant content of the abdominal cavity the proportion of small bowel affliction with cancer is relatively small [8,9]. Based on the histology, WHO has broadly classified small bowel neoplasms into Epithelial tumours, Non-epithelial tumours, Malignant lymphomas, Secondary tumours, Polyps. Metastasis from a GIT source being the most common followed by primary malignancies such as carcinoids and adenocarcinoma. Duodenum is the most commonly affected and the incidence progressively reducing as we go towards the ileum [9,10].
Metastasis to the small bowel are usually from melanoma, breast, lung, colon and kidney cancers. Intestinal metastasis are usually a terminal event with concomitant hematogenous metastasis and are a poor prognostic marker with the exception of melanoma and renal cell carcinoma secondaries in which a reasonable DFS can be expected post adequate resection. The exact incidence of small bowel metastasis is hard to find given the rarity of its occurrence. The problem with metastasis to the small bowel is further compounded by the fact that most are asymptomatic until late into the disease since the small bowel is capable of distention and hence luminal obstruction is delayed. To add to this the post-radiotherapy status can cause chronic radiation enteritis and even present with bleeding which is more often a diagnosis than metastatic disease.
Carcinoma of the cervix is traditionally known to spread in an orderly pattern with lymphatic being the most common mode [11]. After local spread it is known to involve pre and para aortic nodes before metastasizing hematogenously [12]. Trans peritoneal and hematogenous spread being less commonly seen as most patients succumb to local metastasis before distant [13]. It is thus exceedingly rare for a patient to present with symptoms related to small bowel metastasis which is seen to be involved in only about 8% cases [14].
About 10 cases of metastasis to pyloro duodenum and small bowel have been reported in the past with some synchronous presentation and other metachronous with time interval being 2-13 years [13,15]. Search of the literature showed that the previous cases reported so far presented with obstruction, upper GI bleeding, peritonitis and pain abdomen. The presentation with non specific abdominal dyspeptic symptoms makes it even harder to diagnose as in our index case. Inspite of completing the course of Radiotherapy our patient presented with metastatic disease which shows the aggressive nature of such a commonly occurring malignancy.
It therefore puts the onus on us as clinicians and research methodologists to find markers that portend early dissemination so that better care can be delivered to the patient since once the patient develops widely disseminated disease our therapeutic options narrow down to symptomatic and palliative care rather than therapeutic.
Conclusion
Metastatic intra luminal pathologies though a rarity in themselves, given the high prevalence of cancer of the cervix in the subcontinent, the treating surgeon should be on the lookout for such rare presentation of a common problem.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
[1]. Ferlay J, Bray F, Pisani P and Parkin DM: GLOBOCAN 2002: Cancer incidence, mortality and prevalence worldwide. IARC Cancer Base No. 5, version 2.0. IARC Press, Lyon, France, 2004 [Google Scholar]
[2]. Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM, Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008Int J Cancer 2010 127:2893-917. [Google Scholar]
[3]. National cancer registry program (NCRP)Biennial report 1988–89. An epidemiological studyIndian Council of Medical Research New Delhi 1992 [Google Scholar]
[4]. WHO/ICO Information Centre on HPV and Cervical Cancer (HPV Information Centre). Summary report on HPV and cervical cancer statistics in India 2007. [Last Assessed on 2008 May 1]. Available from: http://www.who.int/hpvcentre [Google Scholar]
[5]. Cheah PL, Looi LM, Carcinoma of the uterine cervix: a review of its pathology and commentary on the problem in MalaysiansMalays J Pathol 1999 21(1):1-15. [Google Scholar]
[6]. Jemal A, Siegel R, Ward E, Hao Y, Xu J, Thun MJ, Cancer statistics, 2009CA Cancer J Clin 2009 59:225-49. [Google Scholar]
[7]. Waggoner SE, Cervical cancerThe Lancet 2003 361:2217-25. [Google Scholar]
[8]. Schottenfeld D, Beebe-Dimmer JL, Vigneau FD, The epidemiology and pathogenesis of neoplasia in the small intestineAEP 2009 19(1):58-69. [Google Scholar]
[9]. Torres M, Matta E, Chinea B, Dueno MI, Martinez-Souss J, Ojeda A, Malignant Tumors of the Small IntestineJ Clin Gastroenterol 2003 37(5):372-80. [Google Scholar]
[10]. Loualidi A, Spooren PFMJ, Grubben MJAL, Blomjous CEM, Goey SH, Duodenal metastasis: an uncommon cause of occult small intestinal bleedingThe Netherlands Journal of Medicine 2004 62(6):201-05. [Google Scholar]
[11]. Christopherson W, Voet R, Buchsbaum HJ, Recurrent cervical cancer presenting as small bowel obstructionGynecologic Oncology 1985 22:109-14. [Google Scholar]
[12]. Raphael JC, Ram TS, Pavamani S, Choudharie L, Viswanathan PN, Squamous cell carcinoma cervix with metastasis to pyloroduodenal regionJ Can Res Ther 2011 7:183-84. [Google Scholar]
[13]. Kanthan R, Senger JL, Diudea D, Kanthan S, A review of duodenal metastase from squamous cell carcinoma of the cervix presenting as an upper gastrointestinal bleedWorld Journal of Surgical Oncology 2011 9:113 [Google Scholar]
[14]. Gurian L, Ireland K, Petty W, Katon R, Carcinoma of the cervix involving the duodenum: case report and review of the literatureJ Clin Gastroenterol 1981 3:291-94. [Google Scholar]
[15]. Chawhan SM, Dani AA, Meshram SA, Randale AA, Kumbhalkar DT, Metastasis of squamous cell carcinoma of uterine cervix to duodenum: a case reportJournal of Clinical and Diagnostic Research 2015 9(1):ED3-4. [Google Scholar]