The International Association for the Study of Pain defines pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.” This definition recognizes the interplay between the objective, physiological sensory aspects of pain and its subjective, emotional and psychological components [1].
Postoperative pain after orthopaedic lower limb surgery is a very distressing symptom and a major component of the postoperative morbidity. So far, many analgesics by different routes have been used for postoperative pain relief which includes NSAIDs, acetaminophen, opioids but postoperative nausea, vomiting and bleeding becomes a concern with all these agents [2].
Regional anaesthesia which include epidural analgesia, single-shot and continuous peripheral nerve block and local anaesthetic wound infusion may provide reduction in the stress response, systemic analgesic requirements, opioid-related side effects and possibly the development of chronic pain [2]. Lower extremity blocks are safe and have certain advantages, such as postoperative pain relief and lack of complete sympathectomy. Recent applications have focused on postoperative analgesia rather than intraoperative anaesthesia to improve patient comfort and to assist in rehabilitation and early discharge from the hospital [3].
Bupivacaine is most commonly used local anaesthetic in regional anaesthesia. It belongs to aminoamide group of local anaesthetics [4]. Sciatic nerve block provides postoperative pain relief after below knee surgery and knee surgery [5]. Many studies with different approaches for sciatic nerve block have been conducted to demonstrate the efficacy of sciatic nerve block with different local anaesthetic drugs over the past decade [5–11].
To study the efficacy of single-shot sciatic nerve block for postoperative pain management in below knee orthopaedic surgery.
Materials and Methods
All patients aged between 18 and 60 years of either sex (male or female) scheduled for unilateral below knee open orthopaedic surgery in Poona Hospital & Research Centre, Pune between 1st November 2014 and 30th November 2015 under spinal anaesthesia were included in the study. Permission was obtained from Institutional Ethics Committee (IEC) and Scientific advisory committee of the institution and every patient signed an informed consent form. It was an observational study and was carried out on 60 American Society of Anaesthesiologists (ASA) grade I and II patients as per inclusion and exclusion criteria detailed below.
Inclusion Criteria
a) ASA physical status class I and II.
b) Age between 18-60 years of either sex.
c) Unilateral below knee open orthopaedic surgery.
Exclusion Criteria
a) Absence or withdrawal of valid written informed consent.
b) Bilateral below knee surgeries.
c) ASA physical status class III and IV.
d) Emergency surgeries.
e) Known hypersensitivity to any of the drug in the study.
f) Contraindications to nerve block like bleeding diathesis, infection at the site of needle placement, nearby cellulitis or systemic blood infections, individuals with delayed developmental milestones as well as patients with dementia or movement disorders and peripheral neuropathy or previous nerve injury.
Based on previously published study [12], setting an alpha error at 0.05, and power at 80%, sample size of 60 was calculated by formula [13].
Pre-anaesthetic check-up was conducted one day prior to surgery. The patients were evaluated for any systemic disease and routine laboratory investigations were recorded. The procedure of subarachnoid block and also the sciatic nerve block was explained to the patients and written informed consent obtained. The patients were educated about the Visual Analogue Scale (VAS). They were kept fasting for 6 hours for solid foods and 2 hours for clear liquids.
Patients were shifted to OT table after accessing IV line. All of them were preloaded with 15 ml/kg Ringers lactate, 15 minutes prior to the surgery. Baseline vitals were recorded using pulse oximetry, noninvasive BP and electrocardiography. Premedication: Inj. Ondansetron-4mg IV., Inj. Glycopyrrolate-0.2mg IV was given. Regional anaesthesia was administered.
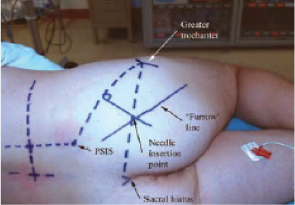
Sciatic nerve block was given by classic (posterior) approach of Labat [3]. The patient was positioned laterally, with the leg to be blocked rolled forward onto the flexed knee as the heel rests on the knee of the dependent non-operative leg (modified Sims position). A line was drawn to connect the Posterior superior iliac spine to the greater trochanter of the femur. A perpendicular line was drawn bisecting the first line and extending 5 cm caudal. A second line was drawn from the greater trochanter to the sacral hiatus. The intersection of this line with the perpendicular line indicated the point of needle entry and falls 5-8 cm along the line [Table/Fig-1]. We confirmed the location of sciatic nerve with the help of ultrasound.
Schematic of sciatic nerve block.
After skin disinfection, local anaesthetic was infiltrated subcutaneously at the needle insertion site. The operator assumed an ergonomic position to allow precise needle manoeuvring and monitoring of the responses to nerve stimulation. The nerve stimulator was set to deliver a current intensity of 1.5 mA. A 22 gauge, 10 to 12 cm atraumatic, insulated needle was introduced perpendicular to the spherical skin plane and advanced until a motor response was elicited (plantar flexion of the foot and toes). After an initial stimulation of the sciatic nerve was obtained, the stimulating current gradually decreased until twitches were still seen or felt at 0.2 to 0.5 mA. When the needle placed properly 20 ml of 0.5% Bupivacaine was injected after negative aspiration of blood. If any resistance to the injection of local anaesthetic was felt then the injection was stopped and needle was withdrawn by 1 mm before reattempting to inject under strict aseptic precautions, using 25 gauge Quincke’s spinal needle, lumbar puncture was performed at L3-4 space. Spinal anaesthesia was given using 3 ml of 0.5% hyperbaric Bupivacaine.
Intraoperatively heart rate, non-invasive BP, respiratory rate, ECG and SpO2 were monitored every 2 minutes for the first 10 minutes and every 10 minutes for the next 50 minutes and every 15 minutes till the end of surgery. Time to reach peak level of sensory block was noted using pin prick method.
Pain was assessed using “VAS” between 0 and 10 (0=no pain, 10= worst pain) at 0, 2, 4, 6, 8, 10, 12, 14, 16, 18, 20, 22 and 24 hours postoperatively. Diclofenac sodium 75 mg i.v. was given slowly intravenously as rescue analgesia when VAS was > 3. Time of supplemental analgesia was noted.
Adverse events such as nausea, vomiting, pruritis, hypotension, bradycardia, respiratory depression, sedation and prolonged sensory and motor blockade were looked for.
The quantitative data are presented as Mean and Standard Deviation (SD). The qualitative data are shown as percentages.
Results
Between 1st November 2014 and 30th November 2015, 60 patients were recruited in the study. In the present study, the age group of the patients was between 18 and 60 years. The mean age of the patients was 36.8 with standard deviation 6.9 years (Minimum age 23 years and Maximum 52 years). Out of 60 patients, 11 (18.3%) were between age of 20 and 29 years, 28 (46.7%) were between age of age 30 and 39 years, whereas 21 (35.0%) were between 40 and 52 years. Out of 60 patients, 31 (51.7%) were males and 29 (48.3%) were females.
The mean weight of the patients was 61.5 kg with standard deviation 6.3 Kg (Minimum weight 50 Kg, and Maximum weight 74 Kg). Out of 60 patients, 27 (45.0%) had weight between 50 and 59 kg, 27 (45.0%) had weight between 60 and 69 kg and 6 (10.0%) had weight more than 70 kg. Out of 60 patients, 41 (68.3%) had ASA grade I and 19 (31.7%) had ASA grade II.
Mean duration of surgery was 121.66 minutes whereas mean duration of spinal block was 198.33 minutes.
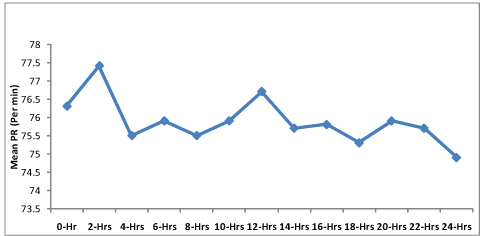
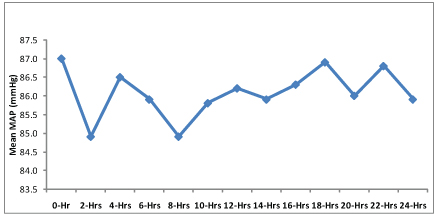
It can be seen from [Table/Fig-2,3] that mean pulse rate and mean arterial blood pressure were within normal limits.
Mean pulse rate at various time interval.
Arterial pressure at various time intervals.
As depicted in [Table/Fig-4], 16 (26.7%) patients did not require any rescue analgesia, whereas 40 (66.7%) patients required rescue analgesia after 18 hours of surgery; so in all 93.4% patients did not require rescue analgesia upto 18 hours after surgery. Mean VAS score of the patients who did not require rescue analgesia was 2.06 at 24 hours postoperatively which is far below the level where rescue analgesia was required [Table/Fig-5].
Time at which rescue analgesia given (n=60).
| Time rescueanalgesiagiven (Hrs) | No. of cases | Mean VAS | % of cases |
|---|
| Not given (at 24-Hrs) | 16 | 2.06 | 26.7 |
| 4-Hrs | 1 | 4.00 | 1.7 |
| 16-Hrs | 3 | 4.33 | 5.0 |
| 18-Hrs | 13 | 4.31 | 21.7 |
| 20-Hrs | 18 | 4.28 | 30.0 |
| 22-Hrs | 7 | 4.29 | 11.7 |
| 24-Hrs | 2 | 4.00 | 3.3 |
| Total | 60 | | 100.0 |
Mean Visual Analogue Score at different time interval.
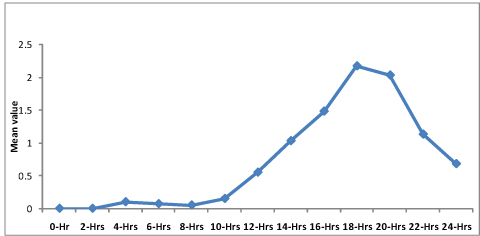
The mean time by which rescue analgesia was given was 19.3 hours with standard deviation of ± 3 hours. In the present study Inj. diclofenac sodium 75 mg IV was given as a part of rescue analgesia when VAS score exceeded 3.
No adverse systemic toxicity of Bupivacaine such as seizure, arrhythmia or cardiovascular collapse was noted. Neither vascular puncture nor paresthesia occurred. No complications, such as hematoma, infection or persistent paresthesia were observed within 24 hours after the operation.
Discussion
There are not many publications or research available over pain relief in below knee orthopaedic surgery or trauma. Hence, an attempt was made to study the efficacy of single-shot sciatic nerve block for postoperative pain management in below knee orthopaedic surgery. We performed an observational study in 60 patients undergoing below knee orthopaedic surgery who received single shot sciatic nerve block for postoperative pain relief.
Parker et al., reported that sciatic nerve block reduced pain score and analgesic requirements [14]. Monsó A et al., studied 312 cases of sciatic nerve block in the popliteal fossa for surgery of the dorsal foot. They reported that duration of analgesia was 6 hours 15 min (range 3-16 hours) [15]. Sinardi D et al., compared bupivacaine and ropivacaine in sciatic nerve block. They reported that duration of analgesia for ropivacaine and bupivacaine was 16 hours and 13 hours respectively [9]. Young DS et al., conducted a retrospective cohort study on 78 consecutive patients who had a total ankle arthroplasty from October 2006 to June 2013. They concluded that infragluteal peripheral nerve block as a means of postoperative pain control in patients undergoing a total ankle replacement was associated with significantly decreased opioid use compared to patients receiving no peripheral nerve block [11].
Mendicino RW et al., studied use of sciatic popliteal nerve blocks in conjunction with common peroneal and saphenous nerve blocks. They reported reduced requirement of opioids postoperatively [8]. Rongstad K et al., evaluated 86 patients after giving sciatic nerve block in major foot or ankle operation. The block lasted an average of 20 hours [6]. Casati A et al., studied 45 healthy patients undergoing hallux valgus repair. They concluded that 0.75% levobupivacaine provides a shorter onset time than 0.5% levobupivacaine and a longer duration of postoperative analgesia than both 0.5% levobupivacaine and 0.75% ropivacaine with reduced need for rescue analgesia after surgery [10]. McLeod et al., reported that the lateral popliteal block with 0.5% bupivacaine lasted 18 hours [16]. In the present study, the mean time of rescue analgesia given was 19.3 hours.
Monsó A et al., reported no complications or sequelae after sciatic nerve blocks. They concluded that the technique was highly effective and comfortable for patients, as it required only one puncture and provided good postoperative analgesia with no major side effects [15]. Mendicino RW et al., reported less undesirable adverse effects associated with these drugs [8]. The aforesaid studies are comparable with present research.
Limitation
There were few limitations in the present research such as the onset of sciatic nerve block could not be assessed because subarchanoid block was given immediately after sciatic nerve block and the patients could not be observed after 24 hours due to logistic issues. Also, we have not compared the two groups like one with only spinal anaesthesia and the other with spinal anaesthesia along with sciatic nerve block.
Conclusion
Single shot sciatic nerve block provided effective pain relief to majority of the patients up to 18 hours in below knee orthopaedic surgery and also decreased analgesic drugs requirement postoperatively. Patients remained haemodynamically stable after the sciatic nerve block. Sciatic nerve block was found to be safe with no adverse effects.
Authors’ Contribution
Author 1: Research design, Collection of data, writing research paper draft, revising it critically, approving the submitted version.
Author 2 Research design, interpretation of data, approving the submitted version.
Author 3: Research design, Analysis of data, interpretation of data, writing research paper draft, revising it critically, approving the submitted version.