Caudal analgesia, in the recent years, is the preferred technique in paediatric pain management both intraoperative and postoperative, for lower abdominal and lower limb surgeries. This is because it is simple, easy to perform and the level of blockade achieved is predictable. The drawback of single shot caudal analgesia is its short duration of action and this necessitates either the insertion of a catheter or the use of an adjuvant with inherent limitations. Opioids [1], midazolam [2], neostigmine [2], tramadol [3], clonidine [3,4], ketamine, [2,4], and have been used for caudal block with various results.
Clonidine, an alpha2-adrenergic agonist produces analgesia without causing significant respiratory depression after caudal administration in children [5]. Using clonidine as an adjuvant enables us to use a lower concentration of the local anaesthetic to achieve the same level of analgesia with the advantages of prolonged duration of analgesia, reduced residual motor blockade and increased margin of safety [6]. However, clonidine can cause hypotension and bradycardia [7]. Studies have shown that clonidine in a dose of 1 μg/kg added to 0.25% Bupivacaine produced significant prolongation of caudal block in children [8] and was as effective as 2 μg /kg [9,10].
Few studies have evaluated the addition of 1 μg/kg Clonidine to 0.125% Bupivacaine for caudal analgesia [11,12].
To evaluate the efficacy and side effects of caudal clonidine in a low dose of 1μg/kg combined with a low concentration of 0.125% solution of bupivacaine.
Materials and Methods
A prospective, randomized, double-blind, controlled study was conducted after the approval of the Institutional Ethical Committee and parental informed consent, in 60 patients, over 18 months, from May 2010 to November 2011. They were between 1-10 years of age, of ASA Physical Status I, weighing 5-20 kg, scheduled to undergo infraumbilical operations in a tertiary hospital. Exclusion criteria were: contraindication to caudal blockade, history of allergic reaction to Bupivacaine or Clonidine, ASA Physical Status > I and parental refusal.
Sample size was calculated based on a previous study [11] with a minimum requirement of 30 patients in each group and there were no drop outs. Prior to surgery, the children were kept nil per oral according to standard guidelines. They were randomly assigned to either study groups B or BC, for caudal analgesia.
Group: B: 1ml/kg of 0.125% Bupivacaine solution.
Group: BC: Mixture of 1ml/kg of 0.125% Bupivacaine with preservative free Clonidine 1μ/kg. The solution was prepared by an Anaesthesiologist who was not one of the observers for the study.
All the patients were premedicated with midazolam 0.75 mg/kg orally 30 minutes prior to induction of anaesthesia. In the operation theatre, patients were connected to Datex Ohmeda A-5 multipara monitor and Heart Rate (HR), Mean Arterial Blood Pressure (MAP) and oxygen saturation (SpO2) were monitored. General anaesthesia was induced with thiopentone (1.25%) 5 mg/kg via 22-G or 24-G IV cannula and inhalation of oxygen, nitrous oxide and sevoflurane.
Caudal block was given in left lateral position with a 23 G short bevelled needle with due aseptic precautions after “Swoosh” test and negative aspiration of blood and CSF. Anaesthesia was maintained using nitrous oxide (66%), oxygen (33%) and sevoflurane (2.5% - 3.5%) for the first 10-15 minute via a Jackson Rees circuit and thereafter, only with oxygen and Nitrous Oxide with spontaneous ventilation. Surgery commenced 15-20 minutes after the caudal block.
Monitoring of heart rate and oxygen saturation was done continuously and mean arterial pressure, every 5 minutes during surgery. They were recorded prior to induction of anaesthesia and then every 5 minutes after the administration of caudal analgesia for the first 30 minutes and thereafter every 15 minutes till the end of surgery. Postoperatively every 15 minutes for 2 hours in the recovery room, then 2 hourly for 4 hours and thereafter every 4 hourly until 24 hours.
Intraoperative analgesic efficacy was defined by haemodynamic stability - absence of an increase in HR and MAP > 15% of pre incision baseline values. If this occurred, within 20 minutes, it was considered as failure of caudal anaesthesia and the patient was given a rescue analgesic Fentanyl 2 μ/kg IV and was excluded from the study. An intraoperative decrease in MAP or HR by more than 30% after caudal anaesthesia was defined as hypotension and bradycardia respectively and was treated by IV fluids, ephedrine or atropine accordingly. Lactated Ringer’s solution was used as intraoperative fluid according to the Holliday and Segar formula (4-2-1 rule). Postoperatively subjects were given 5% dextrose in 0.45% normal saline. Nitrous oxide was cut off during skin suturing.
Postoperative pain was assessed at the end of 2 hours and thereafter 2 hourly for 6 hours, then 4 hourly for 24 hours by the 5 point verbal pain score as follows [13].
Asleep
Awake but no pain.
Mild pain (on touching area or movement)
Moderate pain (constantly cries or complains of pain)
Severe pain (uncontrollable or excessive crying)
Absolute analgesia duration was noted. It was defined as the time from caudal injection until the pain score was II or less [2].
Patients were given oral paracetamol syrup 15mg/kg body weight as rescue analgesic for a pain score of IV or V during the first 24 hours after surgery. Time at which the first rescue analgesic was given and the number of analgesic doses required was noted.
Sedation score was assessed at 2 hours postoperative and then 2 hourly for 6 hours by the – 4 point patient sedation score (PPS) as follows [14]:
Asleep not arousable.
Asleep arousable by verbal contract.
Drowsy.
Alert Awake.
Motor block was assessed at the end of 2 hours in the recovery room and at the end of 6 hours to detect any residual motor weakness by using a modified Bromage scale [15] that consisted of 4 points as follows:
0 = full motor strength (during flexion of knees & feet)
1 = little flexion of knees and feet
2 = little movement of feet only
3 = no movement of knees and feet
Those children who could not move their legs on commands were given a tactile stimulus on their legs and feet.
The incidence of adverse effects postoperatively such as respiratory depression (SpO2 <95%) [16], abnormal behaviour and postoperative vomiting was also evaluated. An episode of vomiting was defined as either vomiting (expulsion of stomach contents) or retching (an involuntary attempt to vomit but not productive of stomach contents).
Statistical Analysis
The data thus obtained was expressed as mean ± standard deviation for quantitative variables and in percentage for categorical ones. The unpaired student’s t-test and Chi-square test were used for inter group comparison. A p-value of < 0.05 was considered to be statistically significant.
Results
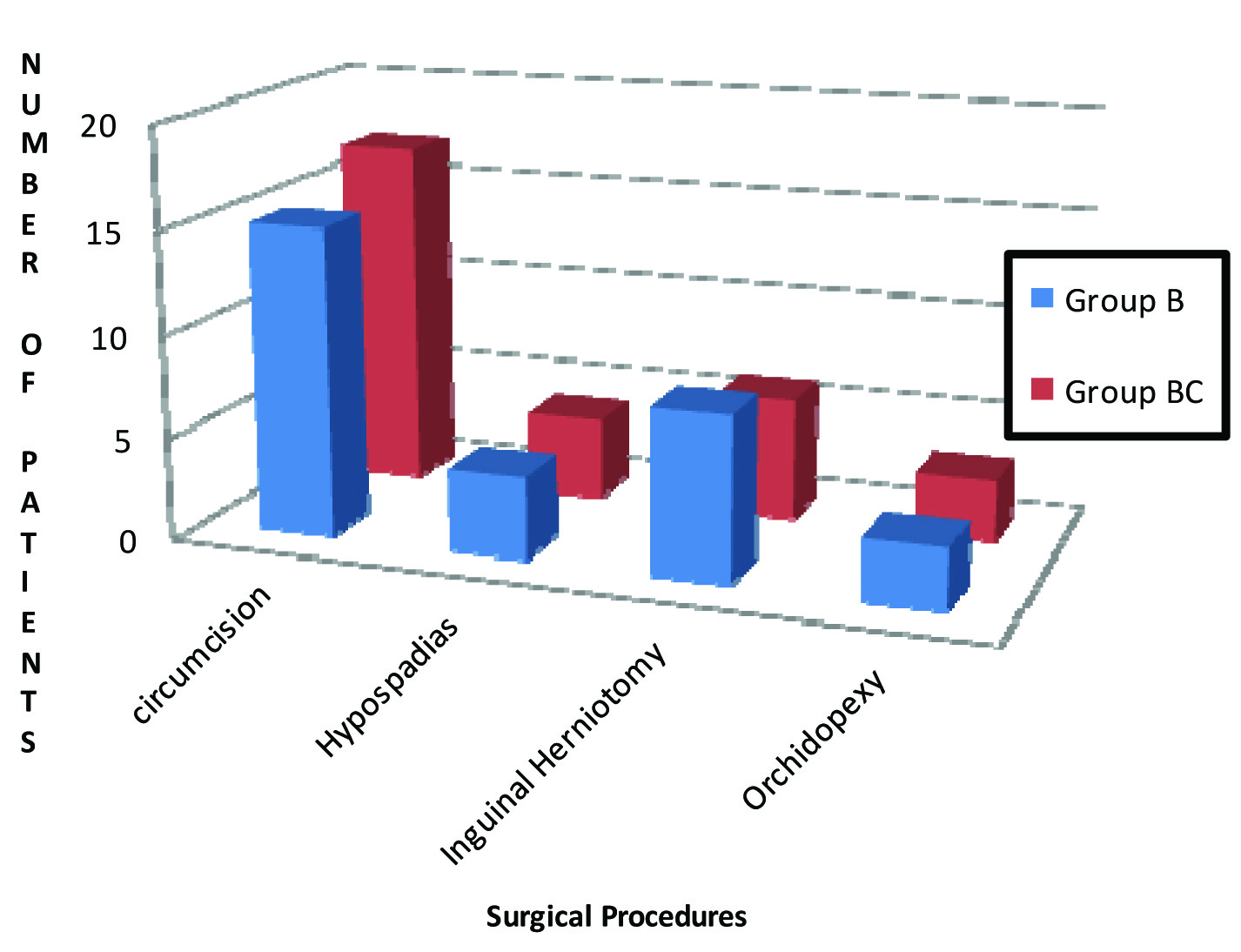
The two groups B and BC were comparable in age, weight and duration of surgery [Table/Fig-1] and also in the type of surgical procedures performed [Table/Fig-2] and the dermatomal level of anaesthesia required. The maximum duration of absolute analgesia in group B was 4 hours and in group BC was 16 hours, while the minimum duration of absolute analgesia in group B was 2 hours and in group BC was 6 hours. The mean duration of postoperative analgesia in group BC was longer than in group B [Table/Fig-3]. This was statistically highly significant with p-value of 0.001. The number of doses of rescue analgesics received postoperatively in both the groups is seen in [Table/Fig-4]. The mean in group B was 3.46±0.57 and in group BC was 1.9±0.48 which was statistically highly significant (p-value of 0.004).
Patient characteristics and duration of surgery.
| Characteristic | Group | Mean ± SD | p-value |
|---|
| Age (Years) | B | 4.63±1.73 | 0.30 |
| BC | 4.43±1.52 |
| Weight (kg) | B | 12.76±3.21 | 0.70 |
| BC | 13.10±3.48 |
| Duration of Surgery (minutes) | B | 32.1±30.618 | 0.8919 |
| BC | 31.03±31. |
Comparison of different surgical procedures in the two groups.
Duration of absolute analgesia (hours) after caudal block.
| Group | Mean Duration of Absolute analgesia (hours) | SD |
|---|
| B | 3.20 | ±0.99 |
| BC | 10.60 | ± 1.90 |
No. of patients receiving postoperative rescue analgesic during the first 24 hours after surgery.
| Number of doses of Rescue Analgesics | Group B | Group BC |
|---|
| 1 | 0 | 5 |
| 2 | 0 | 23 |
| 3 | 17 | 2 |
| 4 | 12 | 0 |
| 5 | 1 | 0 |
Intraoperative and postoperative heart rate in group B and Group BC were comparable. So also the mean arterial pressures in group B and group BC were comparable [Table/Fig-5].
Mean and Std. Deviation (SD) of Intraoperative and post-operative HR and MAP in the two groups.
| Variable | Group BMean (SD) | Group BCMean (SD) | p-value |
|---|
| Intra-operative HR (beats/min) | 114.75 ± (8.30) | 111.7 ± (8.72) | 0.17 |
| Postoperative HR (beats/min) | 111.23 ± (9.9) | 108.9 ± (10.16) | 0.38 |
| Intra-operative MAP (mm of Hg) | 63.5 ± (9.67) | 62.32 ± (9.02) | 0.61 |
| Postoperative MAP (mm of Hg) | 62.5 ± (8.6) | 61.9 ± (9.9) | 0.8 |
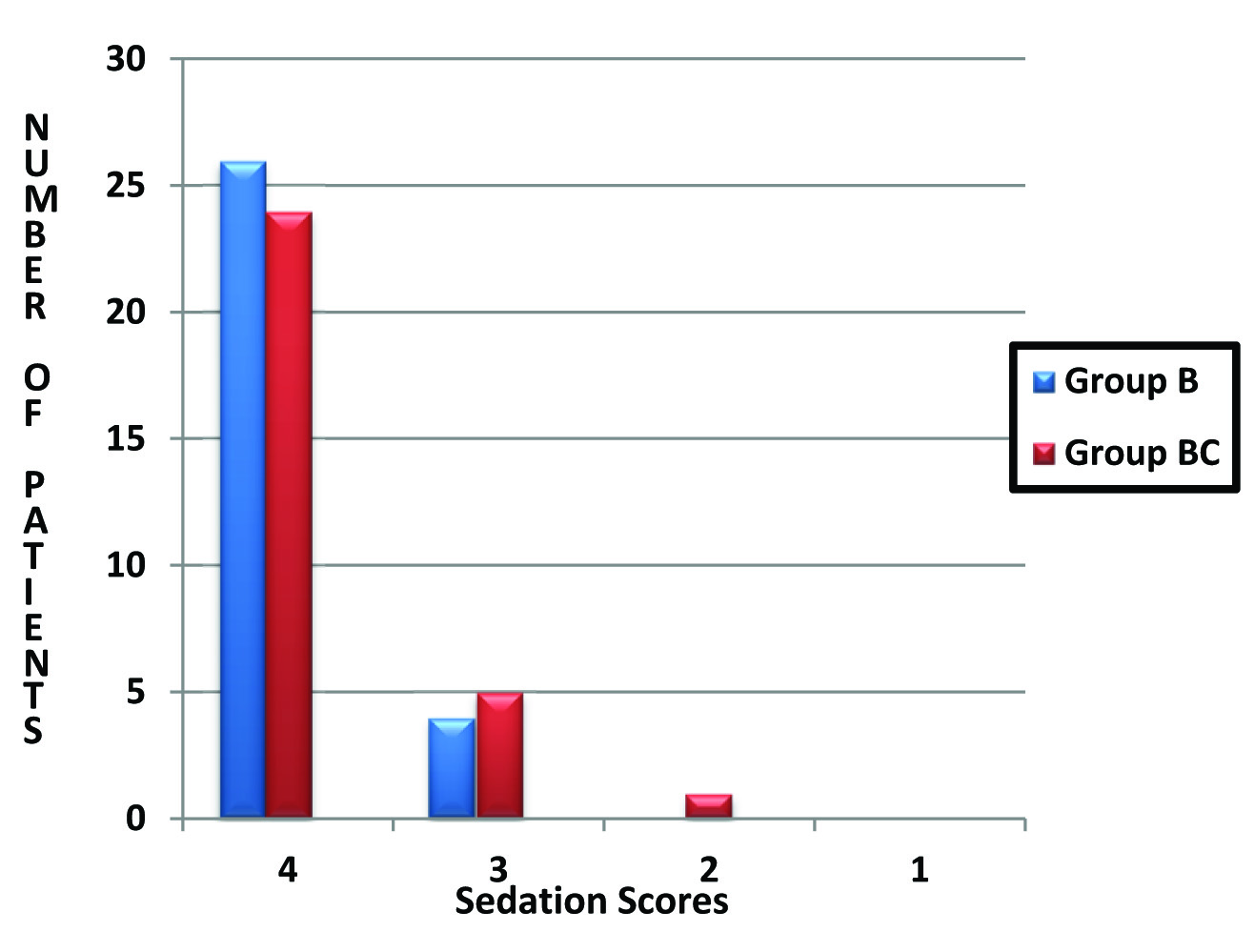
The sedation score in both the groups B and BC at 2 hours are given in [Table/Fig-6].
Comparison of postoperative sedation scores at 2 hours.
The incidence of side effects was similar in both the groups. Vomiting was seen in 10% of patients in group B and 6.6% of patients in group BC. There was neither respiratory depression nor abnormal behavior in any of patients in both the groups. There was no residual motor weakness at the end of 6 hours in either of the groups.
Discussion
Pain in children, if left untreated, can result in morbidity and mortality [17] and research in management of postoperative pain in paediatric surgery is on-going.
Clonidine was demonstrated to have an analgesic action when administered via epidural route [18]. It was later used in paediatric caudal block and it was found to prolong analgesia in children [8,10,11,19,20]. It is also being used intrathecally [21]. Caudal clonidine, combined with bupivacaine has been used in different doses and it was found that increasing the dose of clonidine from 1 μg/kg to 2 μg/kg did not enhance its efficacy [8,14,22]. However, hypotension and bradycardia was seen as a side effect in a dose dependent manner, the incidence being less with 1μg /kg [23]. Thus, we chose Clonidine in a dose of 1μg/kg to achieve effective prolongation of caudal block with a smaller dose [8,14,22] and lesser incidence of hypotension, bradycardia [23] and respiratory depression [24]. Dr. Manickam et al., have also demonstrated that clonidine 1μg /kg provided increased duration and better quality of pain relief with no motor blocakade and sedation when added to 0.1% ropivacaine compared to plain 0.1% ropivacaine and 0.2% ropivacaine [25].
We chose 1ml/kg of 0.125% Bupivacaine according to the prescription scheme of Armitage [26]. Secondly, Sharp et al., speculated that a small volume of Bupivacaine (0.5ml/kg) may not be able to deliver the Clonidine upto the spinal cord, leaving only direct action on nerve roots in the caudal area [22]. A 0.125% of Bupivacaine was chosen to avoid residual motor blockade during postoperative period, which can otherwise lead to having a confused and restless child. In a study by Giorgio et al., made comparison of three different concentrations of levobupivacaine in caudal [27]. Bupivacaine and levobupivacaine are considered to be “equipotent.” A 0.125% of Bupivacaine is associated with less motor block but a shorter duration of postoperative analgesia in comparison to 0.25% and 0.20% Bupivacaine according to the above study.
Our study indicates that for caudal block, the addition of clonidine 1μg/kg to 1ml/kg of 0.125% of Bupivacaine significantly prolongs the duration of analgesia (mean 10.60 hours) then caudal Bupivacaine 1 ml/kg of 0.125% alone (mean 3.2 hours). This confirms with previous study by Tripi PA et al., wherein addition of Clonidine 1 μg/kg to 1ml/kg of Bupivacaine (0.125%) significantly increased the duration of caudal analgesia (8 hours) (3.9 hours for plain bupivacaine group) and decreased postoperative morphine requirement in children undergoing ureteroneocystostomy [12]. The duration of analgesia in the 2ug/kg clonidine group in a study conducted by Aruna et al., was 10 hours, while that in the plain bupivacaine group was 4.5 hours, which was similar to other studies [28]. Several mechanisms have been postulated. Clonidine combines with alpha 2 adrenoceptors at spinal and supraspinal sites, after crossing the blood brain barrier and produces analgesia. Secondly, it causes a direct suppression of the spinal cord nociceptive neurons. Also, the peripheral sensory A δ and C nerve fibre neurotransmission, is suppressed by clonidine. The last mechanism suggested is related to its pharmacokinetics: by inducing vasoconstriction through α -2b adrenoceptors which are located at the peripheral vascular smooth muscles [29].
In our study, 76% children in Bupivacaine-Clonidine required only 2 doses of postoperative analgesia compared with 96% of children in Bupivacaine group requiring three or more doses. The bupivacaine-clonidine group required significantly lesser number of analgesic doses postoperatively as compared to Bupivacaine group (p-value of 0.004) which is statistically highly significant. This compares well with a study by Cook et al., in which the number of doses of postoperative analgesics required were significantly greater in Bupivacaine group compared with the group containing Bupivacaine and Clonidine together [4]. In a study by Aruna Parameswari et al., the number of patients requiring 2 or 3 doses of rescue analgesic was more in the Bupivacaine group compared to patients in clonidine with bupivacaine group [28].
The degree of sedation in the first two hours following caudal block was similar between the two groups in our study. This is comparable to studies [12,25,30] wherein the sedation scores were similar in both the groups. However, Lee et al., noted significant sedation with 2 μg/kg clonidine added to caudal bupivacaine [10]. They attributed it to the analgesia offered by clonidine.
Neuroaxial Clonidine can produce hypotension as a result of inhibition of preganglionic sympathetic fibres and bradycardia due to parasympathetic predominance [7]. In our study there was no statistically significant difference between the two groups with respect to heart rate and mean arterial pressure both during the intraoperative and postoperative period. This compares well with a study by Aruna Parameswari et al., [28]. Gupta S et al., observed a fall in MAP and heart rate with caudal 2 μg/kg clonidine in 0.2% ropivacaine but it got stabilized to normal within 20-30 minutes [31].
There was no respiratory depression in either of the groups as also seen in a study by Lak M et al., [32]. All patients were able to move their legs at the end of six hours and there was no urinary retention which is similar to a study by Archna Koul [5]. The incidence of vomiting was found to be similar in both the groups in our study. In a study by Archna Koul, there was no vomiting except in two patients in the Bupivacaine group [5]. Our study compares well with these studies suggesting that there is no increased incidence of side effects when 1ug/kg clonidine is added to caudal Bupivacaine.
Dobereiner et al., have shown that ropivacaine is preferred if motor block is to be minimized [33]. When ropivacaine is not available, we suggest the use of 0.125% Bupivacaine along with 1μg/kg clonidine as the low concentration of Bupivacaine will minimize the motor block while at the same time clonidine added to it will prolong the analgesia.
Conclusion
Caudal clonidine in the dose of 1 μg/kg in children is a satisfactory and efficacious adjuvant to caudal bupivacaine for producing prolonged postoperative analgesia with minimum side effects.
Short fall: We were unable to use the visual analog scale (10-cm horizontal scale) as the age group ranged from 1-10 years and the older children were unable to understand it.