Unique Application of Cryocone to Diagnose Umbilical Pilonidal Cyst
Kimberly Mallin1, Sudhakar Pemminati2
1 Professor and Director of AUA Health Center, American University of Antigua, College of Medicine, Antigua, West Indies.
2 Associate Professor, Department of Medical Pharmacology, AUA College of Medicine and Manipal University, Antigua, West Indies.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kimberly Mallin, Professor and Director of AUA Health Center, American University of Antigua, College of Medicine, University Park, Jabberwock, Coolidge, Antigua, W.I. (268) 484-8900.
E-mail: kmallin@auamed.net
Patients with umbilical disorders who present with complaints of a mass, pain, tenderness or discharge will typically have a differential diagnosis including umbilical hernias, pyogenic granuloma, endometriosis, Sister Mary Joseph nodule and urachal or epidermoid cysts. We would add the inclusion of pilonidal sinus disease and present the case of a patient with an umbilical pilonidal cyst. The use of a cryocone with lubricating jelly, in this case, proved to be an easy and convenient method that aided in visualization and diagnosis of this fairly uncommon condition.
Belly button, Conservative method, Men, Umbilectomy, Umbilicus discharge
Case Report
A 41-year-old healthy non-obese male presented to the clinic with three month history of discharge from umbilicus. Initially the discharge was thick, brown and foul-smelling, he began cleaning his umbilicus superficially and discharge became thinner, blood stained and non-foul smelling. He had no other symptoms except mild discomfort while pulling his belt over umbilicus. His laboratory tests were unremarkable and his physical exam was normal. He had a hirsute chest and abdomen. Upon examination, he was found to have an umbilicus with depth of 2.5cm and 1cm wide, as well as a 1.5mm cyst, identified at the upper part of the umbilicus. There was serosanguineous drainage in the lower portion of the umbilicus with what appeared to be coarse hair.
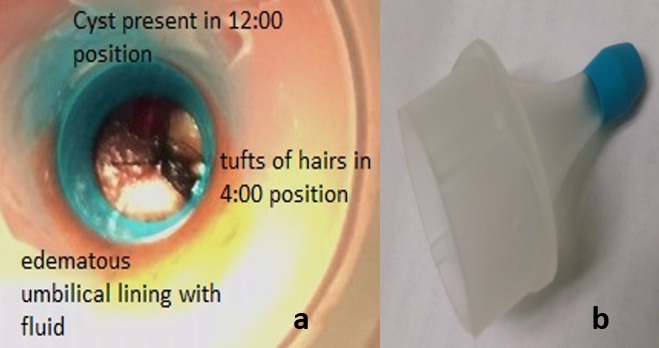
He was advised to clean umbilicus twice a day, keep it dry and apply topical antibiotics like Nebasulf (neomycin + bacitracin + sulphacetamide) daily and follow-up in one week. He returned to the clinic with improvement of the drainage. We attempted to better visualize the bottom of umbilicus now that the drainage had improved. Using a 7mm diameter cryocone with lubricating jelly [Table/Fig-1a,b]. We were able to visualize tufts of hair at the umbilical base. We advised the patient to continue current management and follow up in a week.
(1a) Visualization of cyst and accumulated hair at the bottom. (1b) A 7mm cryocone.
The patient attempted using a sterile ear bud, succeeding in removing much of the detritus, which was composed of more than 80 very thick, coarse hairs, ranging in length from 3mm to 15mm [Table/Fig-2a]. There were several hairs left intact in the epidermis at the umbilicus base.
During intervention and after removal of the hair. Removal of accumulated hair with sterile ear bud and last visit with normal umbilicus without cyst or oedema.
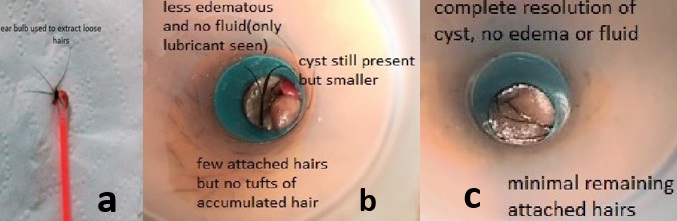
The following week he was re-examined. The cyst was markedly decreased in size, with only 5-6 remaining loose hair, which were removed using forceps [Table/Fig-2b]. There remained 2-3 intact hair at the base. The patient was advised to continue current management. A follow-up visit in a month later showed complete resolution of cyst, few remaining attached hair with no discharge or oedema [Table/Fig-2c].
With this case experience, we advise a simple method to remove accumulated umbilical hair. First, to clean the umbilicus, then slowly insert sterile ear bud to the bottom of the umbilicus, turn ear bub either clock wise or counter clock wise smoothly (to avoid too much curling as that causes pain due to the intact hair pulling the skin) and then remove the ear bud. This technique removes the accumulated hair from the bottom of umbilicus. This method also helps to identify the intact hair at the bottom.
Discussion
Umbilical Pilonidal Sinus (UPS) is an unusual condition that presents similar to other more common umbilical disorders such as hernia, endometriosis, urachus, epidermoid cysts, pyogenic granulomas, metastatic tumors and congenital abnormalities [1]. Anderson first described UPS in 1847 [2]. It is usually seen in hirsute males with deep umbilicus, however, there are other factors which play a role in the development of UPS; wearing tight clothes, family history of UPS, less frequency of bathing and wearing belts. Loose hair gets caught in the umbilicus and friction (often due to tight clothes or belts) causes the thick hair to penetrate the umbilical epidermis, leading to a foreign body reaction consisting of oedema and drainage [3]. Multiple publications discuss causative factors, as well as reviewing treatment options ranging from conservative measures to umbilectomy [4–7], including an algorithm to aid with decision making [6]. There are no studies with specific mention of techniques used to visualize the umbilical base, necessary both for diagnosis and excision of detritus. Use of ultrasound, fistulography and CT scan is discussed along with “good lighting conditions and the help of an assistant to retract the skin of the umbilicus, hairs can be seen deep in the umbilicus and usually protrude from a small sinus” [1,8]. We initially tried to visualize the umbilicus using an otoscope and while we were able to visualize the umbilicus better, it was not optimal. Use of the cryocone allowed us to visualize the entire umbilicus and easily extract any debris.
As a result of this experience, we recommend hirsute males with deep umbilicus to clean umbilicus thoroughly with sterile ear bud, decrease friction to the umbilicus by wearing belts below the umbilicus and avoid very tight clothing. When patients present with abdominal complaints, especially with umbilical discharge, we recommend evaluating the umbilicus with cryocone and proper light to look for hair tufts and should any be found, removal of such hair with tools as discussed, followed by a strict cleaning regimen and use of antibiotic powder/ointment.
Conclusion
To the best of our knowledge this is the first report on the use of common office equipment such as a cryocone, which in the present case provided a better visualization and access tha helped us in the diagnosis and treatment of UPS. We suggest that pilonidal sinus disease be included in the differential diagnosis of umbilical symptoms and that CT scans and/or ultrasound are not always necessary for diagnostic purposes.
[1]. Kabay S, Olgun E G, Yucel M, Yaylak F, Hacioglu A, A rare case of pilonidal sinus of the umbilicusCentral European Journal of Urology 2009 62(2):116-17. [Google Scholar]
[2]. Brearley R, Pilonidal sinus a new theory of originBr J Surg 1955 43:62-68. [Google Scholar]
[3]. Coskun A, Bulus H, FarukAkıncı O, Ozgönül A, Etiological factors in umbilical pilonidal sinusIndian J Surg 2011 73(1):54-57. [Google Scholar]
[4]. Kareem T, Outcomes of conservative treatment of 134 cases of umbilical pilonidal sinusWorld J Surg 2013 37(2):313-17. [Google Scholar]
[5]. Eryilmaz R, Sahin M, Okan I, Alimoglu O, Somay A, Umbilical pilonidal sinus disease: predisposing factors and treatmentWorld J Surg 2005 29(9):1158-60. [Google Scholar]
[6]. Sozen S, Kanat BH, Kanat Z, Bali I, Polat Y, Effective conservative treatment of umbilical pilonidal sinus disease: Silver nitrate? Salt?Ann Ital Chir 2015 86:450-55. [Google Scholar]
[7]. Ponten JB, Ponten JE, Luyer MD, Nienhuijs SW, An umbilical surprise: a collective review on umbilical pilonidal sinus: An uncommon alternative diagnosis in common umbilical symptomsHernia 2016 20(4):497-504. [Google Scholar]
[8]. McClenathan JH, Umbilical Pilonidal SinusCan J Surg 2000 43(3):225 [Google Scholar]