Prosthodontic Rehabilitation of Accidental Maxillofacial Gunshot Injury Using Dental Implants: A Five Year Follow-Up Clinical Report
Vinod Balla1, Angleena Y Daniel2, Nirmal Kurian3
1 Associate Professor, Department of Prosthodontics, Christian Dental College, CMC, Ludhiana, Punjab, India.
2 Associate Professor, Department of Prosthodontics, Christian Dental College, CMC, Ludhiana, Punjab, India.
3 Postgraduate Student, Department of Prosthodontics, Christian Dental College, CMC, Ludhiana, Punjab, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nirmal Kurian, Christian Dental College, Brown Road, Ludhiana-141008, Punjab, India.
E-mail: nirmal36@gmail.Com
Gunshot injuries to the face can have serious aesthetic, functional, and psychological consequences. The incapacitating nature of maxillofacial defects makes reconstruction of the maxilla and mandible challenging, owing to multiple surgeries and extensive rehabilitation phase. Outcome of prosthodontic treatment is one of the important parameters by which a patient measures the success of rehabilitation. A 5-year follow-up of comprehensive surgical and prosthodontic reconstruction of a gunshot injury using dental implants is described. This case report illustrates the contribution of immediate dental implants with proper oral hygiene follow-up as an effective treatment modality in restoring a patient to near normal function and aesthetics.
CAD-CAM abutment, Reconstruction, Sectional tray
Case Report
A 30 year old male patient, conscious and well oriented, presented to trauma center with alleged history of gunshot injury while cleaning his gun. Extra orally patient suffered multiple lacerations on cheek, upper and lower lip and bridge of nose. Intraoral examination revealed lacerations on palate, lower lip, buccal mucosa and tongue with multiple fractured and avulsed teeth [Table/Fig-1]. Patients beard was shaven for better clinical evaluation and wound management. The wound was cleaned and patient was sent for radiographic evaluation which revealed multiple bullet splinters in soft tissue. Five pellets were retrieved during debridement and teeth with poor prognosis were extracted.
Clinical presentation of patient at trauma centre.

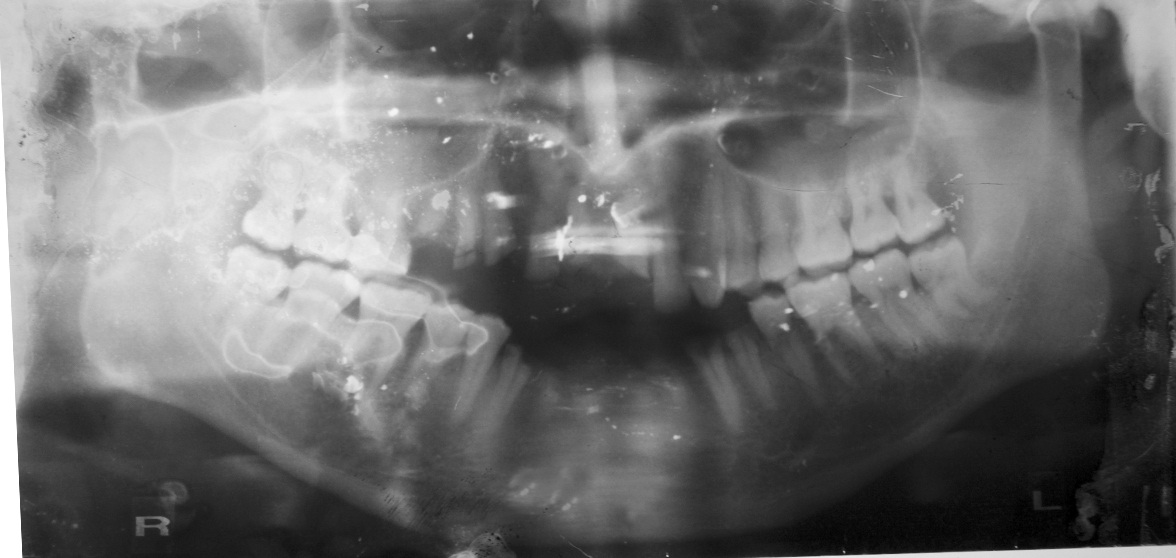
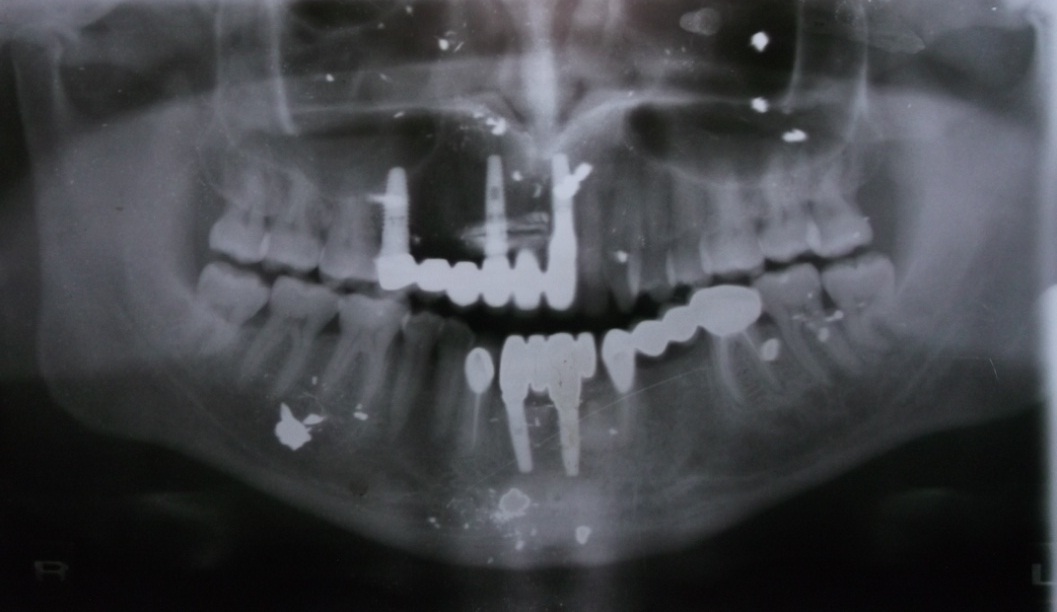
Intraoral examination one month post trauma revealed multiple fractured teeth #15, 14,13, 12, 11, 21, 32, 33, 34, 35, 43 and missing teeth #42, 41 [Table/Fig-2,3]. The mouth opening was reduced as a result of wound contracture.
OPG showing multiple fractured and missing teeth.
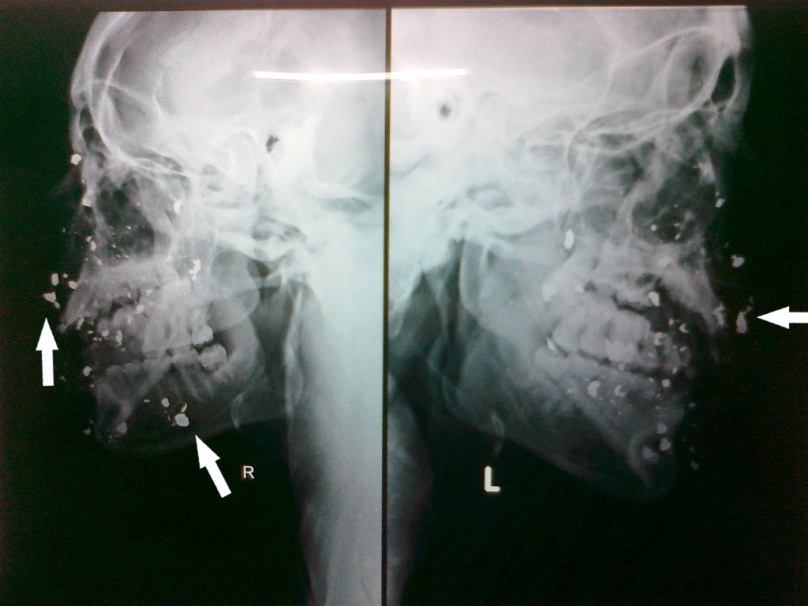
Lateral cephalogram showing bullet splinters in soft tissue.
Fractured teeth with pulpal involvement were treated endodontically. A treatment plan for restoring missing maxillary anterior and mandibular premolar teeth with implant retained fixed dental prostheses and immediate implant placement following extraction of #42, 41, 31, was formulated. Due to financial constraints patient opted for tooth retained fixed dental prosthesis for replacement of #34, 35 and implant retained Fixed Dental Prosthesis (FDP) for maxillary and mandibular incisors. Five endosseous implants of 3.5mm X 13mm were placed at the region of #42, #32 and 4.3mm X 13mm at the region of teeth #21 and #12 and 5.0mm X 11.5mm implants at #15 (Nobel Replace Select Tapered TiU NP). Absence of buccal cortical plate at canine region which was removed during debridement made implant insertion at #13 region contradictory.
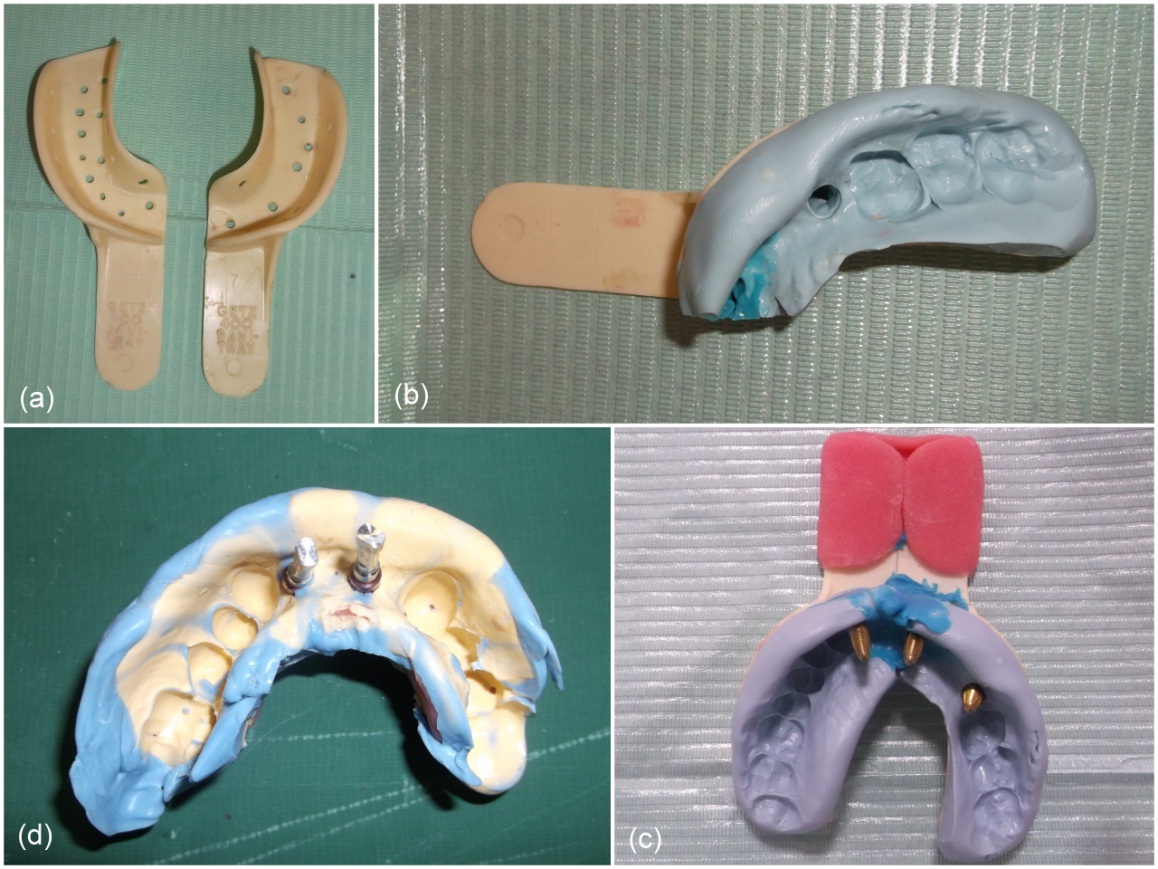
Second stage surgery was performed and gingival former were placed. Definitive impression was made with polyvinyl siloxane elastomeric impression material (AFFINIS, Coltene, Switzerland) utilizing customised sectional trays for maxillary teeth. Two sections of impressions were assembled and master cast was poured [Table/Fig-4].
(a) Sectional trays; (b) Sectional impression; (c) Assembled sectional impressions showing transfer copings in position for maxillary impression; (d) Mandibular impression with implant analogues.
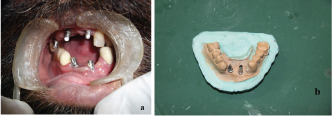
CAD-CAM milled implant abutments were made for mandibular implants [Table/Fig-5a,5b]. Porcelain fused to metal FDP was luted using polymeric implant cement (Implacem, Equinox Medical Technologies B V Holland) [Table/Fig-6]. Post op OPG immediately following cementation of implant retained fixed dental prosthesis revealed satisfactory treatment outcome [Table/Fig-7]. Patient was scheduled for regular follow-up every two months for the first six months and thereafter once in every six months and oral prophylaxis using special plastic tips was carried out during each appointment. Five year follow-up has revealed excellent stability of the implants and prosthetic restorations confirming good prognosis [Table/Fig-8].
(a) Intra oral image showing implant abutments. (b) CAD-CAM milled custom made abutments.
Porcelain fused to metal crowns replacing missing maxillary and mandibular teeth.

Post operative OPG immediately following cementation of implant retained fixed dental prosthesis.
Five year follow-up OPG showing good prognosis of implants and prosthetic restorations along with bullet splinters in soft tissue.

Discussion
Gunshot injuries to the face can have serious esthetic, functional, and psychological consequences. The head and neck region is one of the most commonly affected areas in gunshot injuries which constitute more than 50% of attempted suicides, 14% of assaults, and 12% of accidental injuries [1].
The incapacitating nature of maxillofacial defects makes reconstruction of the maxilla and mandible challenging, owing to multiple surgeries and extensive rehabilitation phase. These patients may also demonstrate signs and symptoms consistent with anxiety, depression, or post-traumatic stress disorder [2]. Restoration of the structural integrity as well as rehabilitation to achieve functional and esthetic demands should be the primary goal of treatment [3].
Gunshot wound rehabilitation represents a major challenge to both surgeons and prosthodontic specialists [4,5]. Injuries of this type can cause extensive destruction and avulsion of bone and soft tissues in oral and maxillofacial region which may be exceedingly difficult to reconstruct and restore to normal.
The severity of the facial gunshot injuries varies according to the caliber of the weapon used and to the distance from which the patient sustained the injury. Close range, high velocity gunshot wounds can result in devastating functional and esthetic consequences for the surviving patients. The patient reported with close range injury causing extensive soft tissue laceration and significant damages to dentoalveolar structures. An early definitive treatment of facial wounds was done based on the criteria outlined by Manson for management of gunshot injury wounds [5].
Several authors have illustrated the successful use of osseointegrated implants in the reconstruction of traumatic craniomaxillofacial injuries secondary to gunshot [6,7]. Reduced mouth opening as a result of tissue scarring in the buccal mucosa was a major obstacle in rehabilitation phase, hence, a modified impression technique that incorporated the use of sectional impression trays was adopted for maxillary impressions [8–10]. Sectional trays were selected and joined at the handle with acrylic to reassemble the sections after individual impressions.
The preformed prosthetic abutments had insufficient height to support the prosthesis and hence, CAD-CAM milled custom made abutments were fabricated for mandibular implants. Bullet splinters were found not to elicit any foreign body reactions and patient was symptom free during the course of treatment. The clinical decision to remove an inert object has to be weighed against potential damage that could be created during a search for the object [11]. Considering the inert nature, need for further invasive surgery and patients reluctance for the same, they were left behind without further intervention.
In reconstructed patients, good results can be achieved with the use of dental implants and implant-supported prostheses with immediate loading [12,13] . Special plastic scaling tips were used during maintenance phase as research has shown that the use of plastic scalers produced insignificant alteration of the titanium implant surface following instrumentation which makes these the recommended choice for scaling titanium implant surfaces [14,15].
Conclusion
A 5-year follow-up of comprehensive surgical and prosthodontic reconstruction of a gunshot injury using dental implants is described. This treatment illustrates the contribution of immediate dental implants with proper oral hygiene follow-up as an effective treatment modality in restoring a patient to near normal function and aesthetics.
[1]. Bidra AS, Veeranki AN, Surgical and prosthodontic reconstruction of a gunshot injury of the mandible using dental implants and an acrylic resin fixed prosthesis: A clinical reportJ Prosthet Dent 2010 104(3):142-48. [Google Scholar]
[2]. Kelly P, Drago CJ, Surgical and prosthodontic treatment of a patient with significant trauma to the middle and lower face secondary to a gunshot wound: A clinical reportInt J Prosthodont 2009 18(7):626-37. [Google Scholar]
[3]. Cakan U, Anil N, Aslan Y, Prosthetic rehabilitation of a mandibular gunshot defect with an implant-supported fixed partial denture: A clinical reportJ Prosthet Dent 2006 95(4):274-79. [Google Scholar]
[4]. Zouloumis L, Emmanouil L, Maxillofacial prosthetic reconstruction of a maxillary defect resulting from gunshot wound. A case reportJ Oral Maxillofac Surg 2012 3:151-58. [Google Scholar]
[5]. Thorne CH, Gunshot wounds to the face. Current conceptsClin Plast Surg 1992 19:233-44. [Google Scholar]
[6]. Schneider R, Fridrich K, Chang K, Complex mandibular rehabilitation of a self-inflicted gunshot wound: A clinical reportJ Prosthet Dent 2012 107(3):158-62. [Google Scholar]
[7]. Rajesh Vakil S, Singh BP, Monika B, Immediate placement of endosseous implants in extraction sites - A case reportJ Pierre Fauchard Acad 2009 23(1):36-39. [Google Scholar]
[8]. Arora P, Wazir S, Sharma A, Hinged and sectional complete dentures for restricted mouth opening: A case report and reviewContemp Clin Dent 2013 4(1):74 [Google Scholar]
[9]. Hegde C, Prasad K, Prasad A, Hegde R, Impression tray designs and techniques for complete dentures in cases of microstomia - A reviewJ Prosthodont Res 2012 56(2):142-46. [Google Scholar]
[10]. Uludag B, Polat S, Sahin V, Tokar E, Ertug O, A simplified technique for solving the transfer problem of implant-supported fixed partial dentures for patients with MicrostomiaJ Oral Implantol 2013 39(2):169-71. [Google Scholar]
[11]. Trott A, Trotter T, Wounds and lacerations: Emergency care and closure 1997 Oct 16 United KingdomMosby [Google Scholar]
[12]. Thiago de Almeida Prado Naves Carneiro T, Oliveira MTF, Lima LB, Simamoto-Junior PC, Zanetta-Barbosa D, Immediate loaded implant-supported prosthesis after mandibular reconstruction with free iliac crest bone graftRevista Portuguesa de Estomatologia, Medicina Dentária e Cirurgia Maxilofacial 2015 56(2):117-21. [Google Scholar]
[13]. Mahajan M, Shah N, Accidental lodgment of an air gun pellet in the maxillary sinus of a 6-year old girl: A case reportDent Traumatol 2004 20(3):178-80. [Google Scholar]
[14]. Humphrey S, Implant maintenanceDent Clin North Am 2006 50(3):463-78. [Google Scholar]
[15]. Chen S, Darby I, Dental implants: Maintenance, care and treatment of peri-implant infectionAust Dent J 2003 48(4):212-20. [Google Scholar]