Crossbite: An Orthodontic Exigency
Sushil Kumar1, Abhishek Singha Roy2, Anil Kumar Chandna3, Ankit Garg4, Upender Kumar Chaudhary5
1 Professor and Head, Department of Orthodontics and Dentofacial Orthopedics, Kalka Dental College and Hospital, Meerut, Uttar Pradesh, India.
2 Reader, Department of Orthodontics and Dentofacial Orthopedics, Kalka Dental College and Hospital, Meerut, Uttar Pradesh, India.
3 Professor and Head, Department of Orthodontics, ITS Dental College Hospital and Research Center, Greater Noida, Uttar Pradesh, India.
4 Senior Lecturer, Department of Orthodontics and Dentofacial Orthopedics, Kalka Dental College and Hospital, Meerut, Uttar Pradesh, India.
5 Professor, Department of Orthodontics and Dentofacial Orthopedics, Kalka Dental College and Hospital, Meerut, Uttar Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sushil Kumar, Professor and Head, Department of Orthodontics and Dentofacial Orthopedics Kalka Dental College and Hospital, Partapur Bypass Road, Meerut, Uttar Pradesh, India.
E-mail: docshilu@yahoo.com
Growth, Interceptive, Overbite
Case-1
An 11 year old male reported to the Department of Orthodontics, with the chief complaint of irregularity in the upper front teeth and difficulty in chewing. Clinical examination revealed maxilla was hypoplastic in all three dimensions - resulting in crowding, anterior crossbite and overclosure of mandible [Table/Fig-1a]. In order to address these composite issues, it was decided to proceed with rapid maxillary expansion and face mask therapy with Delaire face mask [Table/Fig-1b,1c] followed by fixed mechanotherapy. Impressive results were obtained after completion of treatment [Table/Fig-1d].
a.Pre treatment frontal view.
b. Delaire face mask in place
c. After maxillary expansion and face mask therapy
d. Post treatment frontal view
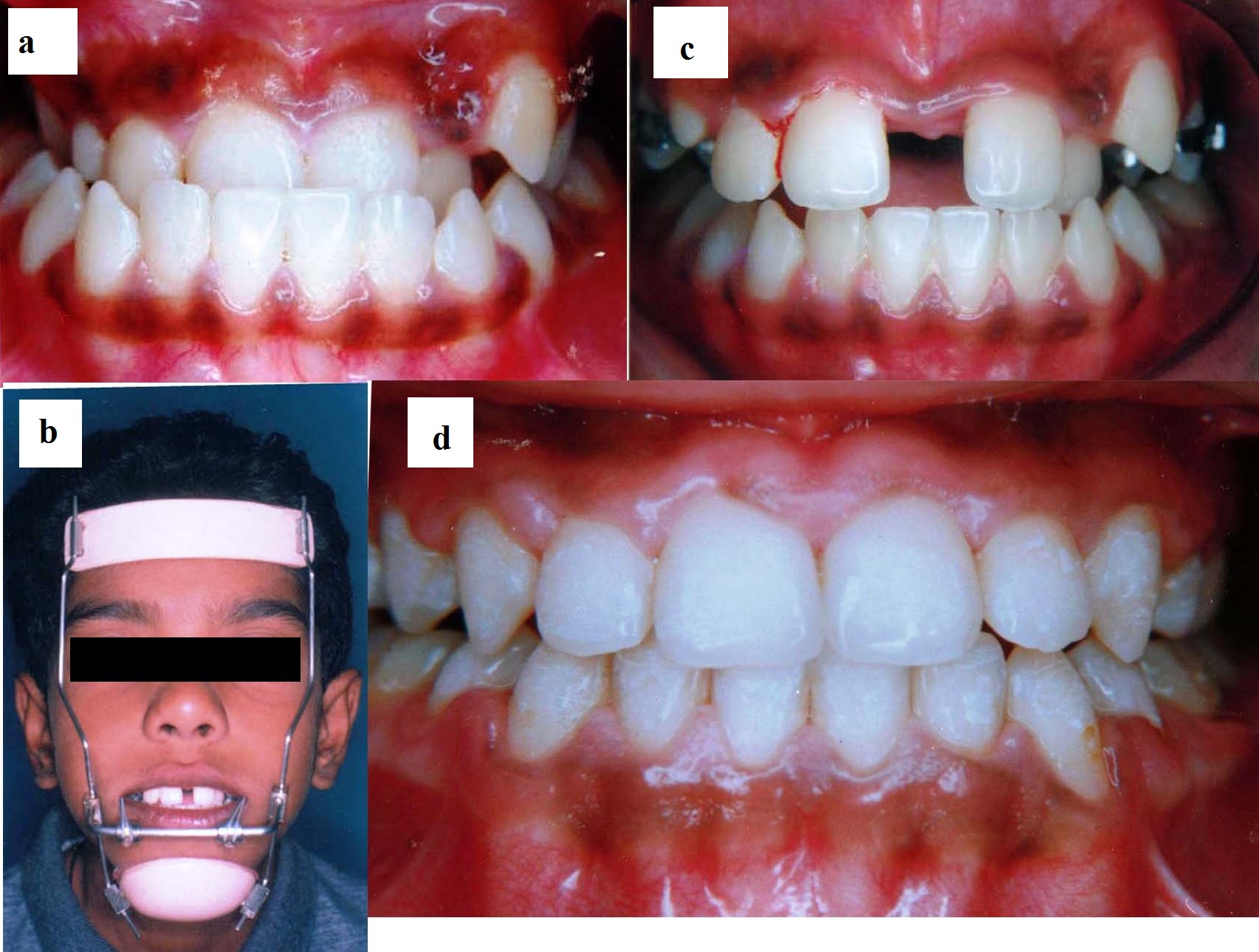
Clinical significance: Although post treatment stability and long term prognosis of facemask therapy is doubtful due to dubious nature of mandibular growth in Class III patients, early treatment does provide a favourable environment for future growth [1], prevents damage to oral tissues along with improving occlusion and facial aesthetics. All these boost the psychosocial development of the children.
Case-2
A 19 year old female patient reported to the Department of Orthodontics, with chief complaint of irregular front upper teeth and poor smile aesthetics. Clinical examination unveiled the presence of cross bite of both upper canines, deep bite and crowded lower dentition [Table/Fig-2a,2b]. We decided to treat her with fixed orthodontic appliance with pre-adjusted MBT prescription (022 slot). Following initial alignment and levelling, a base arch and piggyback archwire assembly consisting of 018" x 025" SS and 014 NiTi were installed to uncross the bite which was kept open with fixed posterior acrylic bite block [Table/Fig-2c,2d]. Smile aesthetics got greatly enhanced with desired canine prominence [Table/Fig-2e,2f].
a.Pre treatment frontal view
b. Pre treatment right buccal view
c.018x025 SS archwire with 014 NiTi in piggyback mode to uncross bite
d.Fixed posterior bite block to keep bite open
e. Post treatment frontal view
f. Post treatment right buccal view
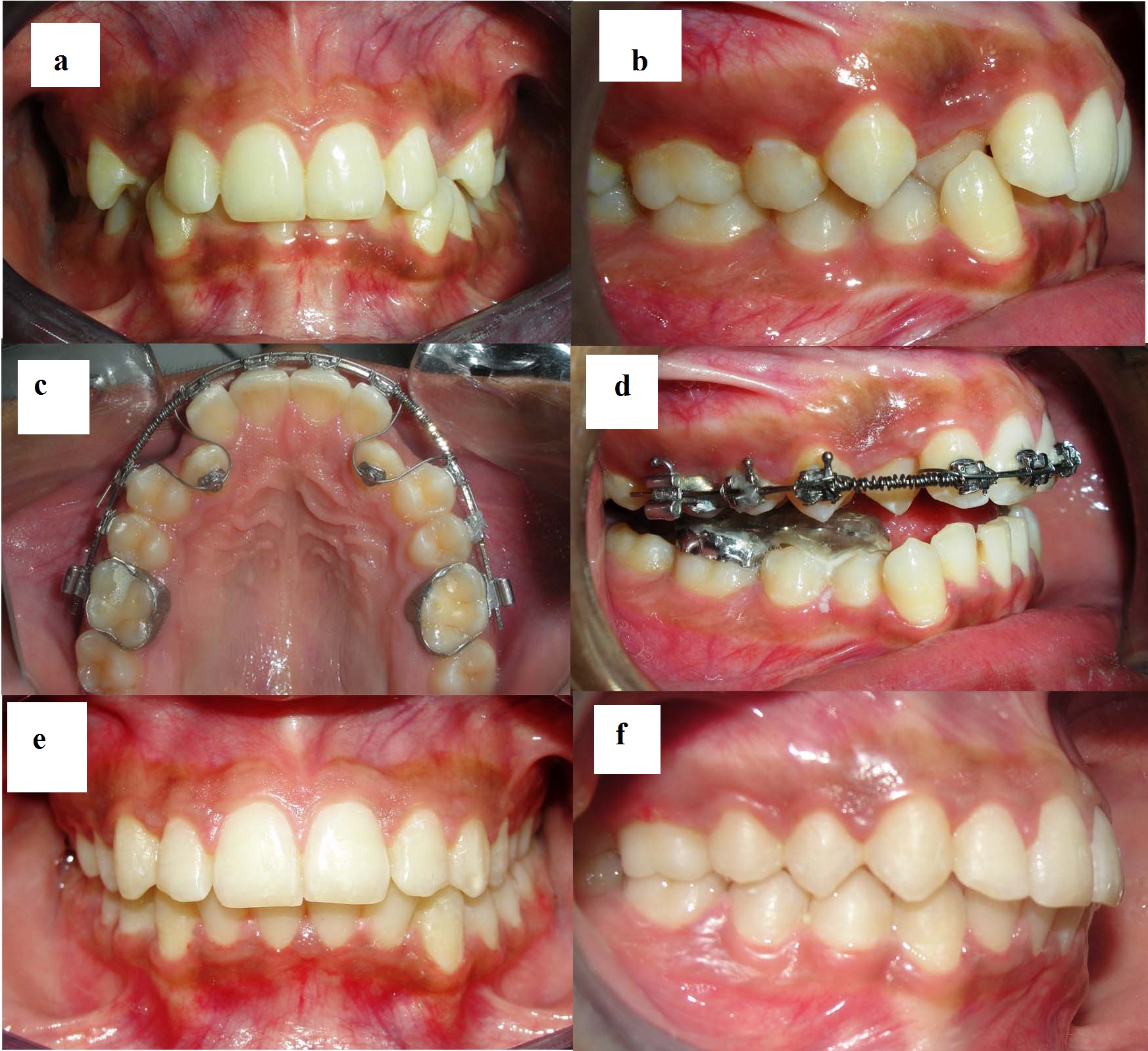
Clinical significance: Considering the age and sex of the patient, growth restriction from this type of crossbite is unlikely in this case, but it may lead to abnormal enamel abrasion, thinning of labial alveolar plate, and/or gingival recession [2]. Lack of desired canine prominence might hamper facial aesthetics too.
Case-3
A 16-year-old female reported to Department of Orthodontics, with buccally positioned upper right canine and irregularly placed upper and lower front teeth [Table/Fig-3a]. The patient had a super-Class I molar relationship with an overjet of 2.5mm, overbite of 3mm. In the functional examination, she could move the mandible back to an edge-to-edge position. Standard edgewise appliance (022 slot) was bonded in upper arch, and an 0.016"× 0.016" Ricketts protrusion arch was placed to procline the upper incisors [Table/Fig-3b]. To temporarily open the bite an interim bite raiser [3] was attached to the occlusal surfaces of mandibular posteriors. After four months of treatment, positive overjet was attained and maxillary crowding was eliminated [Table/Fig-3c]. Satisfactory aesthetics and occlusion were achieved following debonding [Table/Fig-3d].
a. Pre-treatment frontal view, b. Modified protrusion arch for allignment and advancement of incisors. Interim bite raiser in place, c. After correction of crossbite, d. Post treatment frontal view
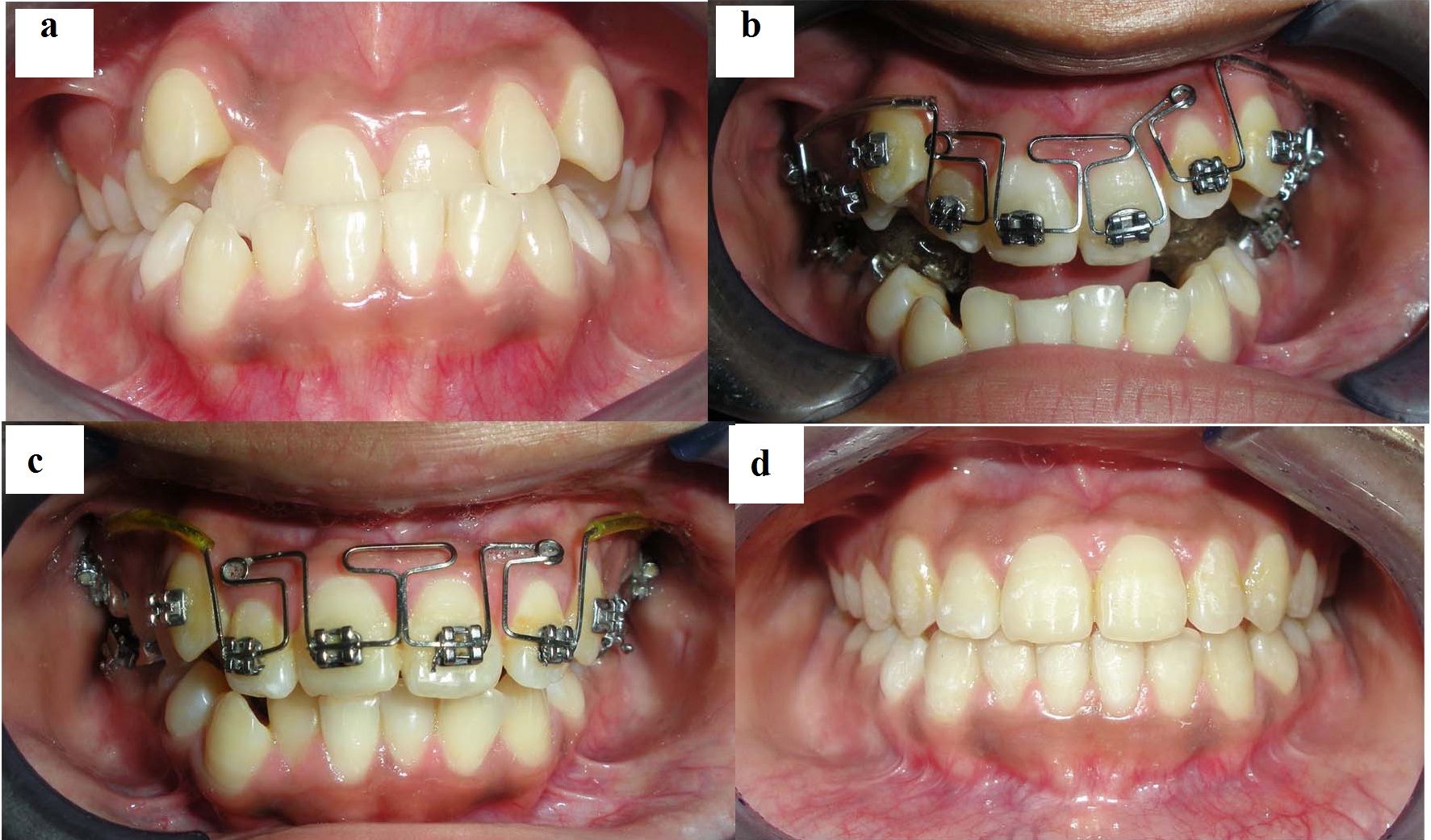
Clinical significance: In this case, adverse growth changes can take place even after growth has been completed. Continuous forward traction of the mandible may stimulate the glenoid fossa to remodel itself [4] and may convert the pseudo Class III to a true skeletal Class III malocclusion, thereby posing more difficulty from therapeutic perspective.
Case-4
A 17 years old female, presented with a Class III incisor relationship on a Class III skeletal base with an increased maxillary-mandibular planes angle and face height ratio. Maxillary canines were impacted [Table/Fig-4a,4b]. Increased skeletal component in both sagittal and vertical dimension demands ortho-surgical correction in order to level and align, close upper anterior space (after extraction of impacted upper canines), co-ordinate arches and to correct skeletal relationship. Following decompensation [Table/Fig-4c,4d], mandibular set back was performed with Bilateral Sagittal Split Osteotomy (BSSO). The basic osteotomy pattern included cuts just through the cortical bone: on the medial side of ramus above the lingula, down the anterior ramus onto the superior aspect of the body of mandible, and then curving inferiorly through the lateral cortical plate, including the lower border [Table/Fig-4e]. The bony segments were separated bilaterally and distal segment was repositioned. The lower teeth were secured to maxilla with maxillo-mandibular fixation and with the aid of occlusal wafer splint. To establish an appropriate condylar position, proximal condylar segment were gently positioned and stabilized with ramus pusher. Interosseous fixation of segments was done with bone plates [Table/Fig-4f]. After a brief period of occlusal settling final result was achieved with good overbite and inter digitations ensuring favourable prognosis [Table/Fig-4g,4h].
a.Pre treatment frontal view, b. Pre treatment close-up lateral view c. Pre surgical frontal view, d. Pre surgical close-up lateral view, e.Intra-operative right buccal view after mandibular sagittal split, f.Intra-operative right buccal view after rigid fixation of segments, g. Post treatment frontal view, h. Post treatment right buccal view.
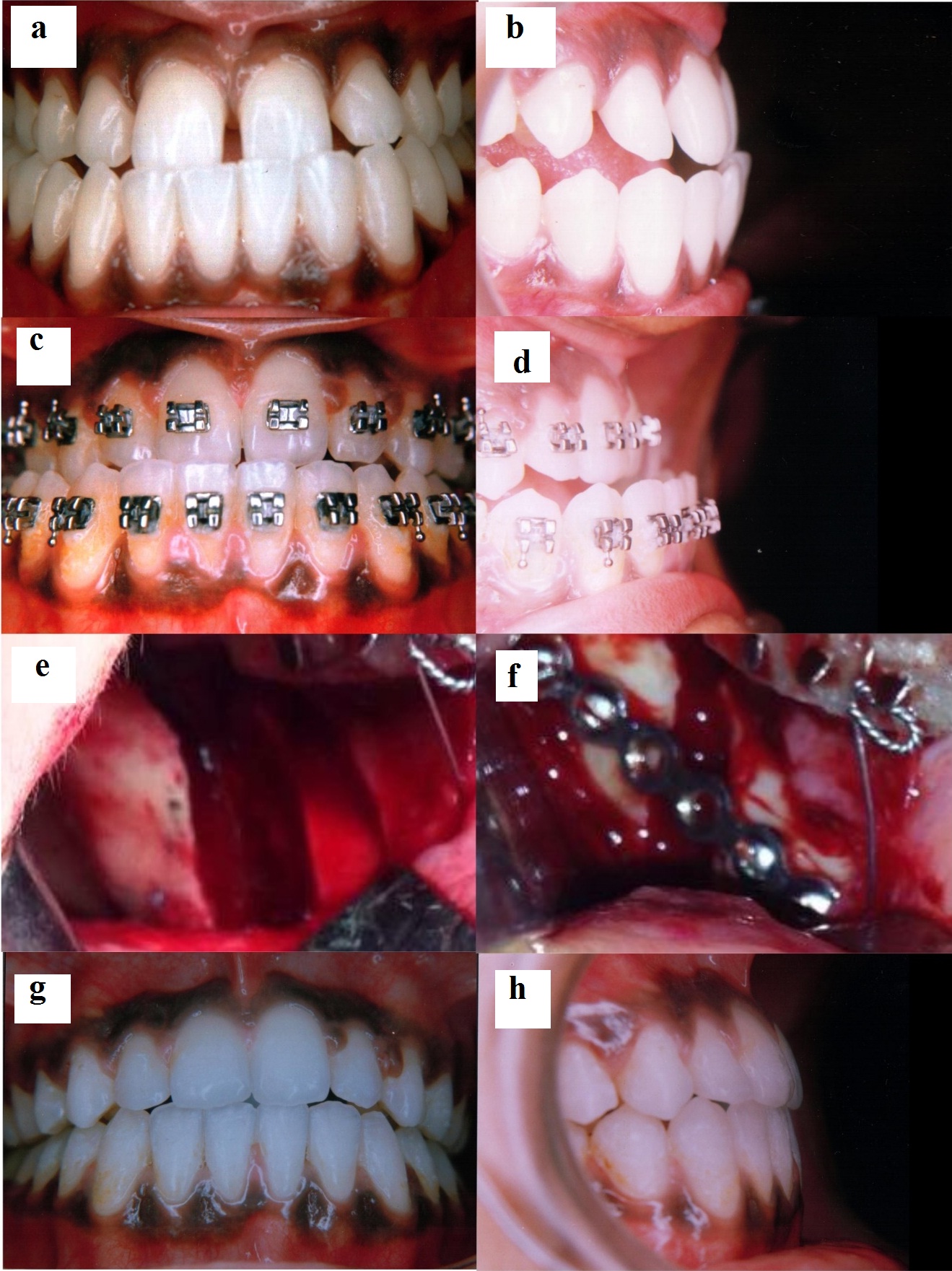
Clinical significance: Considering the skeletal age of the patient and severity of dysplasia in both sagittal and vertical dimensions, placed this patient outside the realms of non-surgical correction in “envelope of discrepancy” [5]. Surgical correction restored aesthetics and function and prevented ongoing damage to the hard and soft tissues of oral cavity.
Crossbite is having major aesthetic and functional implication during the developmental stage of a child because of its self-perpetuating nature. Previous literature reviews [6] advocate early intervention to correct anterior crossbite in the primary or mixed dentition but very few have placed significant weight on the randomised controlled trials of early treatment, moreover strong evidence in support of any one treatment technique is also lacking. Thus, the need for high-quality clinical trials to identify the most effective intervention for correcting anterior crossbites cannot be underestimated [7]. Nonetheless, crossbite is one of the problems that are recommended to be corrected as soon as possible because an uncorrected crossbite can lead to undesirable growth modification thus, resulting in true asymmetry of the face. As growing period provides best opportunity for occlusal guidance and interception of malocclusion, it is important to evaluate post treatment changes in a long-term perspective in the light of prospective study designs.
[1]. Joondeph DR, Early orthodontic treatmentAm J Orthod Dentofacial Orthop 1993 104(2):199-200. [Google Scholar]
[2]. Tse CS, Correction of single-tooth anterior crossbiteJ Clin Orthod 1997 31(3):188 [Google Scholar]
[3]. Roy AS, Singh GK, Tandon P, De N, An interim bite raiserInt J Orthod Milwaukee 2013 24(2):63-64. [Google Scholar]
[4]. Agronin KJ, Kokich VG, Displacement of the glenoid fossa: a cephalometric evaluation of growth during treatmentAm J Orthod Dentofacial Orthop 1987 91(1):42-48. [Google Scholar]
[5]. Ackerman JL, Nguyen T, Proffit WR, The decision – making process in orthodontics. In: Graber LW, Vanarasdall RL, Wig KWL.(eds.)Orthodontics current principles and techniques 2012 ed 5PhiladelphiaMosby:16-8. [Google Scholar]
[6]. Borrie F, Bearn D, Early correction of anterior crossbites: a systematic reviewJ Orthod 2011 38:175-84. [Google Scholar]
[7]. Wiedel AP, Bondemark L, Stability of anterior crossbite correction: a randomized controlled trial with a 2-year follow-upAngle Orthod 2015 85(2):189-95. [Google Scholar]