Calcifying Epithelial Odontogenic Tumour of the Mandible: An Unusually Aggressive Presentation of an Indolent Tumour
DP Arul Dev1, Manjusha Pattamparambath2, Manoj Joseph Michael3, AV Akhilesh4, Bindu Das5
1 Junior Resident, Department of Oral and Maxillofacial Surgery, Government Dental College, Calicut, Kerala, India.
2 Senior Resident, Department of Oral Pathology and Microbiology, Government Dental College, Calicut, Kerala, India.
3 Associate Professor, Department of Oral and Maxillofacial Surgery, Government Dental College, Calicut, Kerala, India.
4 Assistant Professor, Department of Oral and Maxillofacial Surgery, Government Dental College, Calicut, Kerala, India.
5 Assistant Professor, Department of Oral and Maxillofacial Surgery, Government Dental College, Calicut, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Manjusha Pattamparambath, 1/1097-A, Sukrutham, P O Westhill, Calicut- 673005, Kerala, India.
E-mail: manjumdvn@gmail.com
Calcifying Epithelial Odontogenic Tumour (CEOT) or Pindborg tumour is a rare odontogenic tumour of epithelial origin. They constitute less than 1% of odontogenic tumours. Intra-ossseous variant of CEOT are more common compared to extra-osseous variant. Although benign, these can exhibit deceptively aggressive presentation. Here we report a rare case of CEOT in a 36-year-old female patient who presented with aggressive intra-osseous lesion with cortical breach and exuberant soft tissue proliferation. The lesion was treated with resection and reconstructed with titanium reconstruction plate.
Intraosseous, Pindborg tumour, Swelling
Case Report
A 36-year-old female patient reported to the Department of Oral & Maxillofacial Surgery with the complaint of a rapidly growing mass over the right lower gums. The patient noticed the growth two years back. It was small and asymptomatic to start with, however in the last six months the lesion had rapidly increased in size causing difficulty in mastication, speech and in maintaining oral hygiene. Although the lesion was painless, it was fragile and bled while brushing and having food. There was no associated paresthesia.
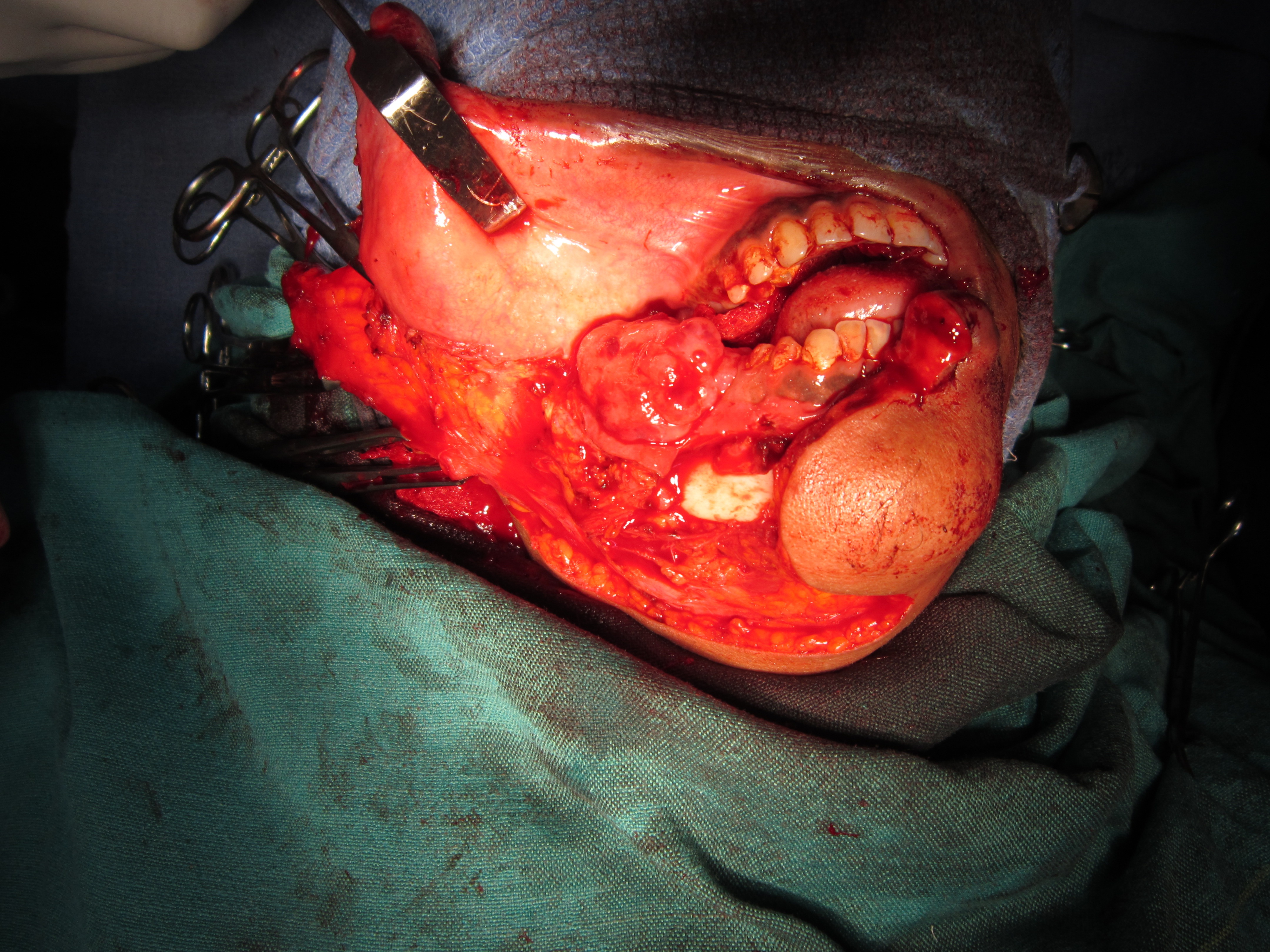
Extra orally the face was asymmetric with a diffuse swelling over the right side of the face [Table/Fig-1]. Patient appeared pale and anaemic. On opening the mouth, mandible deviated slightly to the right. Clicking of right temperomandibular joint was also noted. Intra oral examination revealed a large pedunculated soft tissue mass of about 6cmx4cmx3cm on the right side of mandible. It originated from the retromolar region and extended to the distal aspect of right first premolar anteriorly. Buccally, the lesion obliterated the mucobuccal sulcus superoinferiorly and extended over occlusal table to the lingual aspect of posterior teeth. Lesion had displaced the first and second molars lingually. Third molar was clinically missing. Surface of the lesion was erythaematous and covered by a whitish slough. There were indentations of the upper teeth over the lesion [Table/Fig-2]. On palpation the lesion was slightly tender and fragile.
Extraoral view of the patient showing diffuse swelling on the right side of the face.

Intraoral view of the lesion. Exuberant soft tissue growth with lingual displacement of the molars.

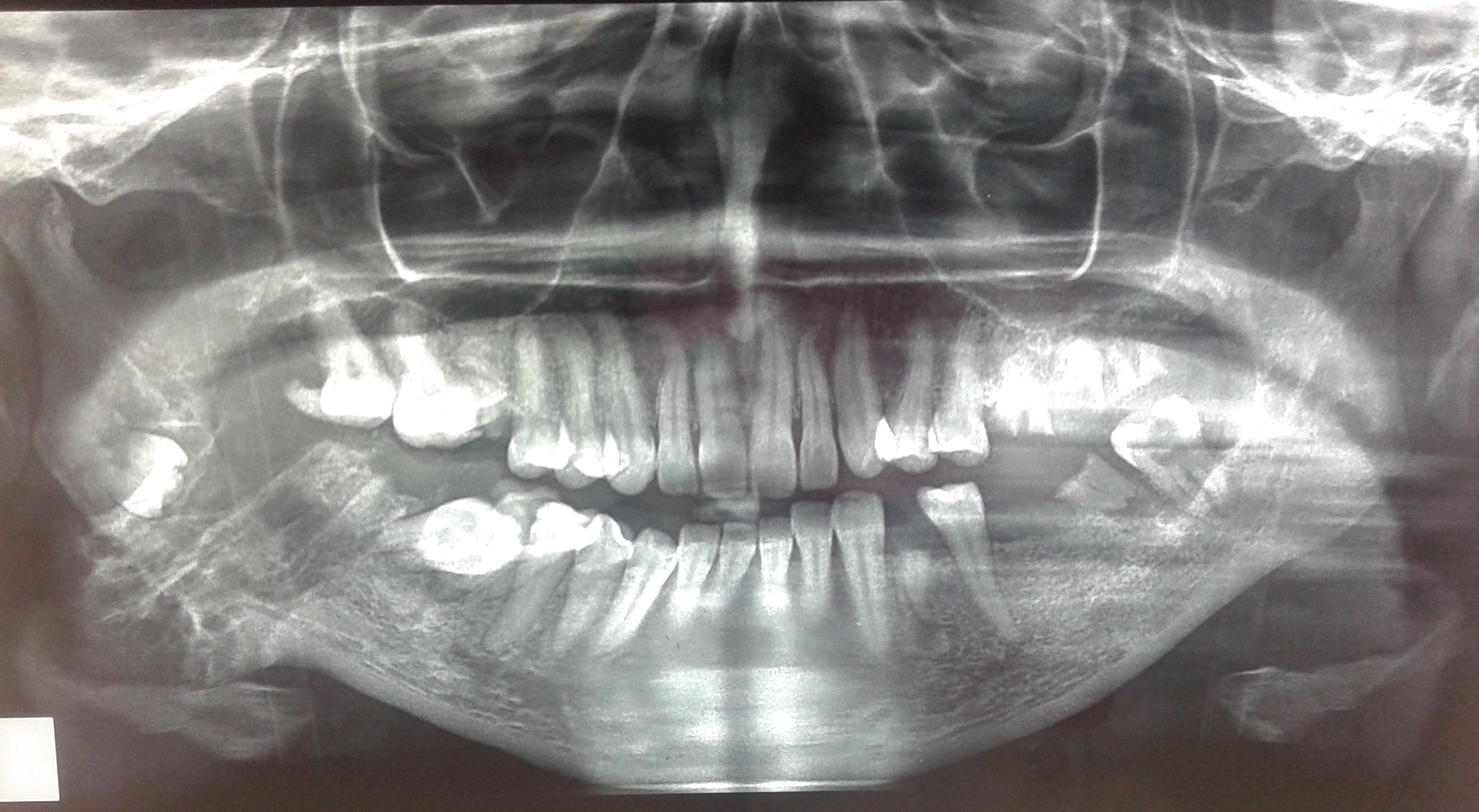
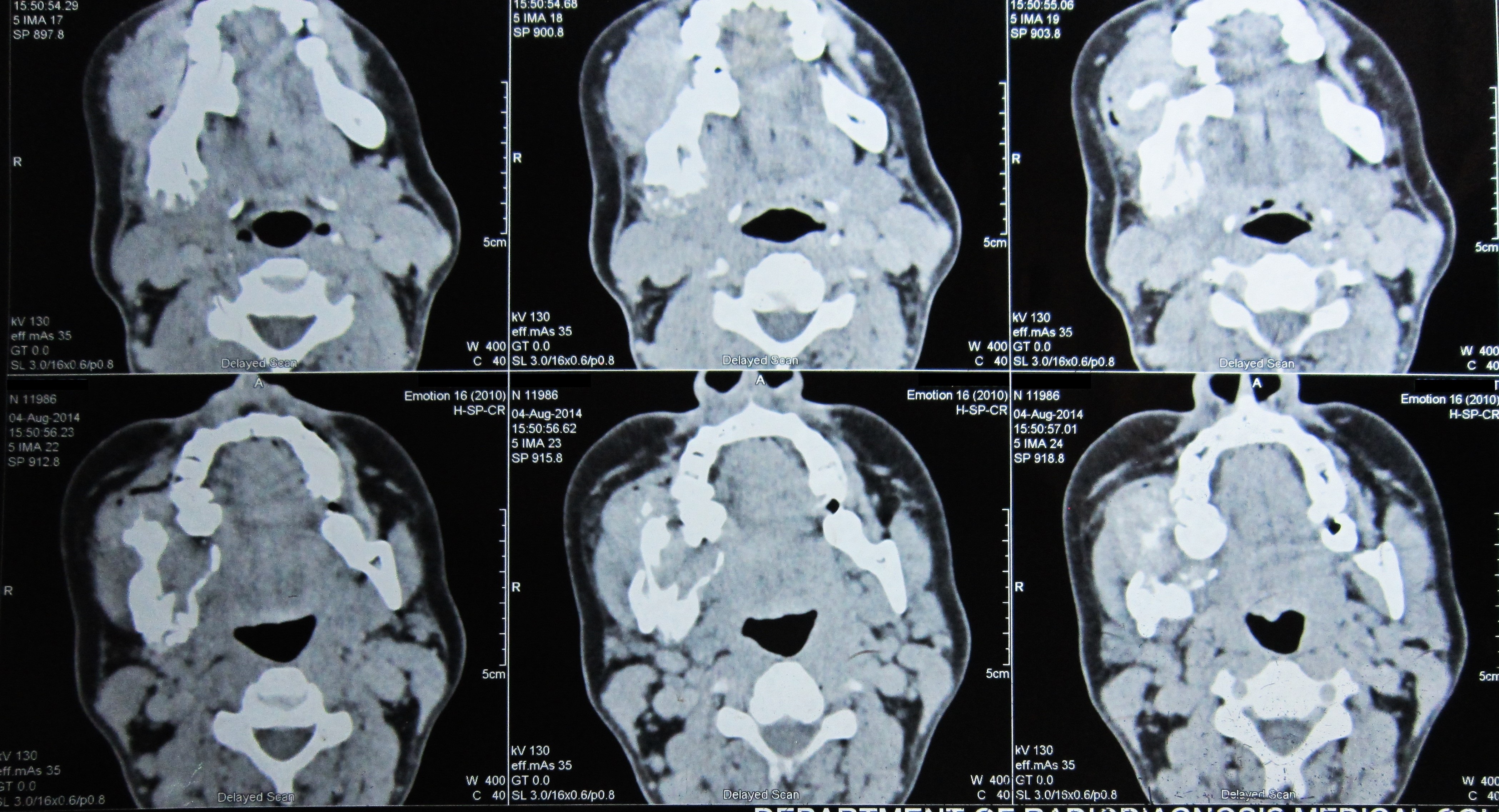
Radiographic examinations were performed. Panoramic radiograph showed a radiolucent lesion on the right body of mandible with irregular radioopacity extending below the lower border. The lower border of mandible was irregular and the trabecular pattern was altered. Impacted 48 was seen, displaced towards the angle of the mandible [Table/Fig-3]. Posterior–anterior view showed a mixed radiopaque-radiolucent lesion with impacted third molar being displaced posteriorly and horizontally [Table/Fig-4]. An axial Computed Tomography (CT) revealed an expansile lytic lesion with exophytic component and cortical breach with exuberant soft tissue component involving buccal surface of the mandible with involvement of angle of the mandible, adjacent ramus and posterior two thirds of the body [Table/Fig-5]. An ultrasonogram was performed which revealed a hypoechoic lesion with significant soft tissue component and the lesion exhibited increased vascularity. Possibility of a malignant neoplasm was suggested.
Panoramic radiograph showing radiolucent lesion with irregular radioopacities. Impacted third molar is also seen.
PA view showing mixed radio opaque radiolucent lesion.

Coronal CT showing expansile lytic lesion involving ramus, angle and body of the mandible.
Diagnosis and Treatment
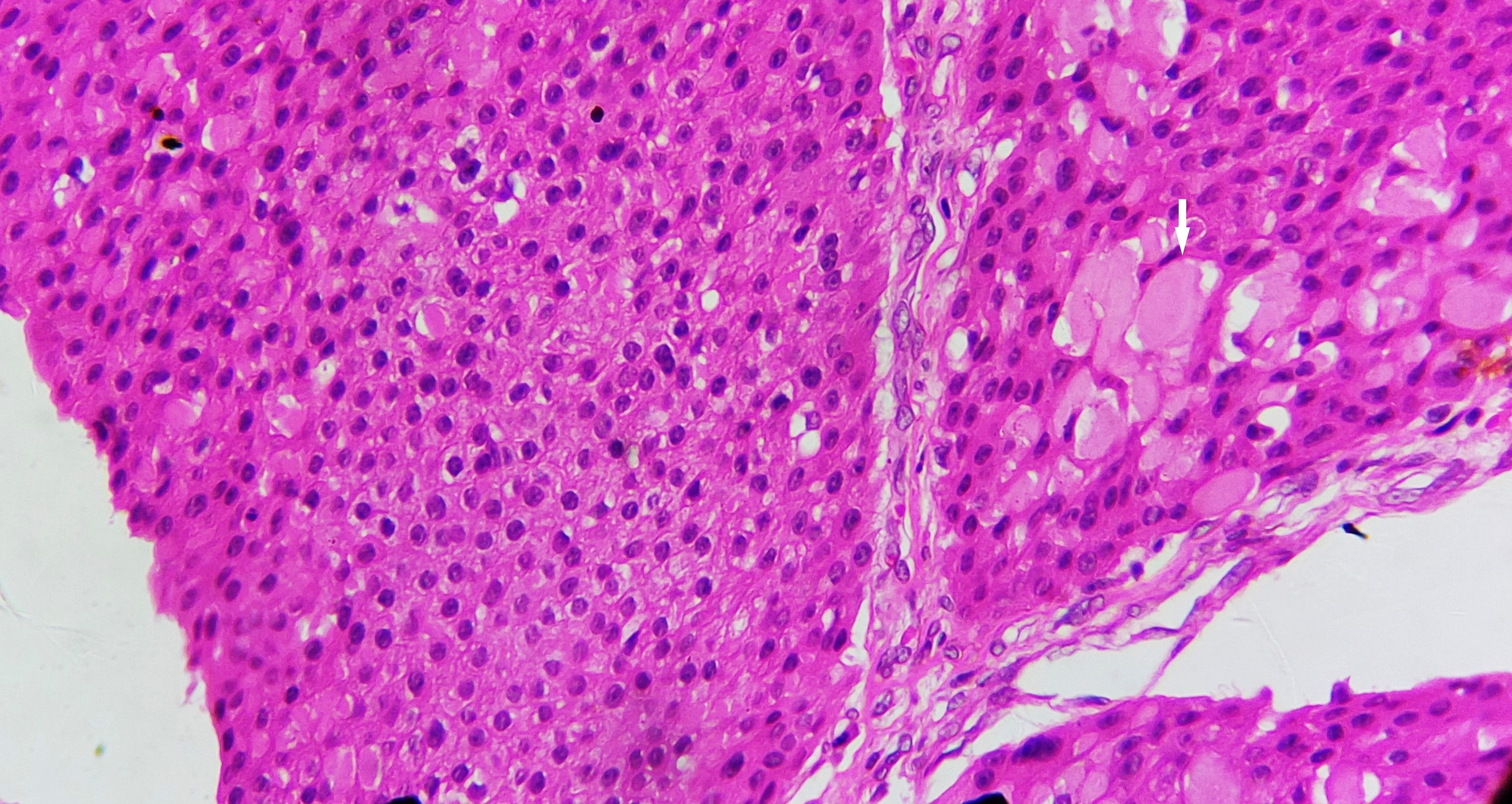
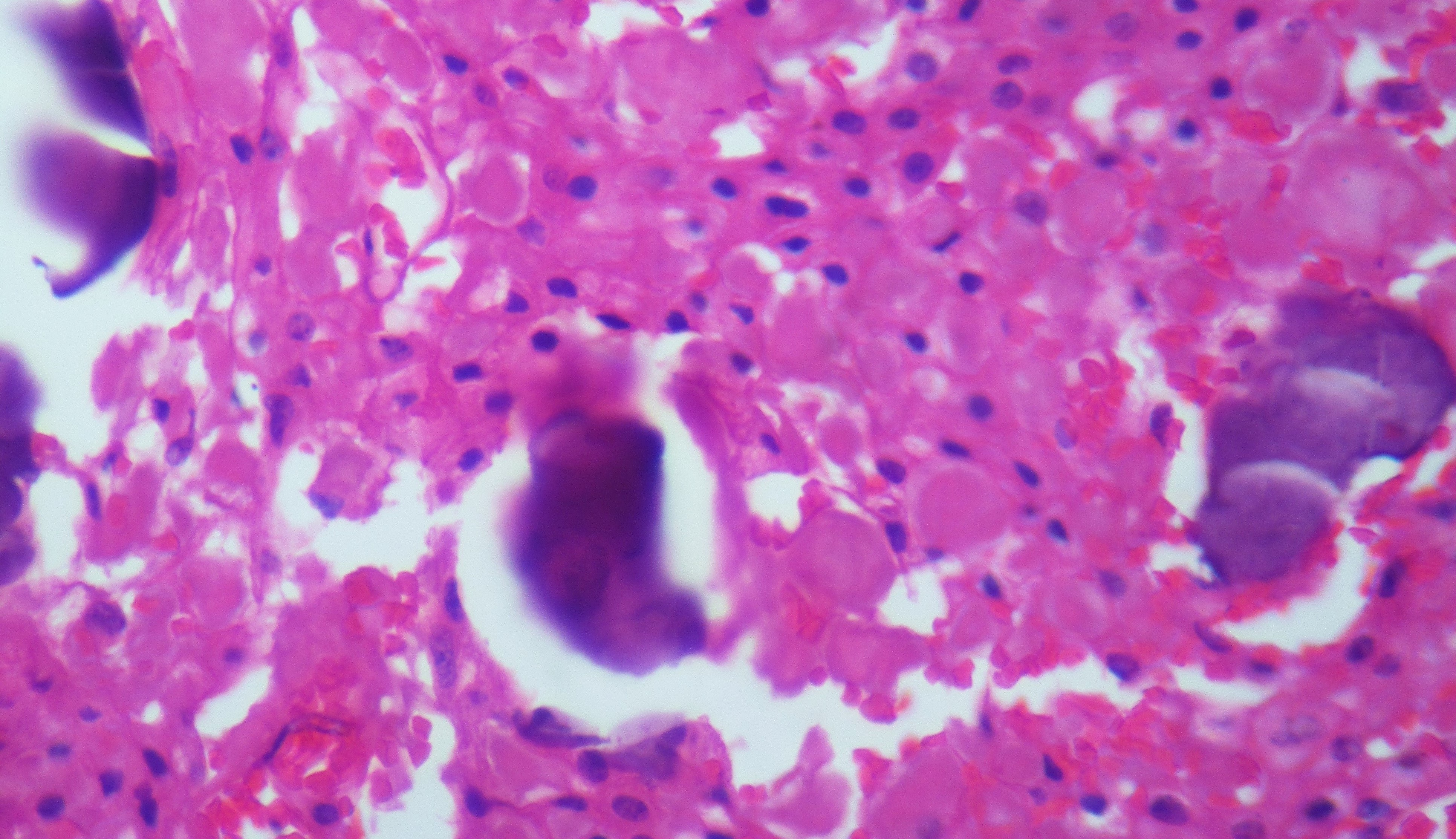
The long duration of the tumour, locally aggressive nature and association with an impacted tooth prompted us to include benign odontogenic tumours like ameloblastoma, odontogenic myxoma and CEOT in the differential diagnosis. Radio-graphic differential diagnosis included osteosarcoma, intraosseous squamous cell carcinoma and metastatic lesion. An incisional biopsy was planned to confirm the diagnosis. Routine blood examination was done which revealed that patient was anaemic with a Hemoglobin (Hb) count of 7.5 gm/dl. Following treatment in the medicine department for the correction of Hb, patient was taken up for incisional biopsy under local anaesthesia. Histopathologic examination revealed sheets and islands of polygonal cells with centrally placed basophilic nucleus, eosinophilic cytoplasm and prominent intercellular bridges [Table/Fig-6]. At areas, sheets of large polygonal cells with abundant eosinophilic material and eccentrically placed nucleus were seen. Extracellularly, areas of homogenous eosinophilic material resembling amyloid were present. Within a few tumour islands basophilic flecks of calcified masses could be noted [Table/Fig-7]. To confirm the nature of eosinophilic material Congo red staining was done. The Congo red stained section was examined under polarised microscope which revealed areas of apple green birefringence which confirmed the presence of amyloid. Thus, a final diagnosis of CEOT was made.
Sheets of cells with polygonal shape and prominent intercellular junctions (H&E; 40X). Arrow shows sheets of cells with extracellular eosinophilic material.
Basophilic flecks of calcification seen within tumour islands (H&E; 40X).
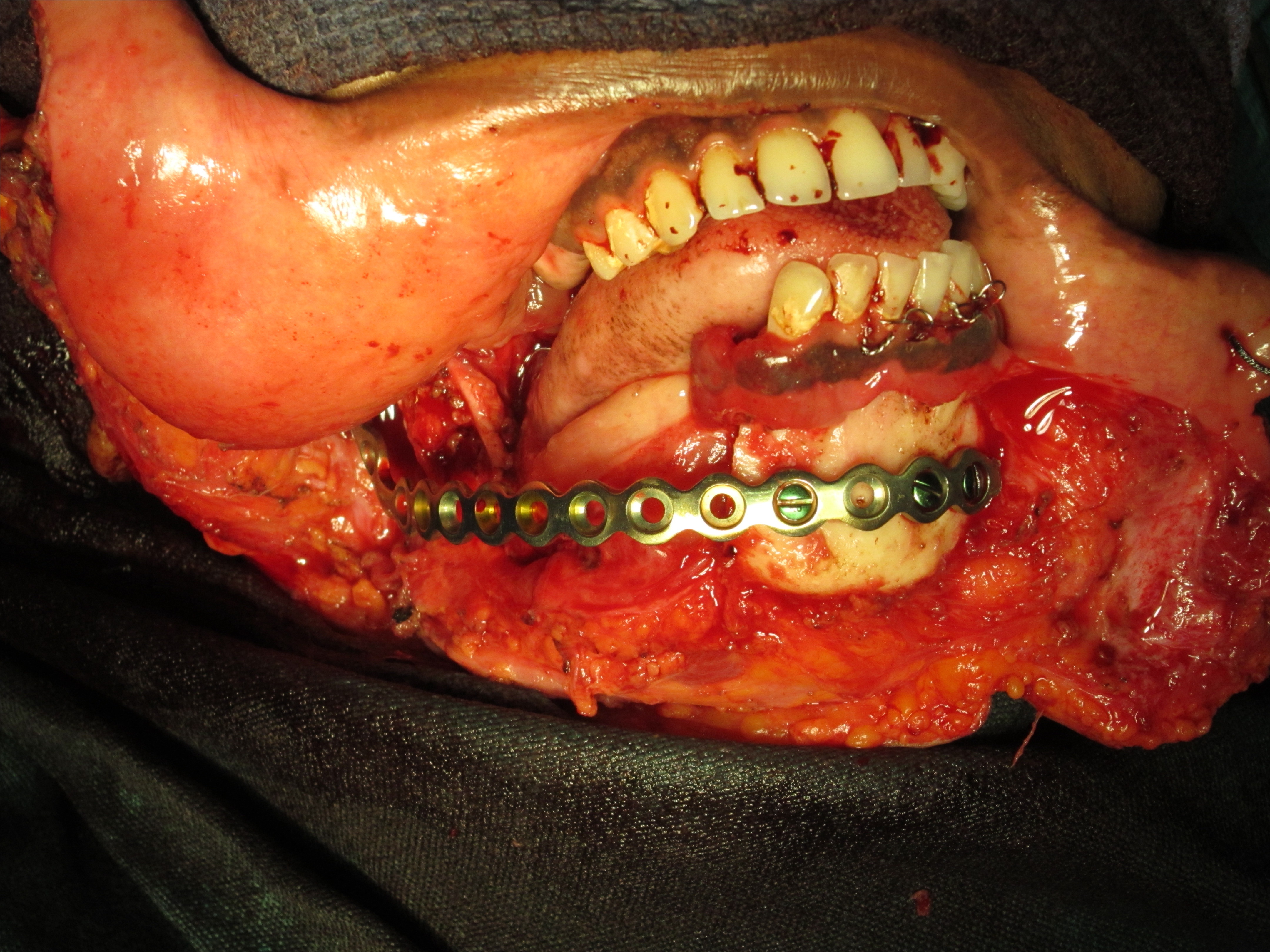
Owing to the increased vascularity of the lesion as observed in Ultrasonogram (USG) and the decreased Hb content in the patient, it was planned to undertake sclerotherapy prior to surgical excision. A 2ml of sodium tetradecyl sulphate, a sclerosing solution was injected weekly over a period of six weeks. There was considerable shrinking of the lesion due to decreased vascularity and increased fibrosis. Following this, surgery was planned under general anaesthesia with a minimum of 1.5cm margin and reconstruction using reconstruction plate. Extended right side submandibular incision was placed with midline lip split access preserving mentalis muscle. Tumour had reached in bone and resection was carried out distal to canine extending upto the subcondylar region, preserving the condyle and the coronoid [Table/Fig-8]. A 2.7mm titanium reconstruction plate was adapted and fixed using two screws in the distal and four screws in proximal region, after achieving occlusion by maxillo-mandibular fixation [Table/Fig-9,10]. Post-operative healing was uneventful and the excised tissue [Table/Fig-11] was further histopathologically diagnosed as CEOT with free margins. The patient was being followed up regularly and there was no evidence of recurrence two years post surgery [Table/Fig-12,13].
Intra-operative view with the tumour exposed.
Intra-operative view with titanium reconstruction plate fixed. Arrow show sheets of cells with extracellular eosinophilic material.
Post-operative view with sutures placed.

The resected mandible with the tumour..

Post-operative view of patient 6 months following surgery.

Post-operative OPG of the patient showing the reconstructive plate in place.

Discussion
CEOT or Pindborg tumour is a rare and benign tumour of odontogenic epithelial origin and accounts for less than 1% of odontogenic tumours [1]. It was first described by Pindborg in 1955. These tumours are most prevalent among the 30 to 50 year age group, with no pre-ference for either sex. The spectrum of CEOT consists of intra-osseous or central CEOT and extra-osseous or peripheral CEOT with an incidence of 94% and 6%, respectively [2]. The commonest site for an intra-osseous tumour is posterior mandible whereas extra-osseous tumours have been described more in the anterior gingiva. Different clinical presentations of the tumour have distinguished histogenetic origins. The central tumours are said to be derived from the stratum intermedium of the enamel organ whereas the extraosseous form arises from dental lamina epithelial rests in gingival and/or basal cells of the gingival surface epithelium [3].
CEOT being a benign lesion, the typical clinical presentation is an asymptomatic slowly enlarging mass of the affected jaw. However, it exhibits a variable biologic behaviour ranging from very mild to moderate invasiveness. The tumour is known to grow by infiltration and producing cortical expansion, tooth movement, and root resorption [1]. Our case was an intra-osseous tumour in the posterior mandible with an unusually aggressive nature which exhibited cortical perforation with resultant exuberant soft tissue component. Impacted right third molar was displaced to the angle of the mandible. First and second molars were lingually displaced. Such an aggressive presentation is rare in CEOT. On literature search we came across a case similar to ours which was reported as intra-osseous and peripheral tumour arising in the same site [4]. However, we consider our case as an intra osseous tumour with increased invasiveness as peripheral CEOTs are typically smaller than 2 cm and they grow from the gum or from the edentulous alveolar mucosa, generally in the anterior region. They are painless and firm, without osseous invasiveness. Its behaviour is less aggressive clinically than the central one [5].
The radiographic appearance of CEOT may vary depending on the stage of development. It may be a well defined radiolucency, mixed radiolucent radiopaque or completely radiopaque mass. The lesion often presents as mixed radiolucent radiopaque with many small irregular trabeculae passing through the radiolucent area. It has been described as “driven snow” appearance due to scattered flecks of calcification [2]. The margins are usually well defined or sclerotic. In the current case the margins were ill defined. As in our case, the tumour may be associated with an impacted tooth. In CT, CEOT usually appears as an expansile unilocular or multilocular lesion containing radioopaque masses within the lesion.
Histopathologically tumour consists of polyhedral cells proliferating in masses, sheets and islands in a scanty connective tissue stroma. The cells exhibit prominent intercellular junctions, abundant cytoplasm nuclear pleomorphism, anisonucleosis and hyperchromatism. Extracellular and intracellular deposit of eosinophilic “amyloid like” material, which gradually becomes concentric calcified deposits, called the “Liesegang rings,” is considered as pathognomonic for this tumour [6]. The eosinophilic amyloid material stains positive for Congo red and will appear as an applegreen birefringence under a polarized microscope. All these features were present in the current case.
CEOT being a tumour with varied presentation, some surgeons have advocated conservative surgery, whereas others have suggested radical treatment. Small intrabony lesions may be treated with conservative tumour enucleation and curettage followed by removal of a thin layer of normal bone adjacent to the tumour. Larger lesions may require resection of the tumour into the disease-free bony margin as these tumours are more invasive and destructive [7]. The lesions treated with enucleation and curettage procedures show a high recurrence rate ranging from 15% to 30% after just 2-4 years [2]. Therefore, CEOT is best treated with a resection using 1.0cm-1.5cm margins in bone. In the current case resection was performed with 1.5cm tumour free margins. Malignant transformation of CEOT is extremely rare and very few cases have been reported [8].
The highly vascular nature of the lesion as evidenced by USG prompted the use of sclerotherapy in the current case prior to resection. Sclerotherapy is a conventional method well accepted in the treatment of vascular lesions. It is known to decrease the size and vascularity of the lesion and changes its nature to more fibrous consistency; thence, resection is accomplished with minimal blood loss [9].
Conclusion
Although a benign tumour, CEOT can have deceptively aggressive presentation. Cortical breach and subsequent soft tissue involvement as seen in the current case is an extremely rare feature. The aggressive nature of the lesion warrants a more radical approach of treatment. The present case highlights the highly aggressive and locally destructive capability of benign odontogenic tumours and the need for clinicians to be aware of such a possibility.
[1]. More CB, Vijayvargiya R, Intraosseous calcifying epithelial odontogenic (Pindborg) tumour: A rare entityJ Oral Maxillofac Pathol 2015 19:269 [Google Scholar]
[2]. Sahni P, Nayak M, Singhvi A, Sharma J, Clear cell calcifying epithelial odontogenic (Pindborg) tumour involving the maxillary sinus: A case report and review of literatureJ Oral Maxillofac Pathol 2012 16:454-59. [Google Scholar]
[3]. Hicks MJ, Flaitz CM, Wong ME, McDaniel RK, Cagle PT, Clear cell variant of calcifying epithelial odontogenic tumour: case report and review of the literatureHead Neck 1994 16:272 [Google Scholar]
[4]. Vinayakrishna K, Soumithran C, Sobhana C, Biradar V, Peripheral and central aggressive form of Pindborg tumour of mandible – A rare case reportJ Oral Biol Craniofac Res 2013 3(3):154-58. [Google Scholar]
[5]. Goode R, Calcifying epithelial odontogenic tumourOral Maxillofac Surg Clin North Am 2004 16(3):323-31. [Google Scholar]
[6]. Sedghizadeh P, Wong D, Shuler C, Linz V, Kalmar J, Allen C, Multifocal calcifying epithelial odontogenic tumourOral Med Oral Pathol Oral Radiol Endod 2007 104(2):e30-e34. [Google Scholar]
[7]. Lin J, Bianchi M, Popnikolov N, Abaza N, Calcifying epithelial odontogenic tumour: case report with immunohistochemical and ultrastructural study and review of the literatureJ Oral Maxillofac Surg 2013 71(2):278-89. [Google Scholar]
[8]. Demian N, Harris R, Abramovitch K, Wilson J, Vigneswaran N, Malignant transformation of calcifying epithelial odontogenic tumour is associated with the loss of p53 transcriptional activity: a case report with review of the literatureJournal of Oral and Maxillofacial Surgery 2010 68(8):1964-73. [Google Scholar]
[9]. Selim H, Selim A, Khachemoune A, Metwally SA, Use of sclerosing agent in the management of oral and perioral haemangiomas: Review and case reportsMed Sci Monit 2007 13(9):CS114-19. [Google Scholar]