Acute Right Heart Failure in a Patient with Right Heart Thrombus and Pulmonary Thromboembolism
Mohammad Mostafa Ansari-Ramandi1, Samaneh Ansari-Ramandi2, Nasim Naderi3
1 Cardiology Resident, Department of Cardiology, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran.
2 Tehran Shahresalem Co, Tehran, Iran.
3 Associate Professor, Department of Cardiology, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nasim Naderi, Rajaie Cardiovascular Medical and Research Center, Iran University of Medical Sciences, Tehran, Iran.
E-mail: dr.mm.ansari@gmail.com
Right Heart Thrombus (RiHT) management is really controversial, and appropriate guidelines are not present for the management. In patients referring with RiHT and Pulmonary Embolism (PE), there are three ways of managing these patients. Out of the three, one is thrombectomy, which is with high risk taking in mind the comorbidities these patients have. The other is using thrombolytic which, in many cases is contraindicated or with high risk. The other less effective way is full anticoagulation. It is really controversial to choose between these ways of management and no clear approach is present. The case presented is a 44-year-old morbid obese male with history of dyspnea on exertion (functional Class II) and foot oedema or the last three months, who was transferred to the emergency department with respiratory distress and hypoxia. Echocardiography was done for the patient which showed moderate Right Ventricular (RV) dysfunction with severe RV enlargement and a severe Tricuspid Regurgitation (TR) with TR gradient of 70mmHg. He also had a semi-mobile large pedunculated mass in favour of a clot in his RV cavity. With the impression of PE heparin was administered to the patient and he was admitted in the coronary care unit. Pulmonary Computed Tomography (CT) angiography showed sub-segmental Pulmonary Thromboendarterectomy (PTE) in the left lung. He had negative cardiac markers and stable vital signs and so full anticoagulation was chosen for his treatment. His clinical course was uneventful and after 10 days of treatment the RV size and function improved significantly. On follow-up after a month he was doing well. Although recent Guidelines of European Society of Cardiology in management of acute PE stated that RiHT, particularly mobile, are associated with a significantly increased early mortality risk in patients with acute PE. Immediate therapy is mandatory, but optimal treatment is controversial in the absence of controlled trials. Thrombolysis and embolectomy are probably both effective while anticoagulation alone seems to be less effective.
Anticoagulation, Management, Pulmonary embolism
Case Report
A 44-year-old morbidly obese male with history of dyspnea on exertion of functional New York Heart Association (NYHA) functional Class II and foot oedema since three months presents to the emergency department with respiratory distress and hypoxia (an O2 saturation of 80% at room air).
On arrival he had a Blood Pressure (BP) of 140/85mmHg, Heart Rate (HR) of 98 beats per minute and a respiratory rate of 24 per minute. He had no fever. The O2 saturation increased to 92% after administeeing nasal oxygen and his respiratory distress was improved. He had un-remarkable findings in his heart and lung exam except for tachycardia and a grade of 2/6 systolic murmur at left sternal border. The patient was found to have a prominent abdomen with increased liver span and 3+ bilateral pitting oedema of lower extremities.
Transthoracic Echocardiography showed a preserved left ventricular function (left ventricular ejection fraction = 50%) with a severely enlarged RV with moderate systolic dysfunction. The tricuspid valve was severely regurgitant with a Tricuspid Regurgitant Gradient (TRG) of 70mmHg.
A semi-mobile large (3.6cm X 2.2cm) pedunculated mass in favour of thrombus was obvious in his RV cavity attached to the lateral papillary muscle adjacent to the tricuspid valve leaflet. The main pulmonary artery and its branches seemed dilated without any evidence of thrombus.
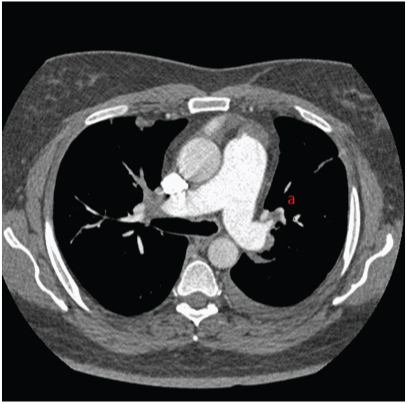
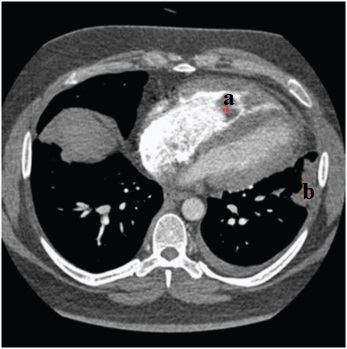
He was transferred to the Coronary Care Unit (CCU) with an impression of acute PTE and intra venous heparin was started. Pulmonary CT angiography showed a sub-segmental PE in the left lung and RiHT and color doppler sonography of the lower limb veins was compatible with acute Deep Vein Thrombosis (DVT) of left popliteal veins [Table/Fig-1,2]. The laboratory tests in terms of complete blood count and renal function tests were within normal limits and the troponin was negative.
Mediastinal view of the pulmonary CT angiography showing segmental PE in the left lung (a)
Mediastinal view of the pulmonary CT angiography showing (a), right heart thrombus and (b), pulmonary infarct
Considering stable vital sign and an estimation of intermediate-low risk for his acute PTE, he was candidate for anticoagulant therapy. His clinical course was uneventful and after 10 days of treatment with heparin and warfarin the RV size and function improved significantly, TRG reduced to 40 mmHg and the RV thrombus was decreased in size (1cm X 2cm) and appeared immobile and fixed in the lateral papillary muscle. On follow-up after a month he was doing well.
Discussion
Right heart thrombus (RiHT) is present in 3%-4% of patients with PTE and its management is controversial and appropriate guidelines for the management of the same are lacking [1]. In patients with RiHT there is high incidence of PE [2–4].
Two types of RiHT have been defined. The type A thrombi have high mobility and are associated with DVT. Type B thrombi are small and immobile associated with right sided heart abnormalities. PE and mortality is more in type A thrombi as compared to type B thrombi [5].
Patients having PE with RiHT have shorter duration of symptoms, lower blood pressure, higher pulse rate, more frequency of congestive heart failure and right ventricular wall hypokinesia and poor prognosis [3].
Although, there are several different modalities for the treatment of RiHT which include anticoagulation with heparin, thrombolysis, catheter embolectomy, and surgical embolectomy, but there is no clear guideline for their use [6].
Out of the four, one is surgical thrombectomy which accompanies significant risk, considering the comorbidities these patients may have. The other is using thrombolytic which in many cases may be contraindicated. The other less effective way is full dose anticoagulation therapy. It is really controversial to choose between these [7].
Recent guidelines of European Society of Cardiology in management of acute PE stated that RiHT, particularly mobile, are associated with a significantly increased early mortality risk in patients with acute PTE but in our case the patient had good outcome by anticoagulation therapy. Immediate therapy is mandatory, but optimal treatment is controversial in the absence of controlled trials. Thrombolysis and embolectomy are probably both effective while anticoagulation alone seems to be less effective [1]. In our case taking in mind the low to intermediate risk profile of the patient, full anticoagulation was chosen for the patient and great response was seen.
Conclusion
According to the right heart thrombi European registry, 30 days prognosis in patient with RiHT is predominantly related to hemodynamic consequences of PTE and not to the characteristics of RiHT. Therefore, recommended methods of prognostic PE stratification are applicable also to patients with RiHT. RiHT patients with low risk PE defined by simplified Pulmonary Embolism Severity Index (sPESI) 0 or by hemodynamic stability with preserved right ventricular function have good prognosis and anticoagulation seems to be sufficient.
[1]. Koc M, Kostrubiec M, Elikowski W, Meneveau N, Lankeit M, Grifoni S, Outcome of patients with right heart thrombi: the Right Heart Thrombi European RegistryEuropean Respiratory Journal 2016 21:ERJ-00819. [Google Scholar]
[2]. Chartier L, Béra J, Delomez M, Asseman P, Beregi JP, Bauchart JJ, Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patientsCirculation 1999 99:2779-83. [Google Scholar]
[3]. Torbicki A, Galié N, Covezzoli A, Rossi E, De Rosa M, Goldhaber SZ, Right heart thrombi in pulmonary embolism: results from the International Cooperative Pulmonary Embolism RegistryJ Am Coll Cardiol 2003 41:2245-51. [Google Scholar]
[4]. Dincer HE, Right heart thrombusClinical Pulmonary Medicine 2012 9(5):226-31. [Google Scholar]
[5]. Dincer I, Dandachi R, Atmaca Y, Erol C, Caglar N, Oral D, A recurrent right heart thrombus in a patient with Behçet’s diseaseEchocardiography 2001 18(1):15-18. [Google Scholar]
[6]. The European Cooperative Study on the clinical significance of right heart thrombiEuropean Working Group on EchocardiographyEur Heart J 1989 10:1046-59. [Google Scholar]
[7]. Rose PS, Punjabi NM, Pearse DB, Treatment of right heart thromboemboliChest 2002 121:806-14. [Google Scholar]