Children require omega-6 and omega-3 PUFA for neural integrity and function. The omega-3 PUFA like Alpha-Linolenic Acid (ALA), Eicosapentanoic Acid (EPA) and Docosahexanoic Acid (DHA), are necessary for brain development and cell membrane functioning [5]. The omega-6 fatty acid Gammalinolenic Acid (GLA) is a metabolic precursor to AA, hence important in brain growth and development. Colquhoun and Bunday first proposed a link between hyperactivity and PUFA deficiency [6]. Mechanisms include insufficient dietary intake, less conversion of short chain PUFAs to long chain PUFAs or rapid metabolism of long chain PUFAs.
The conventional management of ADHD involves pharmacological treatment with stimulants or atomoxetine, in combination with non pharmacological management like behaviour therapy. However, the findings of PUFA deficiency in ADHD children lead to interventional studies which supplemented usual treatment with these fatty acids. The results have been mixed with some studies showing improvement in symptoms of ADHD along with improvements in domains like physical aggression and irritability [7], while Cochrane database review found little or no significant benefit in ADHD symptoms [8]. There have been inconsistencies in sample sizes, selection criterias, type and dosage of PUFA supplementation, follow-up times and other methodological issues [8]. We conducted this study with the objective of evaluating the effect of PUFA administration in Indian children with ADHD. To the best of our knowledge, we could not find any Indian study on this issue. Also, considering the growing percentage of younger population in Asian subcontinent, the subject is a pertinent one. Hence, the present study aimed at evaluating the effect of PUFA administration in Indian children with ADHD.
Materials and Methods
The study was conducted at a tertiary care multi-specialty hospital of India. Departments of Paediatrics and Psychiatry of the medical college associated with the hospital were involved in conducting the study over the period of one year. The study was approved by the Institutional Ethics Committee and the Thesis Review committee.
The study was a prospective double blind randomized control trial. Children aged 4-11 years presenting to the paediatrics Out Patients Department (OPD) of the hospital were screened for symptoms of ADHD using Conners’ Parent Rating Scale-Revised: Short Form (CPRS-R:S) and behavioural observation. CPRS-R:S is a 27 item, 4 point Likert scale with proven validity and reliability [9]. Those screened positive were examined by a psychiatrist and diagnosed as ADHD according to the DSM-IV TR criteria and Kiddie-Schedule for Affective Disorders and Schizophrenia - Present and lifetime version (KSADS-PL) [10]. The K-SADS-PL is a semi-structured diagnostic interview designed to assess current and past episodes of psychopathology in children and adolescents according to DSM-III-R and DSM-IV criteria [10]. A prior informed and written consent was taken from the parents of the children, explaining the full procedure to them. All the consenting children/parents were enrolled in the study.
A detailed history was obtained and thorough physical examination was conducted in all these children to rule out any acute physical illness, hearing or visual defect, gross brain damage, epilepsy & autism. In history, emphasis was given on antenatal and birth history to find out pregnancy and delivery complications, low birth weight and prenatal substance exposure. The inclusion criteria were children with age 4-11 years, both males and females, diagnosed with ADHD after detailed evaluation and parental consent for participation. The exclusion criteria were any acute physical illness requiring hospital admission, autism, mental retardation, chronic physical disability such as hearing or visual impairment, epilepsy and psychosis. It was ensured that these children were not on any other medication, treatment, street drugs or other nutritional supplements.
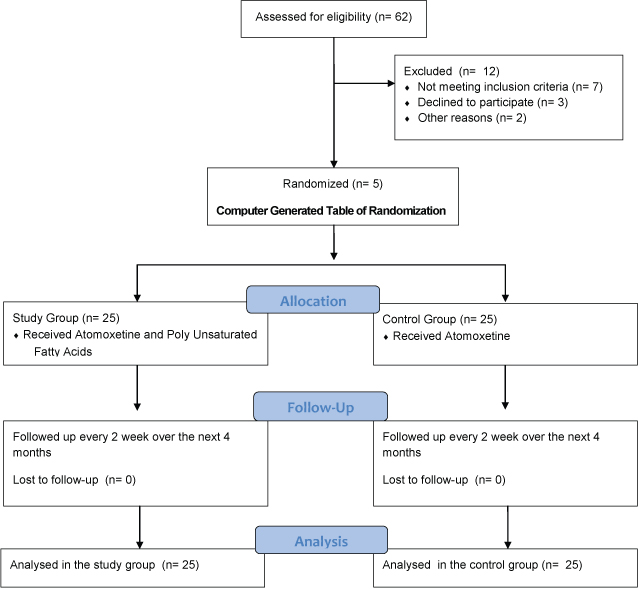
The children were then randomized according to a computer generated table of randomization and assigned to either the study group or control group, by an independent pharmacist of the department. The control group was given Atomoxetine, a nor-epinephrine reuptake inhibitor, in the dose of 0.5mg/kg/day. Study group was given Atomoxetine and supplemented with PUFA in the form of a pill containing 180 mg of EPA and 120 mg of DHA. The drugs were given in an envelope which was labeled as number 1 and 2, for the study and control groups respectively. Both the groups were followed up every 2 week over the next 4 months using the CPRS-R:S. The data was recorded in individualized files by the blinded primary investigator. Both the participants and primary investigator were blind to the group allocation. After successful completion of the trial, blinding was unfolded and data was analysed. The process of enrollment and flow chart of randomization is explained in [Table/Fig-1].
Flow chart for randomization
The data was carefully analysed by SPSS software (17th version) with the help of a statistician. The data collected for case and controls was entered in the EXCEL programme. Confidence interval of 95% was used. The complete data was analysed using appropriate parametric and non parametric tests. Correlation was done between various socio-demographic and illness related parameters. For all analyses, probability of 5% or less was assumed to represent statistical significance.
Results
A total of 62 parents and children were screened for inclusion in the study. However, 7 of the screened children were excluded after psychiatric examination as they did not match the criteria for ADHD after KSADS-PL assessment and clinical examination. Three of the parents did not consent for study and follow-up. Two children had co-morbid disorders (epilepsy and severe mental retardation) and had to be excluded. Thus, a total of 50 children were enrolled and completed the study.
These 50 children diagnosed with ADHD were randomized to study group (n=25) and control group (n=25). Both the groups matched well for age and sex distribution. Also, the subject distribution for classification of ADHD as per DSM-IV TR, matched in control and study groups. The age and sex distribution and clinical parameters of children included in study and control group are demonstrated in [Table/Fig-2].
Demographic profile and clinical parameters of children in control and study groups.
| Socio-demographic and clinical parameters | Control group(n) | Study group(n) |
|---|
| Age | 5 years | 6 | 5 |
| 6 years | 13 | 12 |
| 7 years | 6 | 8 |
| Sex | Male | 18 | 17 |
| Female | 7 | 8 |
| Type of ADHD | Inattentive | 4 | 5 |
| Hyperactive | 3 | 5 |
| Combined | 18 | 15 |
In the study, all the children fell in the age range of from 5 years to 7 years, while 50% of the children were of 6 years of age. The mean age of ADHD presentation in our study was around (6 ± 2.1 years). The mean age of boys was 5.77±2.4 years and that of girls was 5.13±2.2 years. Majority of the children in the study were males (n=35). The overall ratio of males to females in the study population was 2.3:1 (35:15). Combined type of ADHD was the most common type found in the study (n=33, 66%), followed by almost equal numbers in inattentive and hyperactive group.
We compared the improvement in ADHD rating scale scores between the two groups after completing the intervention. The study group had pre-intervention scors of 39.1 ± 2.2, at the start of the study. While the control group’s score was 38.4± 2.31. The post intervention scores at 4 months, in the study and control groups were 36.6±2.21 and 37.4±2.18 respectively [Table/Fig-3]. The reduction in the Conners’ ADHD scores were 2.5 (p-value = 0.08) and 1.0 (p-value = 0.28) respectively. The study group had comparatively more reduction in Conners’ ADHD scores than the control group, however, the reduction in scores was not statistically significant.
Effect of intervention on symptoms of ADHD in control and study groups.
| Pre intervention scores(Mean ± S.D.)0 week | Post intervention scores(Mean ± S.D.)4 months | p-value |
|---|
| Total score | Control group (N=25) | 38.4 ± 2.31 | 37.4 ± 2.18 | 0.28 |
| Study group (N=25) | 39.1 ± 2.12 | 36.6 ± 2.21 | 0.08 |
| Sex Distribution |
| Males | Control group (N=18) | 39.4±2.22 | 37.4±2.16 | 0.14 |
| Study group (N=17) | 39.3±2.15 | 36.5±2.14 | 0.07 |
| Females | Control group (N=7) | 39.3±2.18 | 37.4±2.14 | 0.15 |
| Study group (N=8) | 39.1±2.21 | 37.2±2.18 | 0.16 |
| Age Distribution |
| 5 years | Control group (N=6) | 38.4±2.14 | 36.1±2.12 | 0.10 |
| Study group (N=5) | 39.3±2.16 | 37.5±2.15 | 0.16 |
| 6 years | Control group (N=13) | 39.4±2.12 | 37.4±2.14 | 0.14 |
| Study group (N=12) | 40.1±2.08 | 37.3±2.10 | 0.05 |
| 7 years | Control group (N=6) | 38.5±2.12 | 37.4±2.2 | 0.24 |
| Study group (N=8) | 38.8±2.16 | 37.4±2.16 | 0.20 |
| Classification of ADHD |
| Combined type | Control group (N=18) | 39.3±2.18 | 37.4±2.14 | 0.15 |
| Study group (N=15) | 41.1±2.16 | 38.2±2.12 | 0.04 |
| Inattentive type | Control group (N=4) | 38.4±2.2 | 37.5±2.14 | 0.28 |
| Study group (N=5) | 37.2±2.13 | 36.4±2.12 | 0.30 |
| Hyperactive type | Control group (N=3) | 37.4±2.2 | 36.3±2.14 | 0.22 |
| Study group (N=5) | 36.1±2.16 | 35.0±2.15 | 0.20 |
We tried to evaluate the improvement in ADHD scores among the groups, based upon various socio-demographic and clinical parameters [Table/Fig-3]. We found that males in the study group had significant improvement in ADHD scores at the end of study (4 months), compared to males in control group. However, the improvement was not clinically significant (p = 0.7). There was no difference in the scores among females in the study as well as the control groups. The scores for combined type of ADHD in the study group were 41.1±2.16 (0 week) and 38.2±2.12 (4 months) with p-value of 0.04. The scores for inattentive and hyperactive type of ADHD in the study and control groups did not differ much at the end of 4 months.
Discussion
The results show that PUFA supplementation improved the symptoms of ADHD, which is evident by the reduction in Conners’ ADHD rating scale scores, although the effect was not clinically significant (p> 0.05). In our study, as we supplemented our study group with PUFA supplements and followed them on ADHD rating scale scores every 2 week for 4 months, there was greater reduction in ADHD scores (p = 0.08) as compared to the control group (p = 0.28).
There have been contrasting results in previous studies on effect of PUFA supplementation in ADHD. While a few studies have found positive effects and clinical improvement of Omega 3 PUFA supplementation in children with ADHD, most of the studies did not find significant improvements. This led to a Cochrane systematic review of clinical trials, published in 2012, which found no beneficial effect of PUFA supplementation on ADHD symptoms in children and adolescents [8].
Bos et al., in a recent study, concluded that omega-3 supplementation may be an effective augmentation for pharmacological treatments of ADHD [11]. Similar positive beneficial effects have been demonstrated in a meta-analysis by Bloch et al., [12]. The findings from the Oxford-Durham trial also suggest that omega-3/6 PUFA supplementation may improve ADHD-like behavioural symptoms and educational difficulties [13]. Still, the effect sizes of these studies were small. A recent study by Barragán et al., (2014) reported greater effect of combination of methylphenidate and omega-3 PUFAs compared with children only receiving methylphenidate [14].
Voigt et al., found no improvement in symptoms of ADHD in children after supplementation with DHA (345mg/day) for 4 months [15]. Hirayama et al., found that supplementation of 0.61 g of omega-3 fatty acids per day for two months had no effect when analysing parent and teacher assessment separately in ADHD children. However, when analysing assessment together, physical aggression significantly improved [16]. Stevens et al., supplemented ADHD children with 0.66 g/day of both omega-3 and omega-6 PUFA for 4 months. They measured AA:EPA ratio and found that it decreased from 33.04 to 15.19 but the symptoms did not improve suggesting that AA:EPA ratio may not have been lowered enough to observe a greater impact on behaviour [17]. Similarly, we also did not find significant improvement in ADHD symptoms. However, we could not estimate the blood PUFA levels because of limitation of resources.
The male to female ratio (2.3:1) was significantly higher in the present study, which is in concordance with epidemiological surveys in Western (2:1 to 10:1) and Indian population (3.3 to 7.7:1) [18–21]. The gender differences point towards a biologically based, and genetically transmitted aetiology of hyperkinetic disorders. In the present study ADHD was associated with first born status (58%). A few studies have also found 24%-54% of ADHD cases to be the eldest sibling [22,23], but a study by Goodman and Stevenson could not find any relationship with birth order and hyperactivity [24]. In our study, no risk factors like prematurity and low birth weight were found. Certain workers like Mukhopadhyay and Goodman et al., also did not find high rate of such prenatal risk factors [21,24].
In our study, there was an interesting observation that males respond better to PUFA supplements than females. Also, the children with age 6 years had better reduction of symptoms. Both of these results might me due to the fact that this group had maximum number of study as well as control subjects. Dervola et al., reported sex-specific changes in rat models of ADHD (more improvement in male rats) and attributed it to changes in presynaptic striatal monoamine and amino acid signaling [25].
The combined type of ADHD showed more reduction of symptoms than the other two types (inattention and hyperactivity). Parents of these children observed a significant reduction in their hyperactive and impulsive symptoms. This observation is consistent with Richardson et al., who reported better improvement in dimensions of hyperactivity and impulsivity than attention [13]. However, one study found positive effects on all dimensions of ADHD [26]. Still, some studies showed greater improvement in domain of inattention, rather than hyperactivity [27]. Results are not surprising as changes in activity/impulsivity levels are much easily and readily evident as compared to changes in attention.
Epidemiologic data suggests that population with lower PUFA consumption and hence, lower plasma tissue contents of PUFA including DHA have higher rates of psychiatric disorders, learning disorders and behavioural disorders. Essential fatty acids are required for normal cognitive function. There is a direct relationship between plasma phospholipids, DHA content and metabolism of serotonin and dopamine within the Central Nervous System (CNS) [28–30]. Omega-3 PUFA supplementation leads to increased prefrontal brain activation, thereby improving the performance in sustained attention tasks in both typically developing children and children with ADHD [31–33].
Our study is perhaps the first study in Indian population that tries to evaluate the effect of PUFA supplementation on ADHD symptoms. The use of Conners’ Parent rating scale, DSM IV TR criterias and Kiddie SADS criterias along with involvement of paediatrics and psychiatry department lends strength to the diagnostic value. Also, frequent follow-ups prevented any dropouts from the study. The design of the study (double blind randomized control trial) and use of an active established drug in both groups add to the research value.
Limitation
We report three limitations of our study. We were not able to do the biochemical analysis of nutritional status as well as baseline blood PUFA levels, so it is not known whether the children had initial PUFA and nutritional deficiencies. Further inspection of both nutrient status and PUFA at baseline and correlations of supplementation with magnitude of improvement could confirm relationship between nutrients and/or PUFA deficiency and response. The possibility that supplementation of nutrients in combination with PUFA might provide greater benefits than isolated nutrients (e.g., Zinc, magnesium) requires further investigation [34,35]. Secondly, the follow-up period for our study was short i.e., 4 months. Giles et al., concluded in a systematic review that study period was short for all studies and advocated that follow-up must be beyond three months and preferably considerably longer [8]. Because the turnover of fatty acids in the brain is likely be quite low in 6-12-year-old children [13], a longer period of supplementation and/or a larger amount of supplementation might be required to alter the fatty acid content of the nervous system. Thirdly, we did not supplement children with omega-6 PUFA. It is important to remember that the plasma phospholipids content of AA is also low in children with ADHD and decreases further with DHA supplementation [36]. Thus, any future study of the effect of DHA on ADHD symptoms should include supplementation with both AA and DHA.
Conclusion
The supplementation with PUFA in children with ADHD did show some reduction in symptoms. However, it was not statistically significant. It may be attributed to short duration of the study and supplementation with only omega 3 PUFA. Still, it is the first double blind randomized control trial in Indian children with ADHD. The study may lay a foundation for future similar research trials in Indian as well as Asian population.
Future studies should evaluate the same or a higher dose of DHA given for longer period and supplementation with combination of omega 3 and omega 6 fatty acids. The possibility that more optimal DHA intake during early life may decrease the prevalence of ADHD should also be evaluated. Also, the effect of individual PUFA should also be evaluated. However, it is clear from the data presented here that PUFA supplementation for 4 months did ameliorate the symptoms of ADHD but not significantly.