Predictive Value of Total Serum Bilirubin within 6 Hour of Birth for the Development of Hyperbilirubinemia After 72 hours of Birth
Chaitra Bandi1, Raghavendra Vanaki2, Ashok V. Badakali3, Ramesh R Pol4, Bhuvaneshwari Yelamali5
1 Resident, Department of Paediatrics, S. N. Medical College and HSK Hospital, Bagalkot, Karnataka, India.
2 Associate Professor, Department of Paediatrics, S. N. Medical College & HSK Hospital, Bagalkot, Karnataka, India.
3 Professor, Department of Paediatrics, S. N. Medical College & HSK Hospital, Bagalkot, Karnataka, India.
4 Associate Professor, Department of Paediatrics, S. N. Medical College & HSK Hospital, Bagalkot, Karnataka, India.
5 Professor, Department of Paediatrics, S. N. Medical College & HSK Hospital, Bagalkot, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Raghavendra Vanaki, Associate Professor, Department of Paediatrics, S. N. Medical College & HSK Hospital, Navanagar, Bagalkot-587102, Karnataka, India.
E-mail: drraghavendravanaki@gmail.com
Introduction
Neonatal jaundice is benign and no intervention might be required, but jaundice can be associated with an underlying disease condition, which therefore warrants accurate and unbiased estimation of bilirubin. Total Serum Bilirubin (TSB) measurements (at discharge between 18 hours and 72 hours) can be used to predict the chances of developing severe hyperbilirubinemia.
Materials and Methods
The present hospital-based prospective study was undertaken to determine the predictive value of serum bilirubin before 6 hours of life for subsequent hyperbilirubinemia in healthy term neonates. One hundred and fifty healthy term newborns delivered during January 2013–December 2013 at Hanagal Shri Kumareshwara Hospital and Research Centre, S. Nijalingappa Medical College, Bagalkot Karnataka, India, were included in the study. Serum bilirubin levels were estimated twice, first, within 6 hours of life and second, after 72 hours of life. Bilirubin values were plotted on previously published nomograms. Sensitivity, specificity of the test was established.
Results
A measure of TSB levels (within 6 hours of life) across the study population, showed that maximum number of infants (70/150) had TSB level between 4.1 and 5.5 mg/dL and 16 infants had TSB level >5.6 mg/dL. The TSB levels (after 72 hours of life) showed that maximum newborns (83/150) had TSB levels between 12.8 and 15.3 mg/dL and 9 infants had TSB levels between 7.7 and 10.2mg/dL. Eighteen infants developed hyperbilirubinemia. Newborns with TSB value of >4.95mg/dL within 6hours of life had developed significant hyperbilirubinemia after 72 hours of life with sensitivity of 100% and specificity of 89% (p=0.0001), which was highly statistically significant.
Conclusion
A TSB level of >5 mg/dL within 6 hours of birth would serve as a predictor for risk of subsequent hyperbilirubinemia in the near future.
Neonatal jaundice, Fetal-maternal risk
Introduction
Neonatal hyperbilirubinaemia, defined as a TSB >5 mg/dL, is a commonly encountered clinical condition among the newborns. Nearly 60% of term newborns present with clinical jaundice during the first week of life [1]. Usually hyperbilirubinaemia occurs in the absence of any underlying diseases; however, it may be associated with severe illnesses such as hemolytic disease, metabolic and endocrine disorders, anatomic abnormalities of the liver, and infections [2]. Acute bilirubin encephalopathy and kernicterus are the two important neurological manifestations of hyperbilirubinaemia [3]. Unmonitored and untreated hyperbilirubinaemia may lead to neurological complications and hence, it is important to identify hyperbilirubinaemia and initiate appropriate treatment.
Certain factors would predispose the infants to hyperbilirubinaemia and some of the common fetal-maternal risk factors include fetal-maternal blood group incompatibility, prematurity, and a previously affected sibling. Other maternal risk factors are breastfeeding, drugs (diazepam, oxytocin), Asian, native American ethnicity, and gestational diabetes. Besides the maternal risk factors, neonatal risk factors are birth trauma, certain drugs (sulfisoxazole acetyl, erythromycin ethyl succinate, chloramphenicol), excessive weight loss after birth, infections, infrequent feedings, male gender, polycythemia and delayed meconium passage [2].
Bilirubin is the final breakdown product of hemoglobin that is excreted in the bile after conjugation. Depending on the bilirubin levels, the jaundice may by physiological or pathological. In neonates, physiological jaundice develops within 2–3 days of birth, with a rise in TSB levels to 6–8mg/dL or to a maximum of 12mg/dL on day 3 and subsequent fall in the TSB level within normal limits. In case of pathological jaundice, the TSB levels are constantly increasing beyond the normal values from first day of birth [(>5 mg/dL on day 1; 10 mg/dL (second day) and 12–13 mg/dL there after to pathological level of >17 mg/dL)]. One-third of exclusively breast-fed infants ara also likely to develop mild jaundice but in the third week of life and it may persist for few months. A TSB level of >10mg/dL after the third week of life could be attributed to β-glucuronidases and non-esterified fatty acids in the breast milk that apparently inhibits normal bilirubin metabolism. However, the TSB levels might decline over time [1,2].
In general, neonatal jaundice is benign and no intervention might be required, but jaundice can be associated with an underlying disease condition, which therefore warrants accurate and unbiased estimation of bilirubin. Diagnosis of hyperbilirubinaemia with the aid of Kramer index [4] could be deceptive, especially in children with dark skin. If total and direct bilirubin levels are beyond the normal limits (total bilirubin: 0.3–1.2mg/dL, direct bilirubin: 0.0–0.3 mg/dL) then liver disease could be suspected [5]. Transcutaneous bilimeter (TcB) and/or TSB measurement should be performed on every infant within 8–12 hour after birth. In the event of diagnosing jaundice, subsequent monitoring through TcB or TSB will depend on the nomogram zone [3].
Timed TSB measurements (at discharge between 18 hours and 72 hours) can be used to predict the chances of developing severe hyperbilirubinaemia [6]. The present hospital-based prospective study was undertaken to determine the predictive value of serum bilirubin before 6 hours of life for subsequent hyperbilirubinaemia in healthy term neonates.
Materials and Methods
One hundred and fifty healthy term newborns delivered during January 2013–December 2013 at Hanagal Shri Kumareshwara Hospital and Research Centre, S.Nijalingappa Medical College, Bagalkot, Karnataka, India, were included in the study after obtaining the necessary consent from the ethical committee and parents. Sample size was calculated using OPEN Epi software 2.3.1 version which takes design effect and prevalence into consideration.
Exclusion criteria
ABO and Rh incompatibility
Babies with life threatening birth defects
Prematurity
Congenital anomalies
Infant of diabetic mother
Birth Asphyxia (APGAR <7 in first 5 min)
In addition, neonates who developed direct hyperbilirubinaemia with features suggestive of sepsis and respiratory distress were excluded from the study.
Data related to gender, birth weight, gestational age, parity, mode of delivery, feeding pattern, APGAR score, mother’s blood group, baby’s blood group was obtained. Total serum bilirubin, direct and indirect bilirubin was estimated by Modified Van den Bergh’s kit method.
Serum bilirubin levels were estimated twice, first, within 6 hours of life and second, after 72 hours of life. Bilirubin values were plotted on previously published normograms such as AAP and Bhutani’s charts [7]. Sensitivity and specificity of the test was established. Treatment for hyperbilirubinaemia was decided based on American Academy of Paediatrics guidelines [3]. AAP guidelines are used for phototherapy in >35 weeks of gestation. High risk at 72 hours is >13.5mg/dL, Medium risk is 16.5mg/dL and Low risk is >18mg/dL. For well infants usually it can be adjusted around 16.5mg/dL i.e., around medium risk zone which is considered in our study.
Statistical Analysis
Maternal and neonatal data were collected in predesigned and pretested proforma. Sensitivity and specificity of the test was calculated. For determining significance of each test p-value was used. Bilirubin values were plotted on previously published normograms such as AAP and Bhutani’s charts.
Results
The observed baseline characteristics of mothers and newborns are presented in [Table/Fig-1]. The male to female ratio was 0.97:1 (74 male and 76 female). Significant number of infants weighed above 2.5 kg (148 infants). Most the infants were delivered full term normally (N=126) only 24 infants were delivered through lower (uterine) segment Caesarean section. Maximum number of infants was with ‘O’ blood type. Except for one infant, all the other infants were Rh compatible. All the infants were delivered after 36 weeks of gestation but maximum number of infants were born at 41–42 weeks of gestation (N=115). A measure of TSB levels (within 6 hours of life) across the study population, showed that maximum number of infants (70/150) had TSB level between 4.1 and 5.5 mg/dL and 16 infants had TSB level >5.6 mg/dL [Table/Fig-2]. The TSB levels (after 72 hours of life) showed that maximum newborns (83/150) had TSB levels between 12.8 and 15.3 mg/dL and 9 infants had TSB levels between 7.7 and 10.2mg/dL [Table/Fig-3]. Eighteen infants developed hyperbilirubinaemia. Maximum number of newborns weighing between 2501gm and 2850gm were born after 41 weeks of gestation (84.5%).
Baseline characteristics.
| Characteristics | No. (%) |
|---|
| MATERNAL |
| Type of delivery |
| Full term normal vaginal delivery (FTND) | 126 (84%) |
| Caesarean | 24 (16%) |
| Parity |
| 1 | 94 (62.7%) |
| 2 | 32 (21.3%) |
| 3 | 22 (14.7%) |
| ≥ 4 | 2 (1.3%) |
| Blood group |
| A | 13 (8.7%) |
| B | 47 (31.3%) |
| AB | 33 (22%) |
| O | 57 (38%) |
| NEONATAL |
| Sex |
| Males | 74 (49.3%) |
| Females | 76 (50.7%) |
Distribution of total serum bilirubin (TSB) within 6 hours of life in study population.
| TSB range within 6 hours | Number of newborns | Percent |
|---|
| 2.6-4.0 | 64 | 42.7 |
| 4.1-5.5 | 70 | 46.7 |
| >5.6 | 16 | 10.7 |
| Total | 150 | 100.0 |
Distribution of total serum bilirubin (TSB) after 72 hours of life in study population.
| TSB range after 72 hours | Number of newborns | Percent |
|---|
| 7.7-10.2 | 9 | 6.0 |
| 10.3-12.7 | 39 | 26.0 |
| 12.8-15.3 | 83 | 55.3 |
| >15.4 | 19 | 12.7 |
| Total | 150 | 100.0 |
Distribution of TSB within 6 hours and at 72 hours of life according to gestational age and birth weight is depicted in [Table/Fig-4]. Of the 18 infants who developed hyperbilirubinaemia, maximum number of them were ‘B’ type blood group (N=7), maximum number of them were born after 41 weeks of gestation, and weighed between 2.51kg and 2.85kg. Of the 18 infants who developed significant hyperbilirubinaemia, the TSB levels were >5.6mg/dL within 6 hours of life in 13 infants [Table/Fig-5]. Infants who had TSB level >15.4mg/dL after 72 hours developed significant hyperbilirubinaemia.
Distribution of total serum bilirubin (TSB) within 6 hours and 72 hours of life according to gestational age and birth weight.
| TSB (mg/dL) within 6 hours | TSB (mg/dL) after 72 hours |
|---|
| Gestational age |
|---|
| 2.6-4.0 | 4.1-5.5 | >5.6 | Total | 7.7-10.2 | 10.3-12.7 | 12.8-15.3 | >15.4 | Total |
|---|
| 37 | 2 | 2 | 0 | 4 | 0 | 3 | 1 | 0 | 4 |
| 38-40 | 12 | 13 | 6 | 31 | 4 | 5 | 15 | 7 | 31 |
| >41 | 50 | 55 | 10 | 115 | 5 | 31 | 67 | 12 | 115 |
| Total | 64 | 70 | 16 | 150 | 9 | 39 | 83 | 19 | 150 |
| Birth weight |
| 2.6-4.0 | 4.1-5.5 | >5.6 | Total | 7.7-10.2 | 10.3-12.7 | 12.8-15.3 | >15.4 | Total |
| 2.5kg | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 2 | 2 |
| 2.56-2.85kg | 29 | 33 | 9 | 71 | 5 | 19 | 37 | 10 | 71 |
| >2.86kg | 35 | 36 | 6 | 77 | 4 | 20 | 46 | 7 | 77 |
| Total | 64 | 70 | 16 | 150 | 9 | 39 | 83 | 19 | 150 |
Prevalence of hyperbilirubinemia according to total serum bilirubin (TSB) levels estimated within 6 hours of life.
| TSB (mg/dL) | Presence of hyperbilirubinemia | Total |
|---|
| Yes | No |
|---|
| 2.6-4.0 | 0 | 64 | 64 |
| 4.1-5.5 | 5 | 65 | 70 |
| >5.6 | 13 | 3 | 16 |
| Total | 18 | 132 | 150 |
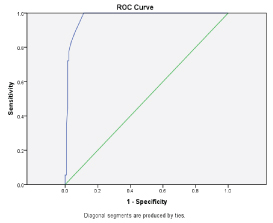
Area under the Receiver Operating Characteristic (ROC) curve was 0.977 (p=0.0001), and the best predictive TSB value for subsequent hyperbilirubinaemia was 4.95mg/dL with a specificity of 88% and sensitivity of 100% [Table/Fig-6].
Receiver operating characteristic (ROC) curve depicts specificity of 88% and sensitivity of 100%.
Discussion
There is a rising concern about increasing incidence of kernicterus in healthy term neonates. Hyperbilirubinaemia is one of the most common causes for readmission of the newborns. Hence, it is important to accurately measure the TSB for establishing a diagnosis of hyperbilirubinaemia in infants who are discharged early from the hospital. Total serum bilirubin levels are usually 1–3mg/dL at birth and peaks by 5–15 days and declines by 3 weeks. Our study hypothesized that a high serum bilirubin level at birth would predict a hyperbilirubinaemia in the near future. The objective of this study was to quantify the relationship between TSB levels within 6 hours of life with that of TSB levels after 72 hours. To avoid fatal effects of late onset of jaundice, AAP recommends all neonates, who are discharged <48 hours after birth should be followed by a health care professional in an office, clinic, or at home within 2–3 days of discharge [3].
The available literature shows that the incidence of significant hyperbilirubinaemia ranges between 9% and 12% [8–10]. In our study also, the incidence of significant hyperbilirubinaemia was 12%. Male gender is a known risk factor for hyperbilirubinaemia [6], but in our study hyperbilirubinaemia was found in 61.1% (11 out of 18 infants with hyperbilirubinaemia) female babies and 38.8% (7 out of 18 infants with hyperbilirubinaemia) male babies. Oxytocin induced delivery or Caesarean section is known to increase the bilirubin levels in infants [11,12]. However, in our study, the higher number of deliveries was through vaginal and the incidence of significant hyperbilirubinaemia was predominant in infants delivered vaginally.
Alpay et al., opined that TSB level of >6mg/dL in the first 24 hours of life is a predictor of significant hyperbilirubinaemia in near future in all term newborns. In their study, of 206 newborns whose TSB level was ≥6 mg/dL in the first day of life, 54 (26.21%) developed significant hyperbilirubinaemia. On the contrary, 6 of the 292 newborns (2.05%) who had a TSB level of <6 mg/dL on the first day developed significant hyperbilirubinaemia [8]. Agarwal et al., showed that TSB level of 6mg/dL at 24±6 hours of life was a predictive cut-off for development of hyperbilirubinaemia. The author reported that 21 (27.2%) of 77(36.1%) infants whose TSB was >6mg/dL developed subsequent hyperbilirubinaemia while only one infant developed subsequent hyperbilirubinaemia among 136 infants whose TSB was <6mg/dL [9]. Randev et al., reiterated that estimation of TSB within 24 hour of birth could be considered as a reliable screening test for neonates, who would be at risk for subsequent hyperbilirubinaemia. A TSB level <6.4mg/dL on day 1 of life carries minimum risk of subsequent hyperbilirubinaemia [10]. In ABO incompatible infants, TSB levels at 6 hours of life have been used to predict the risk of subsequent hyperbilirubinaemia [13,14]. The 35th and 90th percentile zone that nearly corresponds to TSB levels of 3.3mg/dL and 6.5mg/dL at the 6 hours of life are ideal demarcations in predicting the risk of subsequent hyperbilirubinaemia [13]. Keerti et al., showed that TSB level of >2mg/dL at 6 hours of life as the predictive value for risk of subsequent hyperbilirubinaemia [15]. In our study, newborns with TSB value of >4.95mg/dL within 6 hours of life had developed significant hyperbilirubinaemia after 72 hours of life with sensitivity of 100% and specificity of 89% (p=0.0001), which was highly statistically significant.
Conclusion
Hyperbilirubinaemia is a common problem in neonatal wards. Re-admission owing to clinical jaundice is significant among infants who are discharged early after birth. Despite the AAP recommendations, it is difficult to monitor the TSB levels in infants at risk for hyperbilirubinaemia. Although early detection of abnormal TSB levels are helpful in predicting the risk of subsequent hyperbilirubinaemia, there has been no consensus as to what is the accurate and nonbiased levels of TSB at any time after birth. Researchers have used 24 hours as the earliest time for obtaining TSB value and a cut-off of >5mg/dL as a predictor for risk of subsequent hyperbilirubinaemia. In our study, we have found that TSB value of 4.95mg/dL obtained within 6 hours of life was highly predictive of significant hyperbilirubinaemia after 72 hours of life with sensitivity of 100%, specificity of 89%. Hence, screening infants for TSB levels within 6 hours of birth would be beneficial. A TSB level of >5 mg/dL with 6 hours of birth would serve as a predictor for risk of subsequent hyperbilirubinaemia in the near future.
[1]. Mishra S, Agarwal R, Deorari AK, Paul VK, Jaundice in the newbornsIndian J Paediatr 2008 75:157-63. [Google Scholar]
[2]. Porter ML, Dennis BL, Hyperbilirubinaemia in the term newbornAm Fam Physician 2002 65(4):599-607. [Google Scholar]
[3]. American Academy of Paediatrics and Subcommittee on HyperbilrubinaemiaManagement of hyperbilirubinaemia in the newborn infant 35 or more weeks of gestationPaediatr 2004 114(1):297-316. [Google Scholar]
[4]. Kramer LI, Advancement of dermal icterus in the jaundiced newbornAm J Dis Child 1969 118:454-58. [Google Scholar]
[5]. Puppalawar PV, Goswami K, Dhok A, Review on “Evolution of methods of bilirubin estimation”J Dent Med Sci 2012 1(3):17-28. [Google Scholar]
[6]. Barrington KJ, Sankaran K, Canadian Paaediatric Society Fetus and Newborn Committee. Guidelines for detection, management and prevention of hyperbilirubinaemia in term and late preterm newborn infantsPaediatr Child Health 2007 12(Suppl B):1-12B. [Google Scholar]
[7]. Bhutani VK, Johnson L, Sivieri EM, Predictive ability of a predischarge hour - specific serum bilirubin for subsequent significant hyperbilirubinaemia in healthy term and near term newbornsPaediatrics 1999 103:6-14. [Google Scholar]
[8]. Alpay F, Sarici SU, Tosuncuk HD, Serdar MA, Inanç N, Gökçay E, The value of first day bilirubin measurement in predicting the development of significant hyperbilirubinaemia in healthy term newbornsPaediatrics 2000 106:16A [Google Scholar]
[9]. Agarwal R, Kaushal M, Paul VK, Early neonatal hyperbilirubinaemia using first day serum bilirubin levelIndian Paediatr 2002 39:724-30. [Google Scholar]
[10]. Randev S, Grover N, Predicting neonatal hyperbilirubinaemia using first day serum bilirubin levelsIndian J Paediatr 2010 77:147-50. [Google Scholar]
[11]. Murki S, Kumar P, Majumdar S, Marwaha N, Narang A, Risk factors for kernicterus in term babies with non-hemolytic jaundiceIndian Paediatrics 2001 38:757-62. [Google Scholar]
[12]. Maisels MJ, Neonatal jaundice. In: Gleason, Ballard EdsNeonatology, pathophysiology and management of newborn 1981 2nd ednPhiladelphiaJB Lippincot:473-554. [Google Scholar]
[13]. Sarici SU, Yurdakök M, Serdar MA, Oran O, Erdem G, Tekinalp G, An early (sixth-hour) serum bilirubin measurement is useful in predicting the development of significant hyperbilirubinaemia and severe ABO hemolytic disease in a selective high-risk population of newborns with ABO incompatibilityPaediatrics 2002 109:e53 [Google Scholar]
[14]. Stoniene D, Buinauskiene J, Markuniene E, Tameliene R, Kudreviciene A, The value of diagnostic tests in predicting hyperbilirubinaemia in abo incompatibilityPaediatr Res 2011 70:735 [Google Scholar]
[15]. Kireeti AS, Srividya L, The role of first day serum bilirubin estimation in predicting significant hyperbilirubinaemia in healthy term newbornsInt J Res Dev Health 2014 2(2):58-69. [Google Scholar]