Giant Hydronephrosis (GH) is a rare urological disorder in adults. Sterling, in 1939 first defined it, as the volume of urine in the hydronephrotic sac, in an adult, exceeding 1000ml. It is also defined as, a kidney that occupies a hemi-abdomen, at least 5 vertebrae in length, meets or crosses midline [1,2]. Congenital Uretero-Pelvic Junction (UPJ) obstruction is the most common cause of GH. Management strategies in adult GH due to UPJ obstruction are not standardised. Conventional imaging modalities, like Intravenous Urography (IVU) and Computed Tomography Urography (CTU) usually show non-visualised renal units. Even, renal function assessment using radionuclide renal scan can be fallacious [3]. All these methods require exposure to radiation.
Identification of a sensitive biomarker of renal dysfunction, in the diagnosis and follow-up of these cases, seems discerning. Several factors have been investigated in paediatric UPJ obstruction (urine and serum carbohydrate antigen CA19-9, transforming growth factor-β1, endothelin-1, monocyte chemotactic peptide, epidermal growth factor) [4–8]; but, none till date for adult GH due to UPJ obstruction. These factors have demonstrated significant changes in the marker level after surgery.
Serum CA19-9 is a useful tumour marker for gastrointestinal and pancreatic cancer [9]. Although its increase in benign disease is unusual, but there are a very few studies and case reports with raised serum levels due to benign hydronephrosis and GH [10–12]. The normal range of serum CA19-9 in adult is 11.254kU/L±6.006kU/L [13]. We studied whether patients with adult GH due to UPJ obstruction has raised urine and serum CA19-9 levels. Furthermore, we investigated the probable value of urine and serum CA19-9 as a non-invasive prognostic clinical biomarker of renal dysfunction in adult GH due to UPJ obstruction.
Materials and Methods
This hospital based observational study was conducted after approval by the institutional ethics committee from July 2012 to December 2014. Patients were enrolled in the study after taking written informed consent. Out of 33 patients of GH due to UPJ obstruction, who were operated in our institute from July 2012 to December 2014, 24 adult patients with unilateral GH due to UPJ obstruction were included (Group 1). The patients excluded from the study were 9 patients of GH (2 patients with bilateral disease, 4 patients with pyonephrosis and 3 patients who lost to follow-up). Twenty four age and gender matched healthy adults (Group 2) were included as control. The controls were the residents and staffs from the hospital who were included in the study voluntarily.
The initial evaluation included ultrasound abdomen, CTU and DTPA renal scan. All the patients had normal blood urea nitrogen and creatinine level and sterile urine. Study exclusion criteria were: bilateral disease, presence of pyonephrosis, malignant tumour, renal dysfunction, diabetes mellitus, abnormal liver function and presence of benign diseases which could probably cause increased CA19-9.
Serum and first morning voided urine samples were collected from group 2, who had normal ultrasound abdomen. First morning voided urine and serum samples of CA19-9 were collected initially at diagnosis in group 2. At the time of surgery, urine from the affected pelvis was collected to determine CA19-9 level using 22 gauge needles. The patients with preoperative Glomerular Filtration Rate (GFR) > 10 ml / min and split renal function > 20 % underwent reconstructive procedures (pyeloplasty, ureterocalicostomy) and the rest had simple nephrectomy.
Analysed clinical factors were age, gender, laterality, crossing vessel, renal parenchymal thickness, renal function and operative outcome. Patients were followed up after surgery at 3 and 9 months with clinical examinations, urinalysis, diuretic renography, serum and voided urine samples for CA19-9 level, which were correlated with clinical factors. CA19-9 estimation was conducted using solid phase enzyme-linked immunosorbent assay (CA19-9 ELISA kit 96 T CalBiotech, USA).
A pilot study done prior to the study, showed standard deviation in pyeloplasty group = ±4200, standard deviation in nephrectomy group = 1800, Mean difference = 5700, Effect size = 1.9, Alpha Error(%) = 5, Power(%)= 80, sided = 2, Required sample size per group = 5.
Statistical Analysis
Statistical analysis was done using SPSS for windows version 22.0®. Data were expressed as mean ± SD. ANOVA tests were used when comparing means of more than 2 samples. Correlation coefficient was pearson’s r values. Box plot was used in determining the cut-off values of serum and urinary CA19-9 that gave the 95% confidence interval. The p<.05 was considered statistically significant.
Results
To the best of our knowledge, our study represents the first endeavour in evaluating the probable correlation between serum and urine CA19-9 with adult GH due to UPJ obstruction. Patient demographics and clinical parameters evaluated are shown in [Table/Fig-1].
Patient demographics and clinical parameters.
| Giant Hydronephrosis (group 1) | Control (group 2) |
|---|
| Age (In years) | NephrectomyPyeloplastyUreterocalicostomyTotal | 45.2 ± 11.43 (32 – 59)33.0 ± 10.28(19 – 52)44.5 ± 13.50(32 – 62)37.46 ± 12.06 (19 – 62) | 37.5 ± 12 (19 – 62) |
| Sex (Male : Female) | NephrectomyPyeloplastyUreterocalicostomyTotal | 3 : 210 : 54 : 017 : 7 | 17 : 7 |
| Laterality(Right : Left) | NephrectomyPyeloplastyUreterocalicostomyTotal | 4 : 110 :52 : 216 : 8 | |
| Renal parenchymal thickness(< 5 mm : >5 mm) | NephrectomyPyeloplastyUreterocalicostomyTotal | 5 : 02 : 131 : 38 : 16 | |
| Presence of crossing vesselYes : No | NephrectomyPyeloplastyUreterocalicostomyTotal | 1 : 34 : 121 : 36 : 18 | |
| Volume of intraoperative urine drained (ml) | NephrectomyPyeloplastyUreterocalicostomyTotal | 3320 ± 593.29(2500 - 3900)2013.33 ± 400.64(1500- 2700)2575 ± 330.50(2200 – 2900)2379.17 ± 677.89(1500 – 3900) | |
| Duration of follow-up(months) | | 15.17 ± 5 (9 – 26) | |
CA19-9 levels obtained from serum and voided urine preoperatively were significantly greater in group 1 (1665.95 ± 695.28 U /ml and 6596.66 ± 3303.34 U/ml, respectively) than in group 2 (10.39 ± 1.96 U / ml and 21.69 ± 1.40 U/ml, [Table/Fig-2]). In a subset analysis, the preoperative urinary CA19-9 had a significant statistical correlation between nephrectomy and reconstructive procedures (p <0.001).
The distribution of serum, voided urine and renal pelvic urine‡ CA19-9 levels in patients being operated for giant hydronephrosis (group 1) and control (group 2)
| Mean ± SDSerum CA19-9 (U / ml) | Mean ± SDVoided Urine CA19-9 (U / ml) | Mean ± SD Renal pelvic urine CA19-9‡ (U / ml) |
|---|
| Giant Hydronephrosis patients (Group 1) |
| Nephrectomy (1 A)PreoperativePost-operative at 3 monthsPost-operative at 9 months | 2113.52 ± 613.9410.84 ± 2.03*10.56 ± 1.2* | 11003.34 ± 4274.3822.67 ± 3.03*21.50 ± 2.89* | 59336.02 ± 24928.36__ |
| Pyeloplasty (1 B)PreoperativePostoperative at 3 monthsPostoperative at 9 months | 1425.58 ± 705.1318.42 ± 4.6*11.12 ± 1.50* | 5280.45 ± 1809.0571.30 ± 37.75*21.45 ± 1.88* | 36169.03 ± 26238.85__ |
| Ureterocalicostomy (1 C)PreoperativePostoperative at 3 monthsPostoperative at 9 months | 2007.87 ± 323.5020.36 ± 6.77*10.41 ± 1.31* | 6024.0750 ± 1600.7787.68 ± 66.24*21.22 ± 1.35* | 66325.10 ± 31334.36__ |
| Healthy Controls (Group 2) | 10.39 ± 1.96 | 21.69 ± 1.40 | _ |
*p< .05 Preoperative values as compared to postoperative values.
‡ Only in group 1.
CA: Carbohydrate antigen, SD: Standard deviation.
CA19-9 level measured from renal pelvic urine, obtained intra-operatively was 46021.50 ± 28788.05 U/ml, which was significantly greater than preoperative serum and voided urine CA19-9 (p <0.001 each). There were significant decrease in serum and urine CA19-9 level postoperatively at 3 months, as compared to preoperative values in all nephrectomy (p < 0.009 and p < 0.01) and 16 of 19 (p <0.001 and p < 0.001) reconstructive surgery patients [Table/Fig-2].
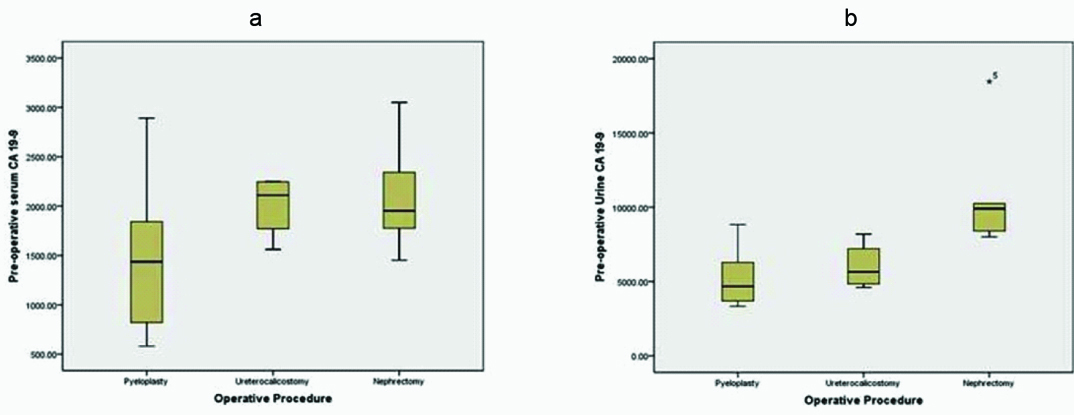
The Box Plot was constructed to determine the reference value for preoperative serum and urine CA19-9 levels with a CI 95%. For serum CA19-9 the cut-off values for the nephrectomy, pyeloplasty and ureterocalicostomy were 2113.52 CI {1351.21, 2875.82} U/ml, 1425.58 U/ml CI {1035.09, 1816.08} and 2007.87U/mlCI {1493.10, 2522.64} respectively. Whereas, the cut-off values for voided urine CA19-9 were 11003.3440 U/ml CI {5695.9960, 16310.6920}, 5280.45 U/ ml CI {4278.64, 6282.27} and 6024.07 U/ml CI {3476.88, 8571.26} respectively [Table/Fig-3a&b].
Box plot comparing different surgical procedures with preoperative serum (A) and urine (B) CA 19 -9 levels.
Three patients (2 pyeloplasty and 1 ureterocalicostomy) had persistently raised urine and serum CA19-9 level, higher than the cut-off values for nephrectomy in serum and voided urine, at 3 months follow-up, all the patients had GFR less than 10 ml/min and split renal function less than 20% at 3 months. These patients were considered as failure of the previous operation and ultimately underwent nephrectomy. Interestingly, all these three patients had preoperative renal parenchymal thickness less than 5 mm, initial GFR 10 to 15 ml/min and split renal function 20 to 25 %.
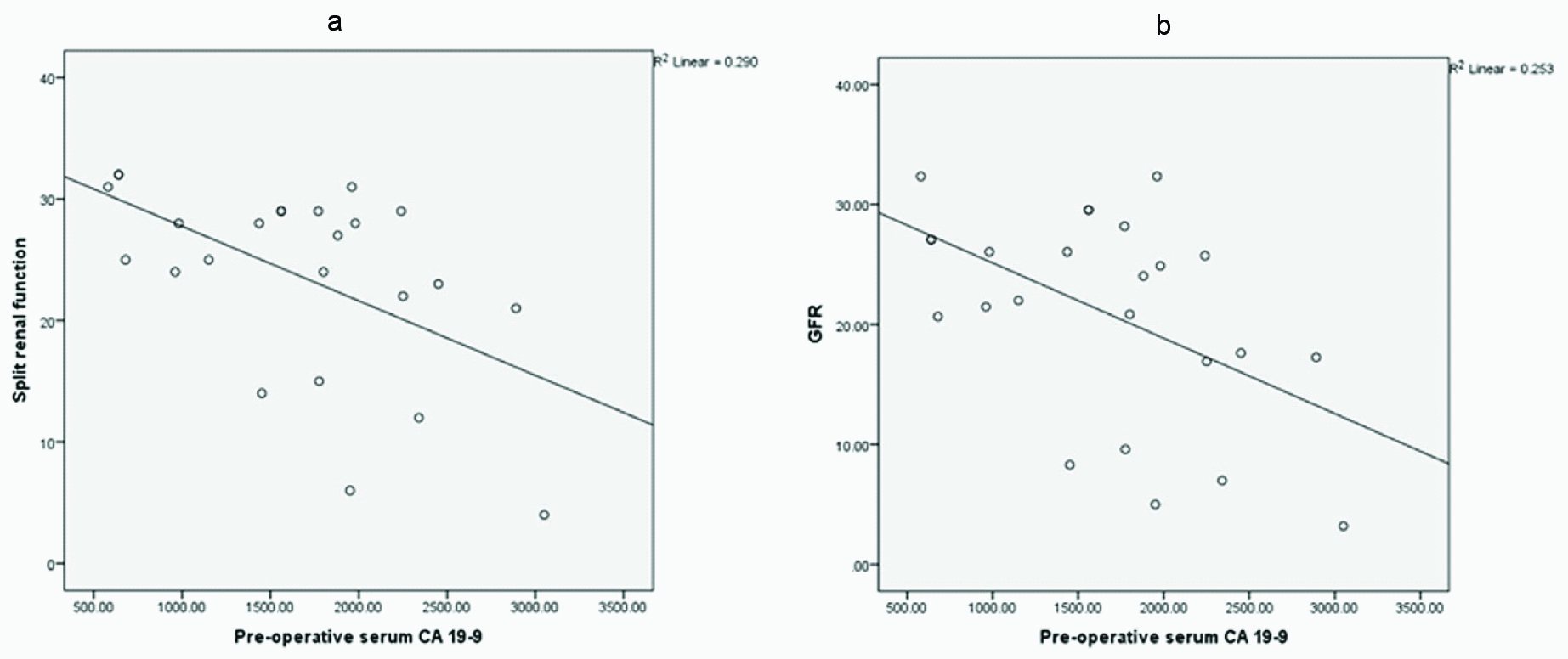
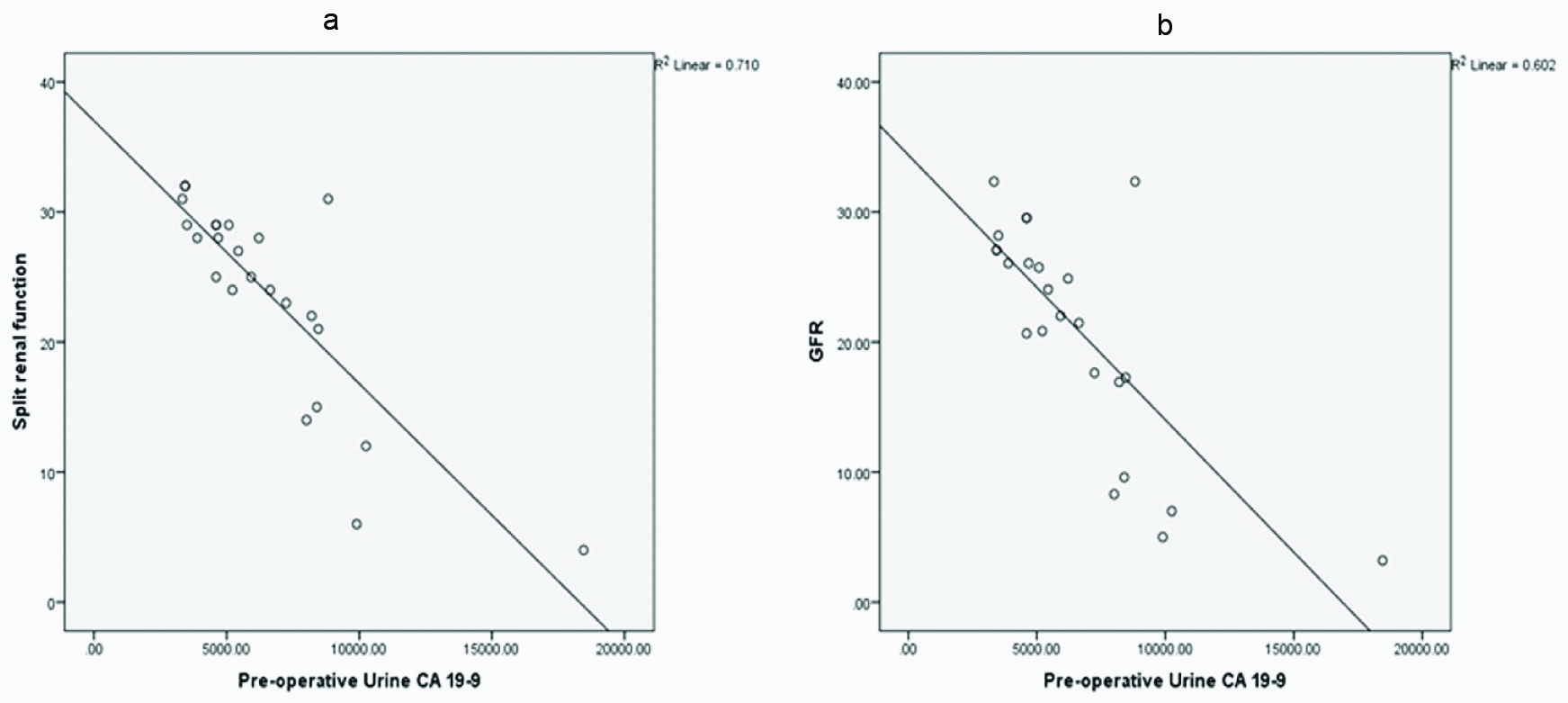
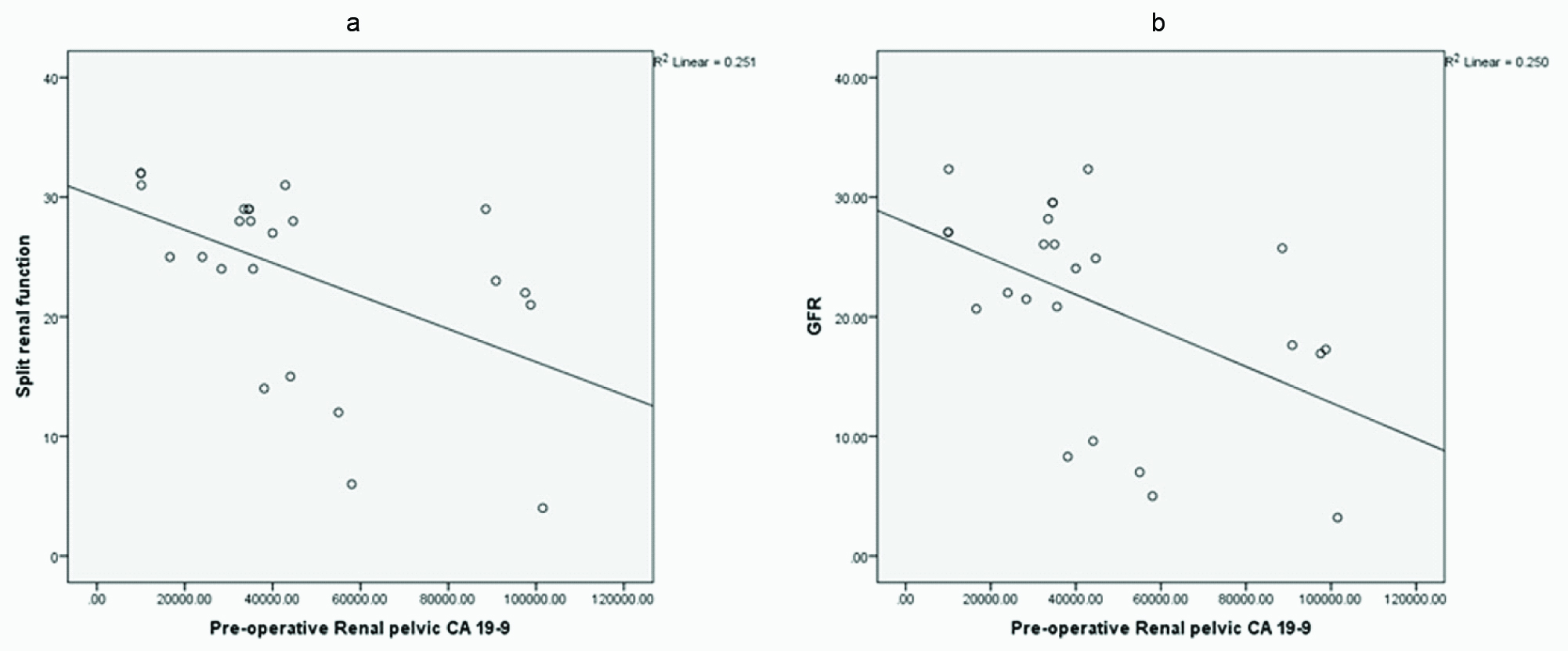
Preoperative split renal function (A) and GFR (B) showed significant inverse correlation with preoperative serum, voided urine and renal pelvic urine CA19-9 [Table/Fig-4,5 and 6]. Strongest correlation was found with urine CA19-9 levels.
A correlation between preoperative serum CA19-9 and initial: a) split renal function (r = -0.538, p <0.007); and b) GFR (r = -0.503, p <0.012).
A correlation between preoperative urine CA19-9 and initial: a) split renal function (r = -0.842, p < 0.000); and b) GFR (r = -0.776, p <0.000).
A correlation between preoperative renal pelvic CA19-9 and initial: a) split renal function (r = -0.501, p < 0.013); and b) GFR (r = -0.500, p < .013).
Initial preoperative GFR and percentage renal function in the reconstructive group was 24.11 ± 3.73 ml/min and 26.69 ± 3.43 % respectively (after excluding 3 cases of eventual nephrectomies). After surgery the values reached 27.58 ± 3.26 ml/min (30.44 ± 3.72 %) and 30.24 ± 3.90 ml/min (33.69 ± 4.61 %) at 3 and 9 months respectively; which was a significant improvement (p < .01, p < 0.00, p<0.01, p < 0.00).
Discussion
The management strategies in GH due to UPJ obstruction is not standardised and many patients end up in eventual nephrectectomy, even after initial reconstructive operations. Crooks et al., Uson et al., Sataa et al., had nephrectomy rate of about 70%, 33% and 30% respectively [2,14,15]. In our study the nephrectomy rate was 33% (including three initial conservative surgery failure cases). Diuretic renogram could often be fallacious in GH [3]. CTU and IVP might show non-visualised unit. The management decision based on these available imaging studies, many a times become difficult. These are also associated with significant radiation exposure. Search for a potential biomarker that will indicate the severity of the disease and help in guiding eventual management and response monitoring seems prudent. Taha et al., reported 100 % sensitivity and specificity of voided urine endothelin 1 for diagnosis of UPJ obstruction in children [6]. Grandaliano et al., described marked change in urinary monocyte chemotactic peptide 1 and epidermal growth factor level after surgical correction of obstructive uropathy [8].
Kajbafzadeh et al., had found urine CA19-9 to be significantly raised in UPJ obstruction cases in paediatric age group; release of obstruction was associated with significant reduction in serum and urinary CA19-9 and improvement in renal function [3]. Similarly, in our study, there was a significant decrease in serum and voided urine CA 19 -9 at 3 months and became normal at 9 months in all the successfully treated patients.
Benign hydronephrosis as a cause of increased CA19-9 expression in renal pelvis was first reported by Ohshio et al., [16]. Although, the exact mechanism is yet to be decoded, the proposed hypothesis states, due to increased inflammation and proliferation of renal pelvic epithelium as well as impairment in the CA19-9 excretion pathway lead to increase in CA19-9 levels [11].
In comparison to serum and intrapelvic CA19-9 concentration voided urine CA19-9 showed much stronger significant inverse correlation with preoperative GFR and split renal function. There was a striking increase in voided and renal pelvic urine CA19-9 levels as compared with serum values, which indicates renal rather than systemic cause of either increased production or decreased degradation. Although, intrapelvic CA19-9 was significantly higher than urine levels, there was a significant correlation between the two, indicating predictive role of preoperative urinary CA19-9 in intrapelvic levels.
The cut-off for voided urinary and serum CA19-9 with 95% CI predicting nephrectomy and pyeloplasty were much higher than the values in paediatric pyeloplasties (serum and urinary CA19-9 were 13.21 U/ml and 30.6 U/ml, respectively) as suggested by Kajbafzadeh et al., but our patient population are different from those cohort and presumably are suffering from more long standing and severe disease [4]. Similar high values are reflected in some case reports also [11]. Three patients had persistently raised urine CA19-9 level in the domain of nephrectomy cut-off value, after conservative surgery. They had decline in GFR and split renal function in follow-up, to underwent nephrectomy eventually. This finding, also support our hypothesis. Even though, by such urinary CA19-9 values we can predict preoperatively the likely surgical intervention the patient will undergo, and avoid unnecessary conservative operations, but the final decision is based on the clinical judgement.
All the patients who had simple nephrectomy, had transperitoneal laparoscopic procedure; which is considered superior to open technique [17]. Laparoscopic reconstructive surgery was avoided for fear of increased intraoperative complications. Nephropexy was done in all cases as an adjunct to open pyeloplasty, as reported by Shah et al., [18]. It tilts the pelvicalyceal system laterally and makes the uretero-pelvic angle close to 180° that helps in dependant drainage. Ureterocalicostomy was done in cases with intrarenal collecting system and when lower pole calyx was the most dependant part [19].
The most relevant parameters in the clinical connotation of this marker were the decrease in serum and urine CA-19-9 levels after successful surgeries. Even though the voided urine CA19-9 concentration at 3 months was significantly lower than the initial level, it was higher than in controls, which eventually became normal at 9 months. Additionally, diuretic renography at 3 and 9 months revealed significant improvement. Further follow-up that will allow us to predict the long-term renal functional status is necessary.
Conclusion
We should recognize that these results were attained in the patients of a rare disorder based on clinical, ultrasound, CTU and DTPA scan evaluations. Thus, further studies in a larger population probably including patients with preoperative GFR 10-20ml/min in all UPJ obstruction cases will consummate the importance of this biomarker in borderline functioning renal units due to UPJ obstruction. The marker will also able to guide the preoperative decision making in those cases.
Voided urine CA 19-9 is a clinically relevant non-invasive marker in adult giant hydronephrosis due to UPJ obstruction. The practical clinical connotation of this marker for diagnosis, treatment and long-term follow-up of these patients are significant. The preoperative values can predict the appropriate surgical decision making. Decrease in urinary CA19-9 level during follow-up can prognosticate superior surgical outcomes and recovery of renal function.
*p< .05 Preoperative values as compared to postoperative values.
‡ Only in group 1.
CA: Carbohydrate antigen, SD: Standard deviation.