Ageing is a biological phenomenon resulting from changes at cellular level to the changes at gross morphological level in all aspects. Gradually, with ageing related, health problems concomitantly accompany and further deteriorate the condition. These may include oral diseases which finally may lead to tooth loss. Loss of teeth may require some form of aesthetics making functional prosthetic treatment necessary for the patient.
Histological and morphological changes of the bony socket and adjacent soft tissue may undergo a series of tissue repair processes after tooth loss. According to histological evidence active bone formation taking place at the bottom of the socket and bone resorption at the edge of the socket are observed around two weeks after tooth extraction; however, the complete fill of the socket with newly formed bone takes around six months time. During this time rapid bone remodeling drops; however, continuous bone resorption may continue at the outer surface of the crestal area of the residual alveolar bone. This results in significant morphologic changes in the bone and its overlying soft tissues over the years [1].
Now-a-days, dental treatments with better aesthetic results and less treatment time are more acceptable by the patient. The prosthetic treatment modalities like removable or fixed partial dentures have risk of various complications including sacrifice of healthy tooth substance. Dental implants have overcome disadvantages of other procedures and emerged as an ideal replacement modality for missing teeth. Inadequate amount of bone for implant placement at functionally and aesthetically most appropriate position is a common problem. Placement of endosseous implants in atrophic ridges is often accompanied by various challenges [1,2].
Various surgical widening techniques have been employed and described for restoration of atrophic ridges, including block grafting, lateral augmentation with or without Guided Bone Regeneration (GBR), onlay grafting and alveolar distraction osteogenesis [2]. These procedures are carried out before or after implant placement to establish at least 1mm bony wall around screw type implants [2]. Although different techniques exist for atrophic ridges, there are chances of need for multiple surgeries which carries surgical risk and postoperative morbidity. Expansion of the existing residual ridge is another method and is referred as Ridge Expansion Osteotomy (REO) [2].
Conventional technique of implant placement includes drilling of the bone which always takes bone away from the site. Often there is a marginal quantity of bone to start with. During the drilling process, there is no practical means to immediately improve adjacent bone quality. In addition, drilling creates heat, which is the main obstacle for osseous integration. To overcome all these obstacles, osteotome technique is in practice which essentially doesn’t produce any heat [2,3].
So, the aim of this study was to evaluate ridge-width gained after ridge expansion procedure, effect of ridge expansion on primary and secondary stability after implant placement by Radio Frequency Analysis (RFA) test and to evaluate radiographic crestal bone loss using digital Intraoral Periapical Radiograph (IOPAR).
Materials and Methods
A preliminary prospective clinical study was conducted on patients who reported during year 2014-2015 to the Department of Oral and Maxillofacial Surgery, Sibar Institute of Dental Sciences, Guntur, Andhra Pradesh, India. A total of 10 patients with inadequate alveolar width and having sufficient alveolar height were included in the study. Sample size was determined based on a previous study [4]. Performance of the 10 implants placed in these 10 patients in the anterior maxilla was evaluated clinically and radiographically over a span of three months.
Ethical clearance was obtained from the Institutional Ethics Committee before the commencement of the study. The subjects for the study were selected on the basis of scientifically pre-defined inclusion and exclusion criteria. Patients who presented with partial edentulous space in anterior maxilla, having a ridge width of 2.0mm to 5.0mm, measured preoperatively, using Cone Beam Computed Tomography (CBCT, between 18 to 60 years of age, co-operative, hygiene conscious, motivated and willing to participate and gave written informed consent and those having adequate vertical height (measured from crest of the ridge to the nasal floor using CBCT, having more than 12mm vertical height) were included in the study. Patients with severely atrophic ridges, those with co-existing vertical defect requiring additional corrective intervention, heavy tobacco users, uncontrolled diabetics, immuno-compromised patients and those who were poorly motivated and unable to keep the follow-up were excluded from the study.
Global Implants (two piece implants, endosseous, thread type) of pure titanium; length range 8mm to 16mm with diameter 3.8mm and 5mm were used for the present study. Ridge Expansion Osteotomes Kit and Mallet (Sirag Surgical Enterprises, Chennai, India) [Table/Fig-1] was used for the expansion procedure. All surgical procedures were performed under strict aseptic conditions and following standard protocols. The patients were initiated on a daily dose of antibiotic (Amoxicillin 20-25mg/kg/day i.e., 1.5gm/day for an average adult of 70kg, one day prior to implant placement and were maintained on it for the next five days), Tab. Aceclofenac 100mg with Paracetamol 500mg (thrice a day) was given to the patients an hour before implant placement and continued for next five days along with Amoxicillin. The baseline clinical examination consisted of a thorough medical and dental history, general and oral health status, assessment of future implant site. The available vertical, mesio-distal and labio-lingual bone dimension was determined by measurements from CBCT and ridge mapping was used to assess labio-lingual ridge width using the ridge mapping calliper. Local anesthesia was administered (Lignocaine HCL + 2% Adrenaline 1:80000) following which an incision was made buccal to the ridge crest to provide more attached tissue along the facial aspect of the implant. During ridge expansion the micro-fracture of cortical plate possibility cannot be overlooked, as the cancellous bone will be compressed to both the buccal and palatal walls. The buccal cortical plate is considered to be more vulnerable for expansion forces as it is not having adequate bone support like palatal side, so it is better to have a good amount of soft tissue which makes the difference post operatively by providing adequate coverage. Also, in undue cases of fracture it acts as pedicle for the buccal cortical plate. Minimal mucoperiosteal flap reflection was performed to expose only the ridge crest. If necessary, the peak of the thin ridge was slightly reduced with a ronguer or osteoplasty bur. The mid-crestal osteotomy of the atrophied ridge was done using round tungsten carbide bur. The ridge expansion began over the prepared initial osteotomy site such that it bisected the ridge crest and expanded the cortical plates [Table/Fig-2,3,4,5 and 6].


Exposure of knife edge ridge.

Ridge width measurement before expansion using bone calliper.

Osteotome in place for expansion.

Ridge width measurement after expansion.

The handle of the osteotome was kept parallel to the palatal or lingual cortex and advanced through the bone using a mallet. This path resulted in a more facial angulation of the handle than the ideal long axis of the teeth. After the osteotome was tapped to depth, it was gently removed with a back and forth motion, parallel to the cut, to prevent alveolar bone fracture. The length of the osteotomy was extended beyond the planned implant sites along the edentulous area so as to allow the cortical plates to expand during osteotomy preparation and implant insertion. Progressively, wider osteotomes were utilized to smoothly expand the atrophic maxillary ridge.
After sufficient expansion (which should be larger than the size of the implant; as a thumb rule the implant should have minimum 1.5mm of surrounding bone, so required implant size plays an important role in the ridge expansion) of the ridge was achieved, the endosteal implants were introduced into the prepared site and evaluated for primary stability using the resonance frequency analyzer and torque wrench, a minimum Implant Stability Quotient (ISQ) of 50 was considered to include in the study implants with torque more than 25 Ncm. The reflected mucoperiosteal flaps were sutured using black braided silk suture material. The patient was advised Chlorhexidine (0.12%) mouth rinse twice daily for two weeks post-operatively. Suture removal was done seven days post-operatively.
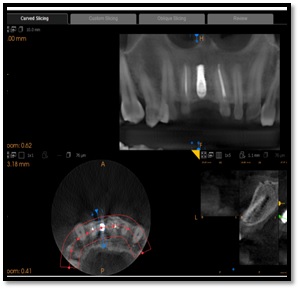
The patients were followed-up at the 7th post-operative day, 3rd week and 3rd month. The patients were evaluated for implant stability and crestal bone loss at 3rd week and 3rd month post-operatively using CBCT [Table/Fig-7,8,9,10,11 and 12]. Functional rehabilitation of the implants were done after three months post-operatively. The results were scientifically recorded, data collected, collated, entered and analyzed using paired t-test.
Measurement of primary implant stability.

Placement of healing cap.

Measurement of secondary implant stability.


Pre operative CBCT showing ridge width.
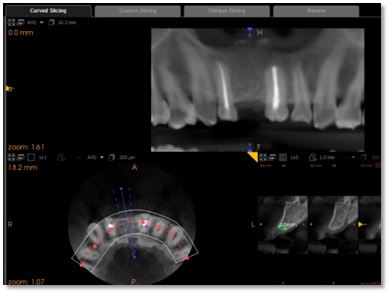
Post operative ridge width showing ridge width.
Results
The implant stability gradually increased over the study period on all the aspects. [Table/Fig-13] shows the data of patient, stability in ISQ and ridge expansion pre, postoperative measurements. Pre-operative ridge width mean was 3.94 ± 0.33 and after ridge expansion ridge width was 7.39 ± 0.66. The difference of mean value was 3.45 which was highly significant (p-value <0.001) [Table/Fig-13]. [Table/Fig-14] reveals crestal bone loss at different time intervals during the study. In comparison of crestal bone loss on the mesial and distal aspect in a time period of three weeks and three months after implant placement, mesial bone loss after three weeks was 0.26 and after three months it was 0.50 which was significant (p-value=0.033). Also, on the distal aspect crestal bone loss after three weeks was 0.34 and after three months mean it was 0.58 which was significant (p-value=0.008) [Table/Fig-14].
Showing data of patient, stability in ISQ (Implant stability quotient) and ridge expansion pre, post-op measurements.
| Patient | Age (years) | Sex | Implant stability (ISQ) values on different aspects | Ridge width |
|---|
| Labial Pre-op | Labial Post-op | Palatal Pre-op | Palatal Post-op | Mesial Pre-op | Mesial Post-op | Distal Pre-op | Distal Post-op | Occlusal Preop | Occlusal Post-op | Pre-op | Post-op |
|---|
| 1 | 26 | M | 70.00 | 79.00 | 72.00 | 80.00 | 73.00 | 78.00 | 72.00 | 80.00 | 73.00 | 81.00 | 4.00 | 7.90 |
| 2 | 23 | M | 68.00 | 80.00 | 72.00 | 79.00 | 65.00 | 70.00 | 60.00 | 75.00 | 70.00 | 79.00 | 4.40 | 7.80 |
| 3 | 23 | M | 71.00 | 80.00 | 70.00 | 81.00 | 70.00 | 81.00 | 68.00 | 79.00 | 72.00 | 75.00 | 3.90 | 8.00 |
| 4 | 20 | F | 70.00 | 72.00 | 63.00 | 74.00 | 65.00 | 76.00 | 64.00 | 71.00 | 66.00 | 70.00 | 3.50 | 6.70 |
| 5 | 23 | M | 65.00 | 71.00 | 68.00 | 71.00 | 69.00 | 73.00 | 70.00 | 70.00 | 67.00 | 70.00 | 3.30 | 6.00 |
| 6 | 19 | M | 71.00 | 78.00 | 72.00 | 78.00 | 76.00 | 76.00 | 75.00 | 74.00 | 76.00 | 76.00 | 4.20 | 7.80 |
| 7 | 25 | M | 71.00 | 78.00 | 72.00 | 76.00 | 74.00 | 80.00 | 76.00 | 72.00 | 69.00 | 80.00 | 4.00 | 7.00 |
| 8 | 25 | M | 72.00 | 76.00 | 72.00 | 78.00 | 69.00 | 78.00 | 70.00 | 79.00 | 76.00 | 78.00 | 4.10 | 7.20 |
| 9 | 38 | M | 68.00 | 79.00 | 71.00 | 78.00 | 76.00 | 81.00 | 78.00 | 78.00 | 71.00 | 81.00 | 4.20 | 8.00 |
| 10 | 24 | M | 71.00 | 72.00 | 68.00 | 76.00 | 76.00 | 78.00 | 72.00 | 78.00 | 76.00 | 76.00 | 3.80 | 7.50 |
| MEAN | 24.60 | | 69.70 | 76.50 | 70.00 | 77.10 | 71.30 | 77.10 | 70.50 | 75.60 | 71.60 | 76.60 | 3.94 | 7.39 |
| SD | 1.641 | | 0.667 | 1.118 | 0.93 | 0.93 | 1.36 | 1.11 | 1.73 | 1.16 | 1.16 | 1.28 | 0.105 | 0.209 |
| RANGE | 19-38 | | 65-72 | 71-80 | 63-72 | 71-81 | 65-76 | 70-81 | 60-78 | 70-80 | 66-76 | 70-81 | 3.30-4.40 | 6-8 |
| p-value | <0.001 (HS) | <0.001 (HS) | <0.001 (HS) | <0.001 (HS) | <0.001 (HS) | <0.001 (HS) |
Showing crestal bone loss at the mesial and distal aspects at different time intervals.
| Patient | Bone loss on Mesial side | Bone loss on Distal side |
|---|
| At 3 Weeks | At 3 Months | At 3 Weeks | At 3 Months |
|---|
| 1 | 0.0 | 0.5 | 0.0 | 0.5 |
| 2 | 0.4 | 0.5 | 0.6 | 0.7 |
| 3 | 0.3 | 0.5 | 0.5 | 0.7 |
| 4 | 0.5 | 0.6 | 0.5 | 0.7 |
| 5 | 0.5 | 1.5 | 0.8 | 1.5 |
| 6 | 0.0 | 0.2 | 0.0 | 0.3 |
| 7 | 0.0 | 0.0 | 0.0 | 0.0 |
| 8 | 0.0 | 0.0 | 0.0 | 0.0 |
| 9 | 0.4 | 0.5 | 0.5 | 0.6 |
| 10 | 0.5 | 0.7 | 0.5 | 0.8 |
| MEAN | 0.26 | 0.50 | 0.34 | 0.58 |
| SD | 0.073 | 0.134 | 0.096 | 1.137 |
| Range | 0-0.5 | 0.0-1.50 | 0.0-0.8 | 0.0-1.5 |
| p-value | 0.033 (S) | 0.008 (S) |
Discussion
Dental implants have now become an integral part of various treatment modalities. Availability of adequate amount of bone in terms of vertical as well as horizontal dimension is the first requirement for a successful implant therapy, but it becomes difficult to place the implant when there is inadequate amount of bone [5].
Morphological and histological changes in the alveolar process are teeth-dependent processes that develops in conjunction with the eruption of the teeth. Previous clinical and cephalometric studies have revealed atrophy and dimensional reduction of the alveolar ridges in both the horizontal and vertical axis after all teeth are removed [6,7]. The greatest reduction occurs in the first 6-12 months [7]. Bone loss occurs in the anterior mandible and the maxilla mainly at the labial side.
Many of recent investigations have inspected the resorption pattern and evaluated the changes that occur in the alveolar processes following tooth extractions by various means including study cast measurements, subtraction radiography and direct measurements of the ridge at surgical re-entry [8–10]. It was reported that in the first three months after tooth extraction around two thirds of bone loss occurs, signifying that maximum alteration in dimension of alveolar ridge takes place within the first three months post extraction and the reported corresponding vertical bone loss is around 0.9mm to 3.25mm. [8–10].
Loss of alveolar bone may also occur prior to tooth extraction because of advanced periodontal disease, periapical pathology, or trauma to teeth and bone or during tooth extraction procedure, periodontal health of the neighboring teeth and periodontal biotype (shape and thickness of soft tissue) the width of the labial cortical plate may also result in bone loss and affect the resorption process [11]. Osteoporosis, renal disease and endocrine disorders are some of the systemic conditions that may speed up bone loss by varying normal bone physiology and metabolism [6] Moreover, habits, including smoking and bruxism have been considered as contributing factors in increased bone loss. All the above stated reasons may result in resorption over a wide area of labial surface leading to marked narrowing of the labio-lingual diameter of the crest of the ridge, thus, forming a knife edge ridge, which is particularly problematic for implant placement owing to insufficient ridge width. Alveolar bone width should be sufficient to provide a minimum 1mm bone width around the implant [2]. When the alveolar ridge is narrower than the optimally planned implant diameter, reconstruction of the ridge before implant placement is mandatory. Various techniques have been mentioned in the published literature for reconstruction of the atrophic ridges so as to increase the existing bone volume like bone grafting, guided bone regeneration and distraction osteogenesis, however, these techniques suffer from limitations like being invasive and increase morbidity, moreover resorption of grafting materials, membrane collapse, exposure to infection and delaying of implant installation for grafting maturation are few other constraints associated with these techniques [1,2].
Ridge expansion of the remaining residual ridge is an additional method to prepare the atrophic ridges for implant placement. This approach has been referred to as ridge expansion, ridge splitting, bone spreading and was developed by Tatum in 1986 [12], but was then reintroduced in 1990 by Bruschi and Scipioni [13]. The method involves the splitting of the vestibular and buccal cortical plates [2,3] and further expanding the gap with Summers’s osteotomes [2,3]. A minimum of 3mm of bone width, including at least 1mm of cancellous bone is required to place an osteotome between cortical plates and accordingly expand the cortical bony plates.
Summers, Scipioni et al., Hahn J [2,3,13,14] and many others got successful results following this technique for narrow ridges. They showed ridge expansion technique having advantages of simultaneous implant placement, lesser overall cost, no need of barrier membranes or bone graft materials and no morbidity related to second site. So in the present study, ridge expansion was carried out using the osteotome technique owing to its advantages documented in literature.
In the present study effect of ridge expansion of narrow partially edentulous ridges on ridge width, implant stability and crestal bone loss was evaluated. The first parameter assessed was the gain in the ridge width which was measured using the ridge mapping caliper. The use of ridge mapping caliper to assess bone levels for implant placement in anterior maxilla, avoids some of the problems associated with CT scanning [15,16].
In present study ridge expansion using osteotomes resulted in significant gain in ridge width after three post operative months (3.94 ± 0.33 pre-operatively to 7.39 ± 0.66 post-operatively) (p-value <0.001) [Table/Fig-13]. Similar to the present study, Roni Kolerman, et al., conducted a study on long-term outcome of ridge expansion using the osteotome procedure followed by implant placement in combination with guided bone regeneration in patients with atrophic maxillary alveolar ridges and reported significant increase in the ridge width over the study period (pre-op ridge width values increased significantly from 3.73±0.67 to 7.19 ± 0.80) [4].
Demarosi F et al., conducted a study on localized maxillary ridge expansion with simultaneous implant placement in adult patients with atrophy of the upper maxilla, 26 ridge expansion surgeries were carried out and 36 implants were placed. The ridge width increased from an initial range of 2.5mm-4.5mm to 6mm-7.5mm at the end of the procedure [17]. That is the gain in alveolar ridge width ranged from 3mm to 5 mm. Measuring primary stability and secondary stability was the second parameter assessed in this study. Stability of the implant was measured in ISQ using RFA device. Primary stability of an implant comes from mechanical engagement with cortical bone. It is affected by the quantity and quality of bone that the implant is inserted into, surgical procedure, length, diameter, and form of the implant [18]. Secondary stability is a biological phenomenon, that is the result of healing that takes place around the implant, (osseointegration) [18].
There is no consensus regarding which method to use when measuring implant stability. One commonly used, non-invasive method is resonance frequency analysis, which evaluates the stiffness of the bone-implant complex. The result is given as implant stability quotient, ISQ [Table/Fig-13]. A dip in ISQ is usually seen during the early healing phase after osseointegration and is related to the shift between primary and secondary stability. The results of the present study revealed that the implant stability increased gradually over the study period and the results were statistically significant over 3 months [Table/Fig-13].
Padmanabhan TV et al., conducted a study to evaluate the crestal bone loss and effect on primary stability exhibited by the bone around early non-functionally loaded implants placed with conventional implant placement technique and with Summer’s osteotome technique and demonstrated a significantly higher stability of implants in the conventional group than in osteotome group on the day of surgery [19]. However, after six months of implant placement, no statistically significant difference in stability was found between both groups (p = 0.076). A significantly less crestal bone loss was reported with conventional group. Thus, the authors concluded that this technique can be utilized for knife edge ridges and should not be substituted for the conventional procedure for implant placement. Kreissel P, in a similar study assessing the implant stability in expanded ridges, reported that bony micro-architecture had no consequence on implant stability, initial bone density, presence of a cortical layer. They also reported that the application of the screw-shaped spreaders significantly increased ISQ values over the study period [20].
Mesial and distal crestal bone loss in a time period of three weeks and three months after implant placement was the 3rd parameter assessed in present study for which Digital IOPAR and DIGORA was utilized similar to Padmanabhan TV et al., [19]. Kolerman R et al., conducted a similar study to evaluate the outcome of a ridge expansion osteotome procedure and implant placement combined with guided bone regeneration in patients with narrow maxillary alveolar ridges and reported that over a mean follow-up period of 52.4 months the survival rate of 116 implants was found to be 100% with statistically significant gain in ridge width of 3.5 ± 0.93 (p < 0.0001) and significant enlargement of the buccal bone was about 1.91 ± 0.6 (p < 0.0001) [4]. The vertical mesial and distal bone loss reported ranged from 0.3mm to 4.2 mm, and 0.4mm to 4.5 mm respectively. Padmanabhan TV et al., conducted a study on crestal bone loss in implant placement done by using osteotome technique and reported a mean bone loss of 1.19 after placement of 10 implants in the maxillary anterior region of five patients [19]. Comparison of marginal bone loss on two aspects, i.e., mesial and distal in a time period of three weeks and three months after implant placement revealed that the distal aspect bone loss after three weeks was 0.34±0.31 and after three months was 0.58±0.43 which was significant for distal bone loss. The lowest ridge expansion width found to be was 2.70mm because it was a narrow ridge and with poor bone quality and the highest ridge width gain was 4.10mm. Least primary stability value was 60 ISQ because of buccal bone fracture. Secondary stability achieved was 70 ISQ with maximum of 81 ISQ which is indication of success of an implant. In comparison of vertical bone loss in mesial and distal side, greater than 1.5 mm bone loss was observed in one case, whereas, the bone loss in the remaining cases was below 0.8mm.
Kolerman R reported an average gain in ridge width of about 3.5±0.93 and bone loss 1.81±1.07 on the mesial side, whereas it was 1.74±1.12 on the distal side [4]. Similarly, in present study average ridge width gain was 3.45±0.33 which was significant and bone loss on mesial side was 0.24 ±0.20, whereas, on the distal side it was 0.24±0.12 and the results were significant. According to Padmanadhan TV et al., primary stability mean value was 59.60 ISQ and secondary stability was 61.50 ISQ which is similar to the results of the present study [19]. In the present study, complications included buccal bone fracture in two of the patients and were not considered in the study protocol. The fractures might have attributed to the technique of removal osteotome after tapping. If the removal of osteotome is inadvertent or more buccal, then the chances of buccal cortical plate fracture are increased. In our two of the cases wrong direction while pulling the osteotome lead to the fracture in which the placement of implant was considered in the later stage. Only single patient complained about the pain during the procedure due to inadequate local anesthesia given to patient. Also, one patient complained about redness and pain at implant site after one month due to gingival inflammation. Three patients were not able to come in time for follow-up. These patient data were not considered for the statistical analysis because they were lost to follow-up. To overcome all these problems further studies with larger sample size and comparative control groups must be carried out with an extended follow up period to substantiate the results of the present preliminary study.
Limitation
The study sample size was smaller. The duration of follow-up is less. The single operator did all procedures. The study warrants long term follow-up with multi center and multi-operators. The fracture of buccal plate is one of the limitation. It requires training to handle the osteotome. The study warrants long term multi-center blind studies. The case selection is critical factor for the success of implant . The inadvertent force during removal of osteotome may lead to fracture of buccal cortical plate.
Conclusion
Horizontal expansion in atrophic alveolar ridge without any complex treatment can be performed using Ridge expansion technique. This technique is helpful and patient friendly as it decreases the rehabilitation time and improves quality of overall bone support with adequate implant stability achieved at three months post operative period.