Medical undergraduate students, evolving from adolescence to adulthood, are faced with academic and clinical challenges every day. This might lead to change in life style and thereby make them susceptible to hypertension. Supporting this, our own study on medical students and many other studies have reported high incidence of pre-hypertension in medical students [1–3]. Prehypertension is an early indicator of clinical hypertension and subsequently of the Cardiovascular Diseases (CVD) [4]. CVD is the major cause of death worldwide [5].
Thus, the Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (BP) defined BP levels of 120 to 139/80 to 89 mm Hg as prehypertension based on the evidence of a modest increase in cardiovascular risk among individuals with such levels [4].
Accordingly, it could be hypothesized that in many individuals, collective effect of risk factors and extent of modifiable risk factors may determine BP; but in certain individuals, a non -modifiable risk factor alone may affect BP adversely in-spite of BP lowering programmes.
Currently, lacunae persist in establishing whether hypertension manifests owing to sole non-modifiable risk factor or while several risk factors cluster. Therefore this pilot study was undertaken. This study model incorporated a scoring system in which each risk factor was assigned a score and summed up for every individual. Association between summed-up score and BP was assessed. Also, to ascertain if any single dominant factor determines prehypertension, each characteristic of prehypertensives was compared with normotensives. The same population was also studied to evaluate the relation between Hb and pre-hypertension.
Materials and Methods
This was a cross-sectional study done in 84 apparently healthy undergraduate medical students. Study included both males and females aged between 18-23 years and pursuing MBBS in a medical college in Mangaluru, Karnataka, India. This study was done after obtaining the Institutional Ethics Committee approval and informed consent from the study participants. This study of one month duration during June 2014 (By assuming 0.5 correlation, with 95% confidence level and 90% power, a total of 75 subjects were to be selected. However, the study included 84 participants).
Inclusion criteria: Students with at least one known risk factor and consenting to participate were only included in the study.
Exclusion criteria: Students who were chronic smokers, alcoholic and known cases of diabetes, dyslipidemia or on any medication known to affect BP were excluded.
Study protocol
All the study procedures were carried out between 4-6 pm in all the study subjects. Prehypertension was defined as BP levels of 120 to 139/80 to 89 mm Hg [4]. General obesity was considered if the BMI > 23.33 kg/m2. For abdominal obesity two cut offs were considered: Level one -if the waist circumference (WC) was 78cm or more for males; 72cm or more for females. Level two-if the WC was 90 cm or more for males and 80 cm or more for females [12]. Sleep quality was assessed as per the guidelines provided. The Pittsburgh Sleep Quality Index’ by Buysse DJ et al., [13]. Perceived stress was defined as per the guidelines described in ‘Perceived Stress Scale’ by Sheldon Cohen [14]. The diet pattern was assessed by a questionnaire based on Dietetics [15]. Severity of risk factors was assessed based on collective scoring system (method followed is described subsequently).
Personal interview: The basic details of the participants (name, age, sex), details regarding the family history of CVD and physical activity were taken. They were asked to fill the required questionnaire on sleep pattern [13,16], perceived stress [17] and nutritional status [15].
Estimation of BMI: Height was estimated by making the subject lean against the wall, standing straight, barefoot and marking with a pencil; the distance between the pencil mark and flat ground was measured using a standard measuring tape in cm. Weight was measured using a weighing machine (in kg) while the subject stood on it barefoot and straight. BMI was calculated as weight in kg divided by square of height in meters.
Measurement of waist circumference: At the level of the umbilicus in expiratory position with a standard measuring tape.
Measurement of BP: Both SBP and DBP was measured in the right arm in the sitting position with the help of digital BP machine.
Collective scoring of risk factors: Since a study tool to assess risk factors is available only for CVD [18] but not for hypertension, each parameter was assigned a score considering the occurrence and severity as presented in [Table/Fig-1].
Pattern of scoring of risk factor for hypertension.
| Parameters | Description | Scores allotted |
|---|
| Gender | Female | 0 |
| Male | 1 |
| Family history of CVD | Without | 0 |
| With | 1 |
| Body Mass Index(kg/m2) | < 23 | 0 |
| 23-24.9 | 1 |
| 25 or >25 | 2 |
| Waist Circumference (cm) | Males | Below 78 | 0 |
| 78–89 | 1 |
| 90 or more | 2 |
| Females | Below 72 | 0 |
| 72–79 | 1 |
| 80 or above | 2 |
| Diet questionnaire score | 14 | 0 |
| 15–28 | 1 |
| 29–42 | 2 |
| 43–56 | 3 |
| Sedentary life/Exercise | Taking part in structured exercise programme- sports / yoga/brisk walk regularly at least from the past one year | 0 |
| Sedentary life | 1 |
| Pittsburg SleepQuality Index (PSQI) | <3 | 0 |
| between 3 to 5 | 1 |
| > 5 | 2 |
| Cohen perceived stress score | <13 | 0 |
| 13–19 | 1 |
| 20 or more | 2 |
Statistical Analysis
Unpaired t-test was applied to unpaired data of independent observations made in two separate groups. Whenever the standard deviation between the groups was not comparable non-parametric equivalent, Mann-Whitney ‘U’ test was applied. Chi-square test was applied when the data were in frequency. Pearson correlation coefficient was applied to measure association of continuous variables. The extent or degree of relationship between two sets of figures was measured in terms of correlation coefficient (r). The level of significance was measured by two-tailed test. The various analyses were performed using SPSS version 15.0. Statistical significance was taken to be a p-value <0.05.
Results
Out of the 94 students who were approached, 87 turned up for the study. Among them, three were chronic smokers and hence excluded from the study. The data on baseline characteristics of 84 subjects studied is presented in [Table/Fig-2]. Continuous variables are presented as mean ± SD. Categorical values are presented as whole number and in percentage in parenthesis.
Baseline characteristics of study subjects.
| Variables | Mean ± SD |
|---|
| Mean age (years) | 19.69 ± 0.878 |
| Male/female ratio | 40 (48%) /44 (52%) |
| SBP (mm Hg) | 118.20 ±11.89 |
| DBP (mm Hg) | 72.21 ±8.09 |
| Body Mass Index(kg/m2) | 23.12 ±4.44 |
| Waist Circumference(cm) | 83.12 ±12.34 |
| Diet questionnaire score | 32.60 ±5.88 |
| Pittsburg sleep quality index (PSQI) | 4.89 ±2.74 |
| Cohen perceived stress score (PSS) | 19.98 ±5.69 |
| Haemoglobin (g/dl) | 13.29 ± 6.69 |
| Pulse rate (beats/minute) | 83.85 ±12.18 |
| Respiratory Rate (cycles/minute) | 17.85±3.06 |
This study subjects were divided into two subgroups, namely prehypertensives and noromotensives based on systolic and diastolic blood pressure independently according to JNC criteria [4]. Data was analysed of these groups in relation to total risk factor scores and individual risk factors of high blood pressure separately.
Association Between Total Risk Factor Scores and Blood Pressure
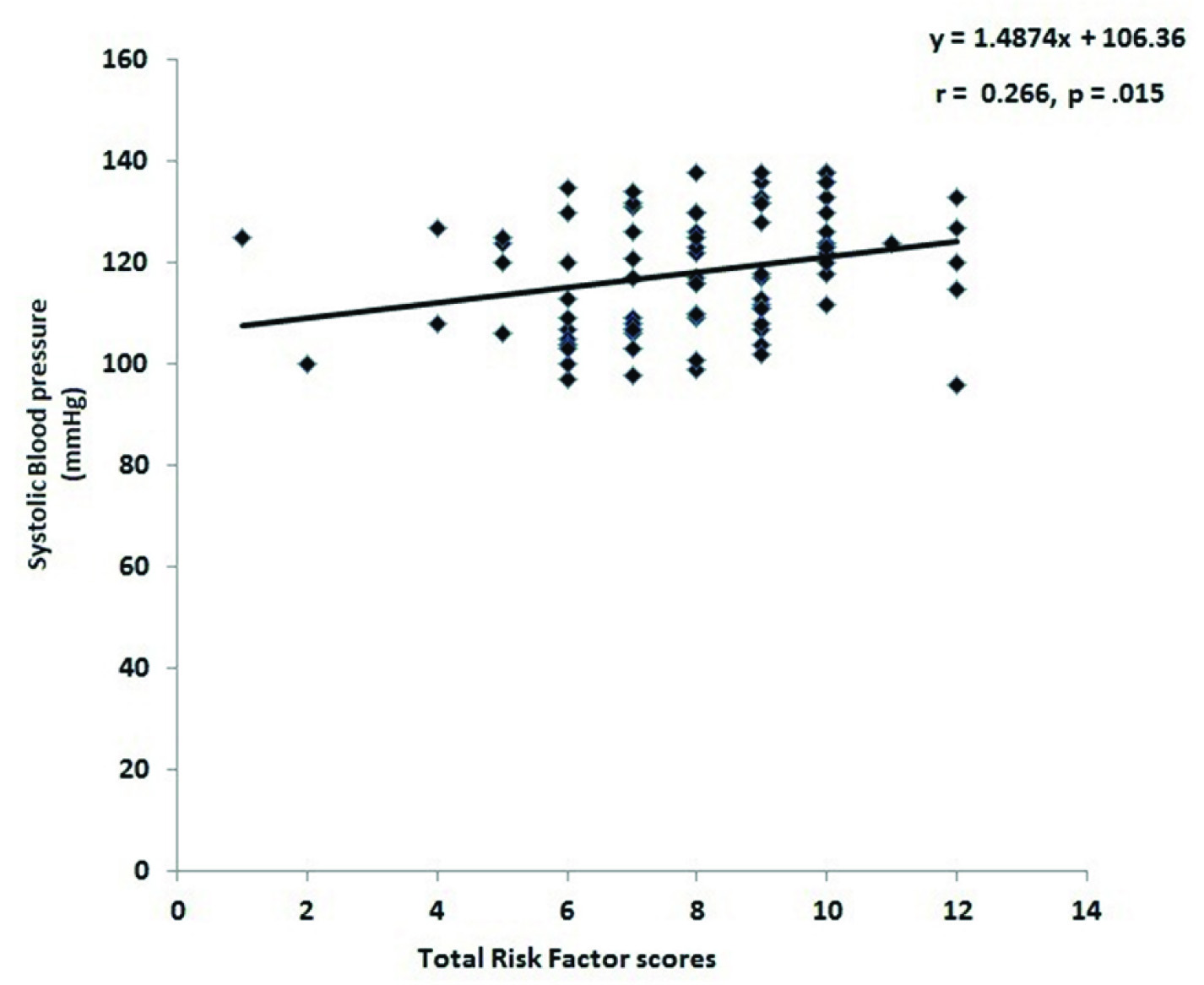
Data collected on risk factors for high blood pressure were scored appropriately and added for each individual. The collective risk factors scores of blood pressure of systolic prehypertensive group was significantly higher compared to normotensive group (8.33±2.29 vs. 7.59±1.90; Mann-Whitney U statistic 655.50, p=0.04). There was significant positive correlation between collective blood pressure risk factors scores and systolic blood pressure (r = 0.26, p = 0.015, [Table/Fig-3]). There was no significant difference in collective blood pressure risk factor scores of diastolic prehypertensives compared to normotensive group (8.5± 2.52 vs. 7.79± 1.97; Mann-Whitney U statistic= 472.50, p=0.079). There was no significant correlation between collective blood pressure risk factors scores and diastolic blood pressure (r = 0.18, p = 0.098).
Correlation between total risk factor scores and systolic blood pressure in study subjects.
Y= 1.4874x+106.36; r= 0.266; p = 0.015, where y = systolic blood pressure (mmHg) and x = total risk factor scores.
Comparison of Individual Risk Factors Between Prehypertensive and Normotensive Groups
Data collected on risk factors of hypertension was individually compared between normotensives and prehypertensives (systolic and diastolic prehypertensives with normotensives separately). Among the risk factors, data on gender, family history of CVD and subjects leading sedentary life are presented in frequency. Data on BMI, WC, Diet sleep quality index and perceived stress score is presented as mean ± SD.
Comparison of Frequency of Male Gender, Subjects with Family History of CVD and Leading Sedentary Life Between Prehypertensives and Normotensives
Frequency of males with systolic prehypertension was significantly higher compared to females (n = 28 (70%) vs. 14 (31.8%), Chi-square=12.28, p<0.0001). Frequency of male subjects with diastolic prehypertension was significantly higher compared to female subjects (n = 14 (35.0%) vs. n = 6 (13.6%) Chi-square=5.271, p = 0.022). Number of subjects with family history of CVD in systolic pre-hypertensive group was not significantly different compared to normotensive group (n = 23 (54.8%) vs. n = 19 (45.2%), Chi-square = 0.762, p = 0.383). Number of subjects with family history of CVD in diastolic prehypertensive group was not significantly different compared to normotensive group (n = 10 (23.8%) vs. 10 (23.8%). Number of subjects not doing exercise in systolic pre-hypertensive group was not significantly different compared to normotensive group (n =24 (57.14%) vs. n = 30 (71.42%), Chi-square =1.868, p = 0.172). Number of subjects not doing exercise in diastolic prehypertensive group was not significantly different compared to normotensive group (n = 16 (29.6%) vs. 4 (13.3%), Chi-square = 2.823, p = 0.09).
Comparison of Individual Risk Factors (continuous variables) Between Prehypertensives and Normotensives
Data on comparison of BMI, waist circumference, PSQI score, diet score and perceived stress score between systolic prehypertensive and normotensive groups are presented as mean ± SD in [Table/Fig-4] and on diastolic prehypertensives is presented in [Table/Fig-5]. BMI and waist circumference of systolic prehypertensives was significantly higher compared to normotensives (p <0.001, < 0.0001 respectively) [Table/Fig-4].
Comparison of individual risk factors and total risk factor score between normotensives and systalicprehypertensives (values are mean± SD)
| Parameters | SystolicPrehypertensives(n =42) | Normotensives(n = 42) | t-value | p-value |
|---|
| BMI(kg/m2) | 24.64 ± 4.45 | 21.59 ± 3.90 | 3.342 | 0.001 |
| WC(cm) | 88.66±12.46 | 77.58± 9.48 | 4.586 | < 0.0001 |
| Diet score | 31.86± 6.19 | 33.33± 5.51 | 1.153 | 0.252 |
| PSQI | 4.40± 2.77 | 5.38± 2.64 | 1.651 | 0.102 |
| PSS | 19.35± 6.50 | 20.59± 4.74 | 0.997 | 0.322 |
| Total risk score | 8.33± 2.29 | 7.59± 1.90 | 655.50* | 0.042 |
*Mann-Whitney U-statistic.
Comparison of individual risk factors and total risk factor score between normotensives and diastolic prehypertensives (values are mean± SD)
| Parameters | DiastolicPrehypertensives(n = 20) | Normotensives(n = 64) | t | p-value |
|---|
| BMI(kg/m2) | 25.73 ± 4.77 | 22.30 ± 4.04 | 3.169 | 0.002 |
| WC(cm) | 91.3±13.87 | 80.57± 10.71 | 3.636 | < 0.0001 |
| Diet | 30.45± 6.71 | 33.27± 5.48 | 1.89 | 0.060 |
| PSQI | 3.40 ± 2.18 | 5.35 ± 2.73 | 2.918 | 0.005 |
| PSS | 20.50± 6.84 | 19.81± 5.33 | 0.469 | 0.640 |
| Total risk score | 8.5± 2.52 | 7.79± 1.97 | 472.50* | 0.079 |
*Mann-Whitney U-statistic.
There was no significant difference in PSQI score, diet score, and perceived stress score between systolic prehypertensive group and normotensive groups [Table/Fig-4]. BMI and waist circumference of diastolic prehypertensives was significantly higher compared to normotensive group (p = 0.002, < 0.0001). PSQI score was significantly lower in diastolic prehypertensive group compared to normotensive group (p = 0.005) [Table/Fig-5]. Diet score and PSS did not differ significantly between diastolic prehypertensive and normotensive groups [Table/Fig-5].
Comparison of Cardiovascular Risk Factors in Male and Female Prehypertensives with Normotensives
The study parameters that showed significant difference between prehypertensive group and normotensive group alone was further analysed separately in male and female study subjects.
In males, BMI of prehypertensives was significantly higher compared to normotensives (24.01± 3.72 (n =13), 20.61± 3.57 (n =28), t =2.67, p = 0.01); PSQI score was significantly lower in prehypertensives compared to normotensives (4.07±2.26, 6.5±3.17, t = 2.75, p = 0.009). There was no significant difference in waist circumference between prehypertensives and normotensives (88.89 ± 12.34, 81.79± 10.89, t= 1.72, p = 0.09).
In females, BMI and waist circumference was significantly higher in prehypertensives compared to normotensives (mean ± SD = 25.90 ±5.59 (n = 14), 21.97 ±4.02 (n=30), Mann-Whitney U-statistic= 105, p = 0.008; mean ± SD = 88.21± 13.15, 75.9 ±8.47, Mann-Whitney U-statistic = 85.50, p = 0.0018 respectively). There was no significant difference in PSQI score between prehypertensives and normotensives (mean ±SD = 5.07± 3.6, 4.93± 2.30 209, Mann-Whitney U-statistic = 50, p = 0.99)
Discussion
High incidence of prehypertension is reported in young adults [1–3]. Therefore, this pilot study investigated the influence of known risk factors of hypertension on blood pressure in apparently healthy young adults. We also investigated to find any significant association between collective effects of known risk factors of hypertension on blood pressure in this student population.
In the present study, there was a significant positive correlation between total risk factor score and SBP. This finding suggests that the clustering of risk factors may contribute to the elevation of blood pressure. Though the total score included several factors, the major contributing factors were male gender, BMI and waist circumference. Thus it appears obesity and male gender are the major risk factors of prehypertension in young apparently healthy adults. In the present study high BMI was identified as a major contributor to elevated blood pressure, particularly SBP. Probably, DBP which is a function of total peripheral resistance is not influenced to such a great extent at an early stage of life.
In our study, frequency of males with prehypertension was significantly higher compared to females. Eran Israeli et al., have found that mean SBP and DBP is significantly higher in male subjects [19]. P Das et al., have also reported higher BP in the male gender [20]. Rima Abdul Razzak et al., have found significant difference particularly in SBP between the two genders [21]. Our study finding along with the other study findings suggest that males are at greater risk of hypertension.
In the present study BMI and waist circumference of prehypertensive group was significantly higher compared to normotensive group. The BMI is widely used as a surrogate measure of overall adiposity because of its simplicity and high correlation with percent body fat [22]. Adult obesity-measured by relative weight or body mass index is a strong risk predictor of CVD-diabetes mellitus and mortality from all causes [23]. These observations suggest that physical activities aiming at weight control should be implemented in medical training curriculum too.
Researchers investigating on causes of hypertension have observed that sleep deprivation [24,25], diet pattern [26], and stress [7] as some of the risk factors of hypertension. However, in our study we did not find any supportive evidence. On the other hand sleep quality assessed by PSQI score was higher in subjects whose diastolic blood pressure was within normal range. Most of these previous studies have investigated association between these risk factors and hypertension in subjects aged 40 years and above unlike subjects aged between 18-23 years in this study. Prolonged sleep loss and alterations of sleep quality have been identified as physiological stressor that impairs brain function and causes over activation of stress system, thereby elevating BP [27]. However, repeated blood pressure elevations and surge of catecholamines during stress, over the years, may cause sustained high blood pressure [7]. Thus, we speculate that poor sleep quality and perceived stress of much longer duration may cause quantifiable elevation in blood pressure. In young adults probably counter regulatory mechanisms in combating rise in blood pressure may be more active compared to older subjects.
This was a pilot study undertaken to find the association between known risk factors of cardiovascular disease and prehyperstensive state in apparently young healthy adults. To the best of our knowledge, currently there is no scoring system as such to assess collective effect of several cardiovascular risk factors in apparently healthy subjects. Thus the scoring system followed in this study needs to be explored further in different sets of population.
This cross-sectional study mainly looked at the influence of cardiovascular risk factors contributing to prehypertensive state. Thus follow-up studies of longer period are required to assess the implication of high systolic blood pressure observed in our young adults. The systolic blood pressure is a function of the cardiac output, that is, it represents the extent of work done by the heart [28]. Therefore it could be speculated that systolic prehypertensive heart works more than normal heart and if neglected may eventually lead to heart failure.
Conclusion
Male gender and family history are inherited and cannot be changed, thus used as non-modifiable risk factors in this study. Whereas other risk factors such as higher body weight, sleep quality, diet pattern, sedentary life can be altered and are the modifiable risk factors. In the present study, incidence of prehypertension was significantly higher in males compared to female subjects. In both males and female prehypertensives, BMI (a modifiable risk factor) was higher compared to normotensives. In addition in prehypertensive females, waist circumference was higher compared to female normotensives. Thus it could be concluded that in apparently healthy young adults, male gender and obesity are the major risk factors of elevated blood pressure.