Bilateral Vocal Cord Palsy with Arnold Chiari Malformation: A Rare Case Series
Nikhil Arora1, Ruchika Juneja2, Ravi Meher3, Eishaan K. Bhargava4
1 Senior Resident, Department of Ear, Nose and Throat, Maulana Azad Medical College and Associated Lok Nayak Hospital, New Delhi, India.
2 Junior Resident, Department of Ear, Nose and Throat, Maulana Azad Medical College and Associated Lok Nayak Hospital, New Delhi, India.
3 Professor, Department of Ear, Nose and Throat, Maulana Azad Medical College and Associated Lok Nayak Hospital, New Delhi, India.
4 Senior Resident, Department of Ear, Nose and Throat, Maulana Azad Medical College And Associated Lok Nayak Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ruchika Juneja, Junior Resident, Department of ENT and Head and Neck Surgery, B L Taneja Block, 3rd Floor, Lok Nayak Hospital, Bahadur Shah Zafar Marg, New Delhi -110002, India.
E-mail: junejaruchika1@gamil.com
Stridor in paediatric age group is not an uncommon presentation to the ENT emergency. The range of differential diagnosis is vast. The presentation may vary from noisy breathing to severe respiratory distress and apnea. Early and meticulous diagnosis is crucial for the management as the condition may be life threatening. We report a rare case series of 3 infants with Arnold Chiari Malformation who presented to the hospital with stridor and were diagnosed with bilateral vocal cord palsy. These 3 infants had similar underlying neurological condition with hydrocephalus and raised intracranial pressure. Chiari malformation is the one of the most common congenital central nervous system anomaly associated with bilateral vocal cord paralysis. However, the presentation is rare. This article, thus, emphasizes the significance of early diagnosis and immediate management of this condition.
Hydrocephalus, Myelodysplasia, Stridor
Case Series
Case 1
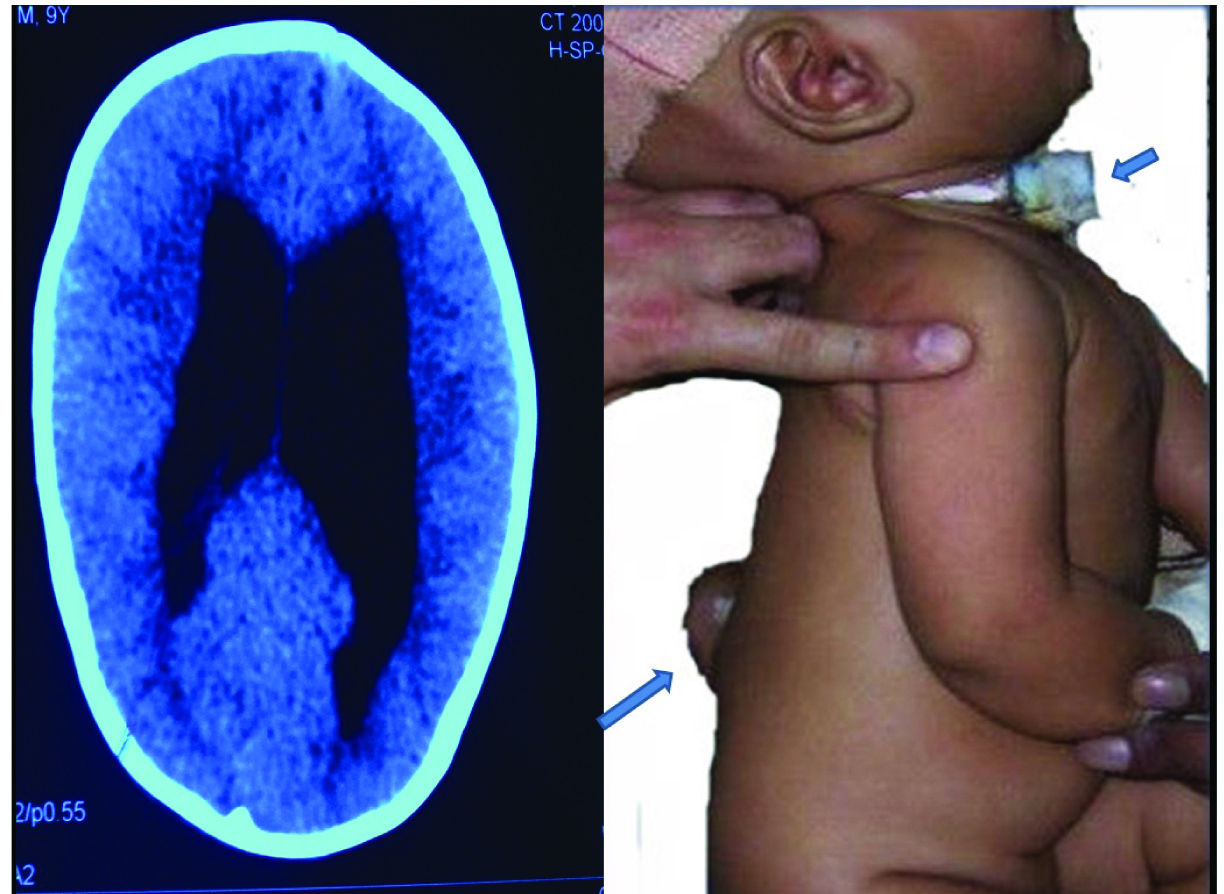
A four-month-old infant presented to the ENT emergency with an acute episode of difficulty in breathing for last 5 days. According to the parents, the child was previously taken to a local practitioner who misdiagnosed the respiratory distress as pneumonitis. The child was managed conservatively and failed to show any signs of improvement. On examination, he had inspiratory stridor, but there was no history of fever, trauma or upper respiratory tract infection. Examination revealed a lumbar meningomyelocele without any apparent neurological deficit. CT scan of head demonstrated severe hydrocephalus and tonsillar herniation due to Arnold Chiari malformation type II. Direct laryngoscopy revealed bilateral vocal cord palsy and the child was intubated with 3.5mm uncuffed endotracheal tube for an emergency ventriculo-peritoneal shunt procedure which was done to relieve the increased intracranial tension. After extubation, the stridor was persistent, due to which the child required reintubation, although he was breathing spontaneously without assisted mechanical ventilation. After observing for an hour, the patient was shifted to ICU and second trial of extubation was planned. After 48 hours, second trial of extubation also failed. Flexible laryngoscopy was carried out to confirm bilateral cord palsy and then the child was tracheostomized [Table/Fig-1]. The child was relieved of stridor and respiratory distress. Repeat direct laryngoscopy after 15 days showed improvement with return of right vocal cord movement and bilateral mobility of vocal cords were demonstrable after another week. Later, the child was taken up for repair of the lumbar meningomyelocele. The tracheostomy tube was removed after endoscopic laser fulguration of the suprastomal granulations.
Showing the hydrocephalus as in NCCT head of the child and clinical picture with tracheostomy tube in situ and the lumbar meningomyelocele.
Case 2
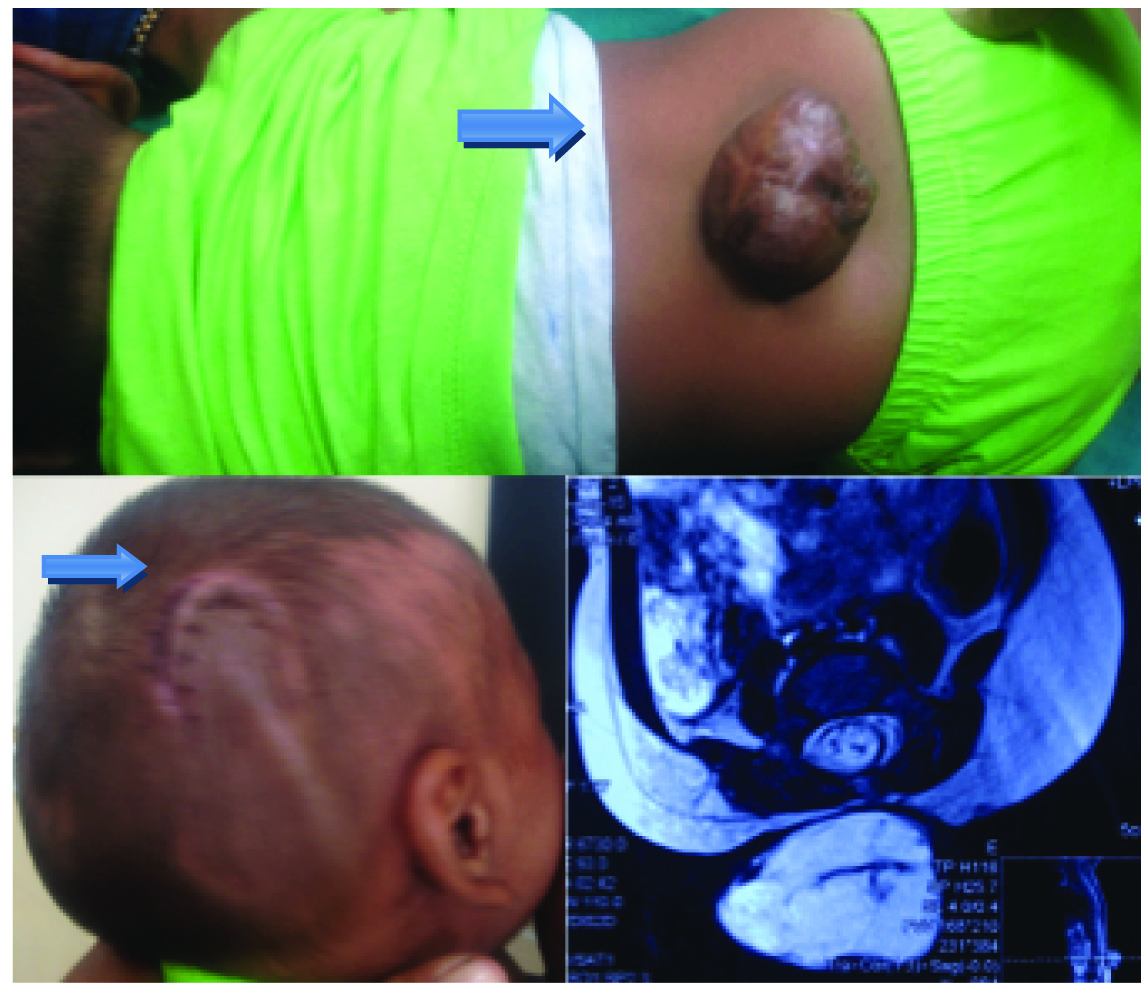
A nine-month-old child [Table/Fig-2] was brought to the ENT OPD with complaints of noisy breathing since last 2-3 weeks without any respiratory distress, no previous history of upper respiratory tract infection, fever and trauma. Patient had a lumbar meningomyelocele without any neurological deficit. MRI revealed type II Arnold Chiari malformation with lumbar meningomyelocele with syringohydromyelia with tonsillar herniation and hydrocephalus. On fibre optic laryngoscopic examination, vocal cords were found lying in paramedian position with no lateral movement. Child was taken up for emergency ventriculo-peritoneal shunt to relieve the raised intracranial tension, after which the stridor was relieved within 15 days. Repeat laryngoscopy showed improvement in vocal cord mobility. The child was taken up for repair of meningomyelocele in the second stage under general anaesthesia.
Showing clinical and radiological picture of the second patient with lumbar meningomyelocele with theventriculo-peritoneal shunt scar.
Case 3
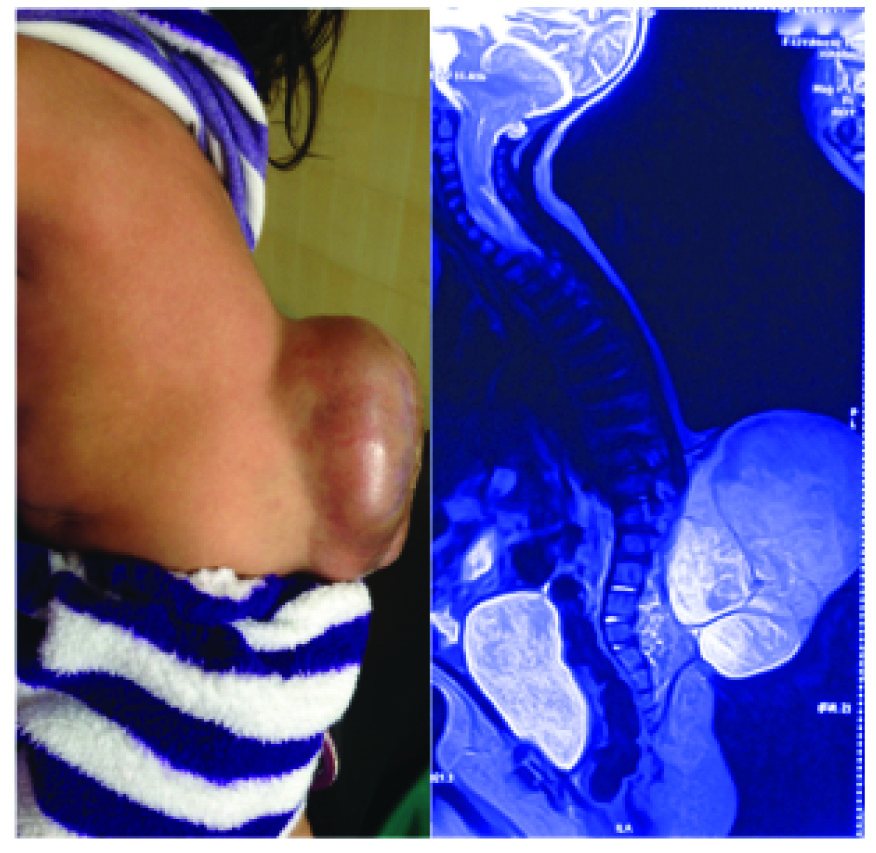
Another nine-month-old child was brought to the ENT OPD with complaints of noisy breathing since 4-5 days with a previous history of upper respiratory tract infection. However, the child did not have any respiratory distress and maintained normal oxygen saturation on room air. On examination, the child had a large lumbosacral meningomyelocele with inspiratory stridor [Table/Fig-3], without any signs of neurological deficit. Right sided pre-auricular tags were also observed. MR brain and spine revealed type II Arnold Chiari malformation, with moderately dilated lateral and third ventricles with tonsillar herniation and compression of the spinal cord. On fibre optic bronchoscopic examination, patient was found to have bilateral abductor cord palsy. Before the child could be taken up for surgery, the meningomyelocele sac burst and there was cerebrospinal fluid leak, relieving the raised intracranial tension. Stridor resolved spontaneously after a week. Laryngoscopy was repeated and the vocal cord mobility was found to have improved. Later, the meningomyelocele was repaired.
Showing the clinical photograph of the patient along with the MRI film suggestive of a large lumbar meningomyelocele.
Discussion
Bilateral vocal cord palsy is the second most common cause of stridor, after laryngomalacia, accounting for 10-15% of cases [1]. Bilateral vocal cord palsy is often idiopathic; however it may be associated with neurological anomalies like Arnold Chiari malformation, intraventricular haemorrhage, meningoencephalocele and hydrocephalus. It may also follow a traumatic forceps delivery, mediastinal surgery, or ligation of Patent ductus arteriosus [1]. Chiari first described different variations of hindbrain herniation through the foramen magnum in 1891 [2]. Type I Arnold Chiari malformations typically involve downward displacement of the cerebellum and cerebellar tonsils that produces a small posterior fossa. This malformation is often an isolated finding. Arnold Chiari II malformation involves downward displacement of the cerebellar vermis, medulla and fourth ventricle. This is strongly associated with hydrocephalus and myelodysplasia. These patients often have intrinsic brainstem histopathological changes that can produce symptoms of bulbar dysfunction (hindbrain dysfunction). Both types of Chiari malformation scan be easily identified on radiological imaging (computed tomography or magnetic resonance imaging) of the craniovertebral junction. Type III Chiari malformation is an encephalocervical-meningocele and type IV refers to cerebellar hypoplasia [3].
The Chiari II malformation is the leading cause of death in children with treated myelodysplasia during first 2 years of life [4]. They usually present with cranial nerve and brain stem dysfunction with dysphagia (92%), stridor or bilateral vocal cord paralysis (69%) or apnoea (54%) [5]. Charney and co-workers classified patients on the basis of their initial brain stem dysfunction and found that the patients with stridor alone, who were classified as Grade I, had minimum mortality. Grade II patients exhibiting stridor and apnoea possessed a 50% chance of recovery. Grade III patients who exhibited stridor, apnoea, cyanotic spells and dysphagia had minimal chances of recovery and a 40% chance of survival. Grade II, III are caused by more extensive brainstem damage due to haemorrhage, infarction and necrosis [6]. Holinger et al., have described a series of 21 children who had stridor associated with meningomyelocele, Arnold chiari malformation and hydrocephalus. Thirteen of these patients also presented with episodes of apnoea. Temporal association of vocal cord paralysis with raised intracranial pressure was noticed during the study [7].
Vocal cord paralysis with inspiratory stridor during infancy is a complication of the Chiari II malformation associated with meningomyelocele, though rarely found with type I Chiari malformation [8]. This develops with acute downward or upward displacement of the malformed brainstem secondary to increased or decreased intracranial pressure. The treatment of these symptoms requires a decompression of the raised intracranial pressure, which reduces the pressure difference between the intracranial and the intraspinal compartments. Yamada et al., have reported the importance of immediate ventriculo-peritoneal shunting in 12 patients of Arnold Chiari malformation with stridor. This procedure provided symptomatic relief to the patients [9]. Solan and Glaisyer had described a case of a neonate who was born with meningomyelocele and had stridor. The cause of stridor was ascertained to be due to evolving hydrocephalus. Symptoms were relieved immediately after direct tapping of the cerebrospinal fluid from the right coronal horn via the coronal suture [10].
The diagnosis of bilateral vocal cord palsyis established by direct laryngoscopy performed without general anaesthesia. Chaten et al., have documented 9 patients who developed unilateral or bilateral vocal cord paralysis in a PICU setting. It was either due to iatrogenic trauma during thoracic surgery or underlying neurological condition with documented or suspected intracranial hypertension. They also discussed the significance of early visualisation of larynx in cases of children who became stridulous post extubation and had underlying neurological disorders associated with raised intracranial tension. Four patients out of seven with neurological disorder regained cord mobility in 4 months [11].
It is to be emphasized that in case of an emergency, endotracheal intubation or tracheotomy should be considered to establish an airway with immediate ventricular puncture. Ventricular shunting procedures to reduce intracranial pressures should ideally be performed within the first 48 hours after the onset of features of hindbrain dysfunction [5]. Delayed procedure reduces the likelihood of recovery of vocal cord paralysis. The degeneration of nucleus ambiguous leads to irreversible paralysis of vocal cords [6,12]. The bilateral vocal cord paralysis may be totally reversed if the intracranial pressure is decreased on time [5]. Glossopharyngeal, vagus and accessory nerves may be involved due to hindbrain dysfunction.
Conclusion
A possibility of bilateral vocal cord palsy should be speculated if stridor is observed in an infant with meningomyelocele. Laryngoscopic examination is imperative for diagnosis in children with stridor. Early decompression of the raised intracranial tension can reverse the palsy, alleviating the stridor and thus, the need for a tracheostomy. Hence, early recognition, diagnosis and management of these abnormalities may be lifesaving.
[1]. Kaushal M, Upadhyay A, Aggarwal R, Deorari AK, Congenital stridor due to bilateral vocal cord palsyIndian J Paediatr 2005 72:444 [Google Scholar]
[2]. Koehler PJ, Chiari’s description of cerebellar ectopy (1891). With a summary of Cleland’s and Arnold’s contributions and some early observations on neural-tube defectsJournal of Neurosurgery 1991 75(5):823-36. [Google Scholar]
[3]. Gupta N, Elizabeth Ross M, Disorders of Neural Tube DevelopmentIn: Swaiman’s Paediatric Neurology: Principles and Practice. Kenneth F. Swaiman, Stephen Ashwal, Donna M. Ferriero, Nina F. Schor 2012 EdinburghElsevier Saunders:125-144. [Google Scholar]
[4]. McLone DG, Results of treatment of children born with a myelomeningocoelClin Neurosurg 1983 30:407-12. [Google Scholar]
[5]. Pollack I, Kinnunen D, Albright A, The effect of early craniocervial decompression on functional outcome in neonates and young infants with myelodysplasia and symptomatic Chiari II malformations: Results from a prospective seriesNeurosurgery 1996 38:703-10. [Google Scholar]
[6]. Charney EB, Rorke LB, Sutton LN, Schut L, Management of Chiari II complications in infants with myelomeningoceleJ Paediatr 1987 111:364-71. [Google Scholar]
[7]. Holinger PC, Holinger LD, Reichert TJ, Holinger PH, Respiratory obstruction and apnea in infants with bilateral abductor vocal cord paralysis, meningomyelocele, hydrocephalus, and Arnold-Chiari malformationJ Paediatr 1978 92(3):368-73. [Google Scholar]
[8]. Allsopp GM, Karkanevatos A, Bickerton RC, Abductor vocal fold palsy as a manifestation of type one Arnold Chiari malformationJ Laryngol Otol 2000 114:221-23. [Google Scholar]
[9]. Yamada H, Tanaka Y, Nakamura S, Laryngeal stridor associated with the Chiari II malformationChild Nerv Syst 1985 1(6):312-18. [Google Scholar]
[10]. Solan K, Glaiyser H, Raised intracranial pressure in a neonate presenting as stridorPaediatr Anaesth 2006 16(8):877-79. [Google Scholar]
[11]. Chaten FC, Lucking SE, Young ES, Mickell JJ, Stridor: intracranial; pathology causing postextubation vocal cord paralysisPaediatrics 1991 87(1):39-43. [Google Scholar]
[12]. Bell WO, Charney EB, Bruce DA, Sutton LN, Schut L, Symptomatic Arnold-Chiari malformation: review of experience with 22 casesJ Neurosurg 1987 66:812-16. [Google Scholar]