Biodentine-A New Novel Bio-Inductive Material For Treatment of Traumatically Injured Tooth (Single Visit Apexification)
Babita Niranjan1, Nandihalli Devendrappa Shashikiran2, Aashutosh Dubey3, Shilpy Singla4, Neha Gupta5
1 Senior Lecturer, Department of Pedodontics and Preventive Dentistry, Rishiraj College of Dental Sciences, Bhopal, Madhya Pradesh, India.
2 Dean, Professor and Head, Department of Pedodontics and Preventive Dentistry, College of Dental Science, Karad, Maharasthra, India.
3 Senior Lecturer, Department of Periodontology & Oral Implantology, People’s Dental Academy, Bhopal, Madhya Pradesh, India.
4 Associate Professor, Department of Pedodontics and Preventive Dentistry, People’s College of Dental Sciences and Research, Bhopal, Madhya Pradesh, India.
5 Senior Lecturer, Department of Oral Medicine & Radiology, People’s College of Dental Sciences and Research, Bhopal, Madhya Pradesh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Babita Niranjan, Senior Lecturer, Department of Pedodontics and Preventive Dentistry, Rishiraj College of Dental Sciences, Bhopal, Madhya Pradesh, India.
E-mail: dr.babitaniranjan@gmail.com
Immature teeth, Open apex, Apical barrier induction
An eight-year-old female patient reported to Department of Pedodontics, People’s Dental College, Bhopal with dental trauma, resulting in coronal fracture of upper central incisors (11 and 21). Clinical examination revealed Elli’s fracture class IV with no associated symptoms [Table/Fig-1]. Electrical and heat pulp testing showed a negative result, as at time of injury sensibility tests frequently give no response, due to transient lack of pulpal response. So a 2-3 weeks interval radiographic assessment showed an arrested apical root development with respect to 11 and 21 [Table/Fig-2]. Therefore, a treatment plan included was apexification procedure.
Preoperative view showing Elli’s Class IV fracture (Traumatized tooth that has become non-vital with or without loss of tooth structure) wrt 11 & 21.

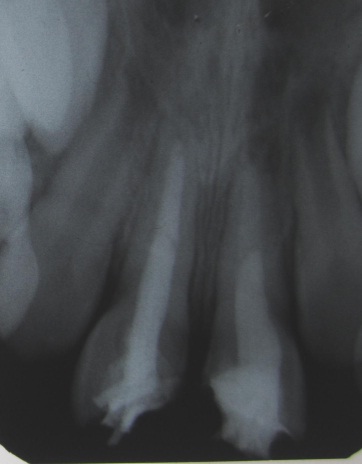
Preoperative radiograph showing oblique fracture line involving pulp and arrested apical root development wrt 11 & 21.

After the administration of local anaesthesia, affected teeth were isolated under rubber dam. Access cavities were prepared followed by preparation of canal very lightly owing to thin dentinal walls, with copious irrigation using 0.5% sodium hypochlorite (NaOCl). A lower strength was used due to an increased risk of extruding NaOCl through open apex [1]. ProRoot white MTA (Dentsply/Tulsa Dental, USA) was placed wrt 21 [Table/Fig-3]. MTA was mixed as per manufacturer’s instructions to obtain putty like consistency [2]. This mix was then placed in desired location and condensed lightly by using an endodontic plugger of ISO size 100 to form an apical plug of 4–5 mm.
Apical plug induction with biodentine wrt 11 & mineral trioxide aggregate wrt 21.

Biodentine (Sepotodont) was placed with respect to tooth number 11 [Table/Fig-3]. Biodentine was mixed as per manufacturer’s instructions to obtain a creamy consistency. This mix was then pushed with a root-canal plugger of ISO size 100 and condensed to form an apical plug of 4-5 mm. The thickness of apical barrier and adaptation of material to dentinal walls was established using radiograph [Table/Fig-3]. Obturation of canal was done with gutta-percha [Table/Fig-4], followed by post preparation by removing 4-5 mm of gutta percha, glass-fibre reinforced post placement, and cementation by bonded resin luting cement. A bonded core was used to permanently seal canal system and composite resin restoration was done with respect to 11 and 21 [Table/Fig-5].
Intraoral periapical view showing obturation of the canal with gutta-percha.
Postoperative view showing esthetics restoration with composite resin restoration wrt 11 & 21.

The patient was recalled at 6 and 12 month interval [Table/Fig-6]. History and clinical examination revealed satisfactory healing and intraoral periapical radiograph showed adequate periapical response as well.
Intraoral periapical radiograph at 12 month time interval wrt 11 & 21, which showed better root growth & dentin thickness in biodentine than mineral trioxide aggregate.

Discussion
For a successful endodontic treatment, proper clinical and radiographic assessment is mandatory particularly in young permanent teeth following trauma [2]. In such teeth ideal choice of treatment is apexification procedure. Traditionally, apexification was introduced by filling canal with calcium hydroxide and iodoform mixture for a period of 3 to 6 months [3]. The main disadvantage being is dressing needs to be change frequently to induce apical healing and time required is long [2]. Newer bioactive materials like MTA and Biodentine are introduced to induce artificial apical barrier in a single visit.
In present case apexification procedure was done by using MTA and Biodentine with respect to 21 and 11 respectively. Main disadvantages of MTA are longer setting time (24-72 hours), higher cost and difficult to handle [3]. Biodentine is Ca3SiO5 based material introduced by septodont’s research group, to improve physical properties like short setting time, high mechanical strength, ease of handling, making it more compatible clinical cases of dentin replacement [4]. Increasing setting time is achieved by a combination of two factors. First reduction in particle size as it greatly influences setting time and second decrease of liquid content which decrease its setting time within 9 to 12 minutes [4]. Biodentine set through a hydration reaction that involves dissolution of calcium silicate granules to produce calcium hydroxide and calcium silicate hydrates. The C-S-H gel formation is due to permanent hydration of tricalcium silicate, which gradually fills in the spaces between tricalcium silicate grains and improves sealing [4].
Better sealing ability between dentin and biodentine could be attributed to surface crystal growth within dentinal tubules, leading to possible ion exchanges between cement and dentin bio-structure. At the material-dentin interface, biodentine results in formation of tag-like structures alongside an interfacial layer called “mineral infiltration zone” [5]. Ca and Si rich interfacial layer can be observed under magnification, which may result in higher acid resistance as well as physical strength.
At 6 and 12 month follow-up period, Biodentine showed better root growth as well as dentin thickness than MTA. Biodentine represents a great improvement than MTA, as mechanical properties like compressive strength; elasticity modulus and microhardness are similar to those of natural dentin, making it an ideal material for single visit apexification.
Conclusion
Post-endodontic restorations are of great significance as immature anterior teeth have a higher tendency for cervical root fracture. From present case report we can conclude that new calcium-based biodentine can be an efficient alternative to conventional apexification materials. Biodentine is new biologically active cement represents a promising evolution of MTA technology.
[1]. Muhammad AH, Ayah J, Mai A, Azzalden A, Management of permanent teeth with calcium hydroxide pasteIntern J Dent Health Sci 2016 3(1):1305-131. [Google Scholar]
[2]. Bajwa NK, Jingarwar MM, Anuradha Pathak A, Single visit apexification procedure of a traumatically injured tooth with a novel bioinductive material (Biodentine)Int J Clin Pedia Dent 2015 8(1):58-61. [Google Scholar]
[3]. Rafter M, Apexification: a reviewDent Traumatol 2005 21(1):1-8. [Google Scholar]
[4]. Camilleri J, Investigation of Biodentine as dentine replacement materialJ Dent 2013 41(7):600-10. [Google Scholar]
[5]. Koubi G, Colon P, Franquin JC, Hartmann A, Richard G, Faure MO, Clinical evaluation of the performance and safety of a new dentin substitute, Biodentine, in the restoration of posterior teeth — a prospective studyClin Oral Investig 2013 17(1):243-49. [Google Scholar]