Dynamic Hip Screw with Trochanteric Stablization Plate Fixation of Unstable Inter-Trochanteric Fractures: A Prospective Study of Functional and Radiological Outcomes
Ashwin Shetty1, Arjun Ballal2, Anand Kumar Sadasivan3, Anoop Hegde4
1 Associate Professor, Department of Orthopaedic Surgery, K.S. Hegde Medical Academy, Mangalore, Karnataka, India.
2 Registrar, Department of Orthopaedic Surgery, ARS Hospital, Tirupur, Tamil Nadu, India.
3 Senior Consultant and Surgeon, Department of Orthopaedic Surgery, ARS Hospital, Tirupur, Tamil Nadu, India.
4 Registrar, Department of Orthopaedic Surgery, ARS Hospital, Tirupur, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Arjun Ballal, Registrar, Department of Orthopaedic Surgery, ARS Hospital, 6/53, 6th Street, Thennampalyam Extension, Palladam Road, Tirupur, Tamil Nadu, India.
E-mail: 5arjunballal@gmail.com
Introduction
Management of unstable intertrochanteric fractures have posed a unique challenge to orthopaedicians over years. Several surgical techniques and implants have been developed for the same. Fractures of the lateral wall have been considered as the major cause of femoral medialization after fixation by Dynamic Hip Screw (DHS). Studies have shown that supplementation of trochanteric stabilization plate reduces the incidence of femoral medialization.
Aim
To assess the radiological union and hip function after fixation of unstable intertrochanteric fractures with DHS and Trochanteric Stabilization Plate (TSP).
Materials and Methods
A prospective study was conducted with a total of 32 patients between age groups of 30-70 years with Evan Jensen unstable and very unstable type of intertrochanteric fractures, between August 2013 to March 2015 in the Department of Orthopaedics ARS Hospital, Tirupur, Tamil Nadu, India. They underwent open reduction and DHS and TSP fixation. They were started on full weight bearing mobilization on post op day three. They were reviewed at post-op weeks 3,6,12 and 24. Hip mobilization and rehabilitation exercises were instituted during course of reviews. Radiographs were taken to assess fracture union and hip function was evaluated during follow-ups. At the end of 24 weeks, degree of radiographic union was scored as per Radiological Union Score for Hip (RUSH). Hip function was scored with Harris hip score. Analyses were done using frequency and proportions. Chi-square tests were used to assess the test of association.
Results
Fifteen patients had RUSH scores between 10-20 and 17 patients had scores between 20-30 points. RUSH score had mean of 21.03+/- 2.132 points. 9 of 32 patients had excellent results as per Harris hip score, 10 had good, nine had fair and four had poor. On comparison of Harris hip score with RUSH score: Interval between 10-20 points, of 15 patients; two had excellent results, five had good, five had fair and three had poor. Of 17 patients between 20-30 points, seven had excellent, five had good, four had fair and one had poor results.
Conclusion
DHS and TSP fixation of unstable intertrochanteric fractures is an effective technique with good radiological and functional outcome.
Evan Jensen classification, Full weight bearing mobilization, Harris hip score, Intra-medullary devices, Radiological Union Score for Hip
Introduction
Fractures of the hip can be considered a major contributor of disability primarily in the elderly in the world [1]. Inter-trochanteric fractures form nearly the one-half of all the hip fractures in the world, they have a negative impact on the quality of life [2,3]. There have been many advancements and research for the ideal implant for management of these injuries. Achieving a stable fixation in these fractures is the prime motive of managing these injuries. Several factors contribute to the stability of fixation: fracture geometry and stability, bone quality, comminution, choice of implant and surgical technique are some of them [4].
The unstable intertrochanteric fractures with loss of postero-medial contact or lateral wall contact or both are a major cause of telescoping and medialization with a biomechanically unstable head-neck fragment [5]. This results in significant limb shortening, fracture collapse and implant failure which increase the rates of re-operation [5]. Parker and colleagues first noted the importance of integrity of the lateral wall after fixation of these injuries [6].
Trochanter Stabilizing Plate (TSP) is used to stabilize the greater trochanter and the lateral wall and it is used as a modular extension of the Dynamic Hip Screw (DHS) [7]. Fixation of unstable intertrochanteric fractures with a TSP have noted to have lesser incidence of femoral medialization and improvement is noted in the functional outcome [5,8–10].
Aim
To assess the radiological and functional outcome of hip after fixation of unstable intertrochanteric fractures with DHS and TSP.
Materials and Methods
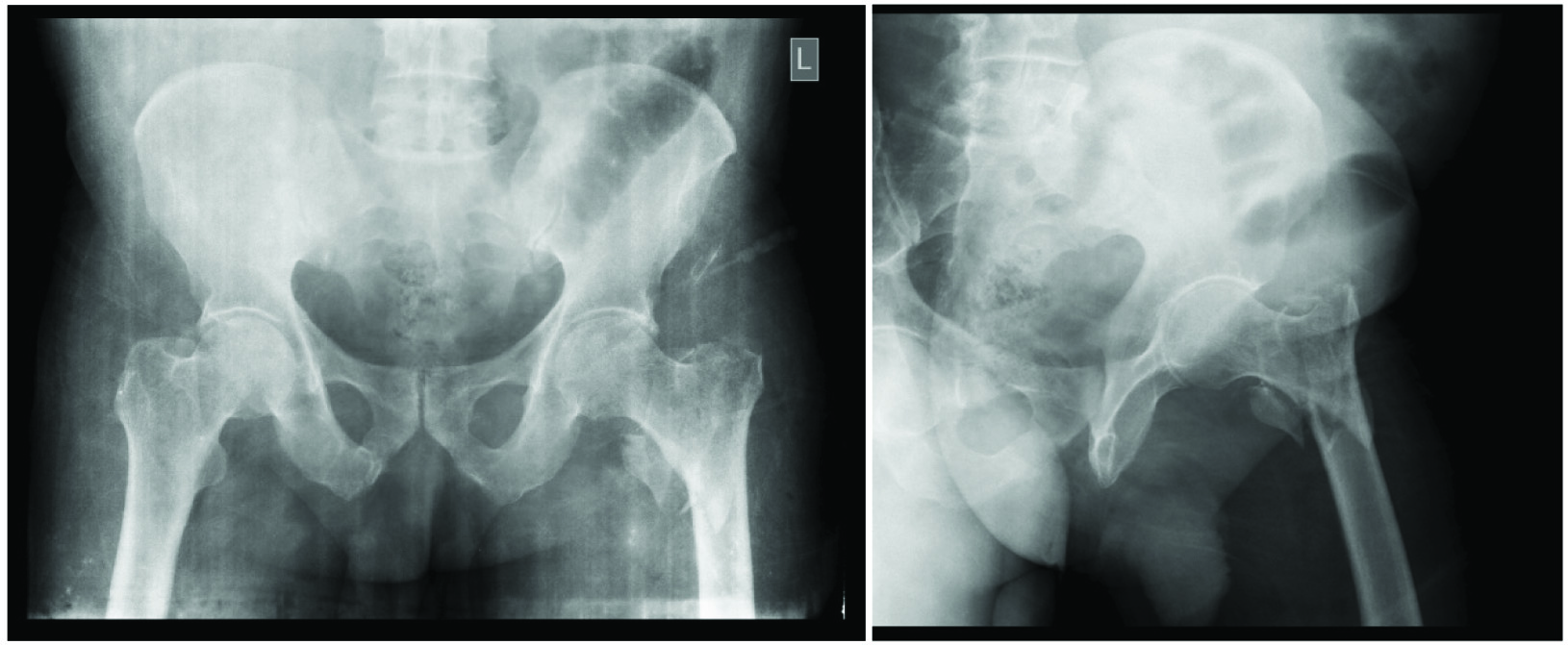
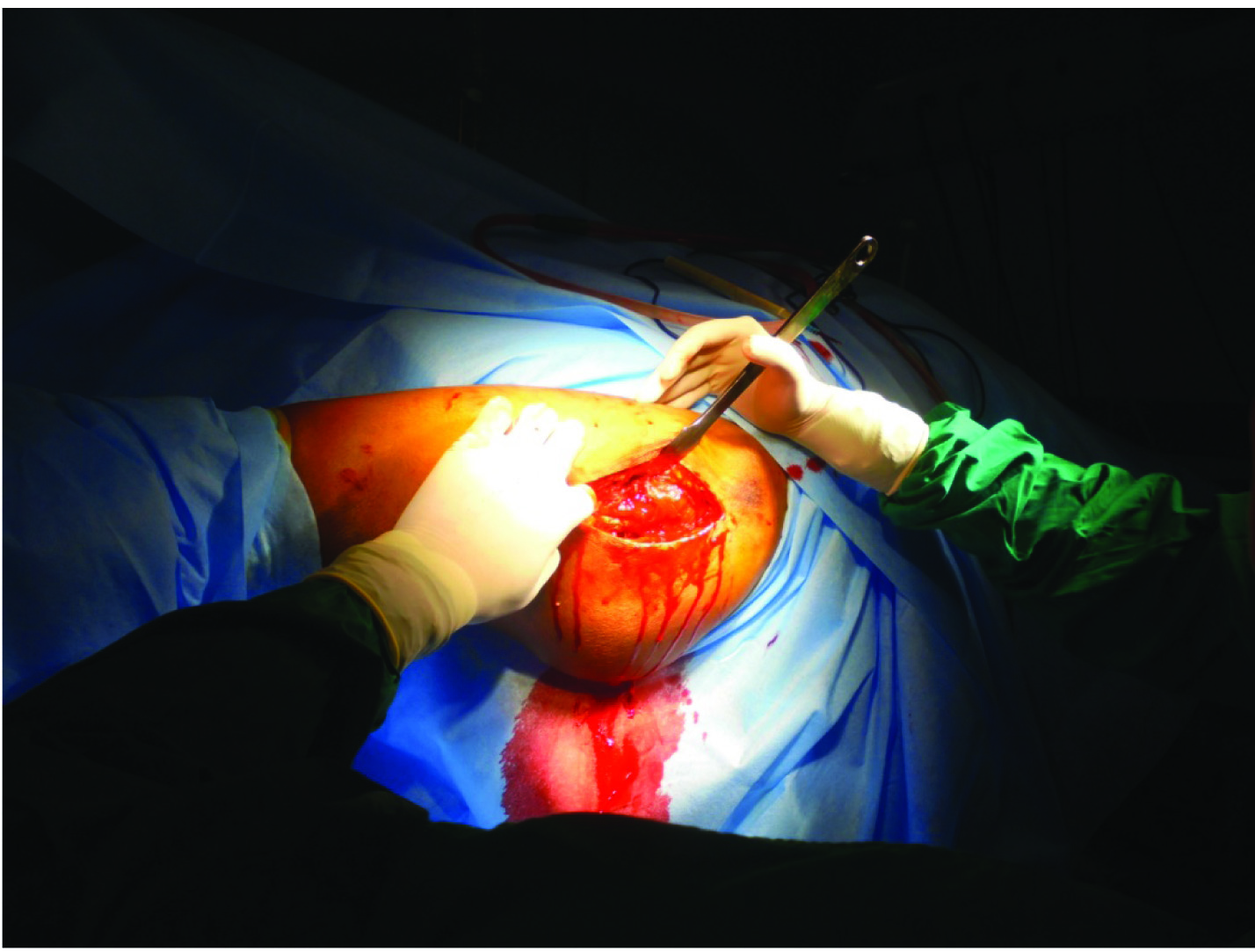
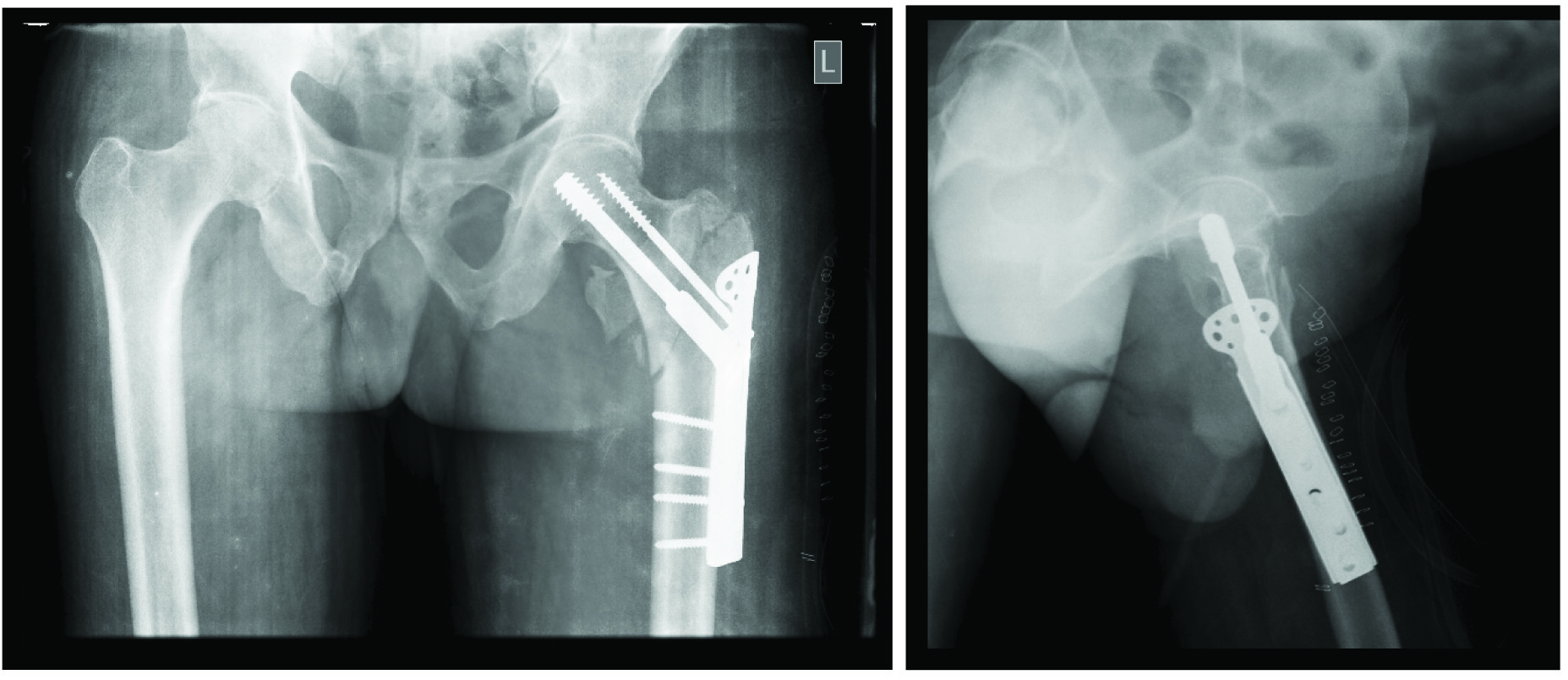
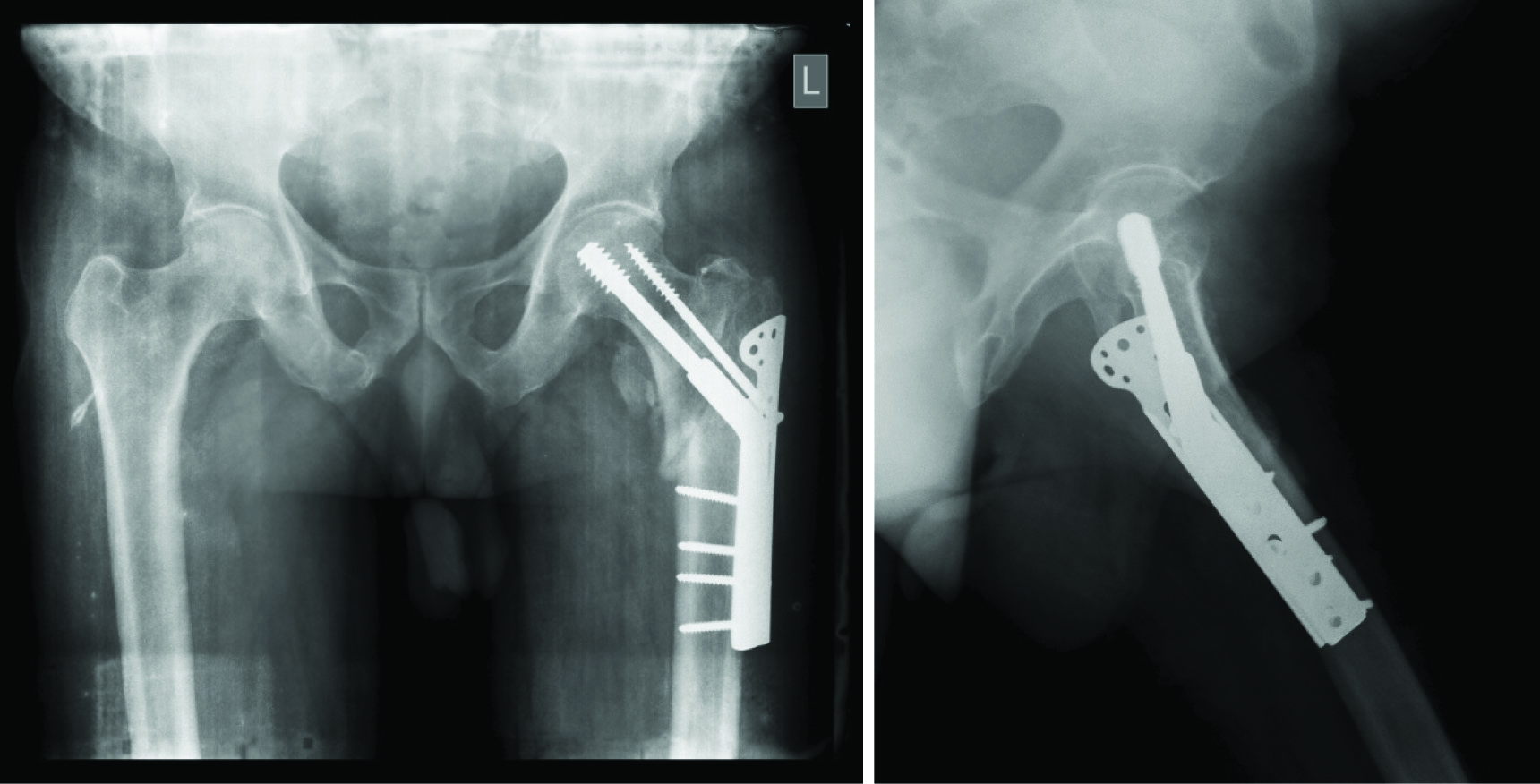
A prospective study was conducted in the Department of Orthopaedics, ARS hospital, Tirupur, Tamil Nadu, India from August 2013 to March 2015. A total of 32 patients with fresh closed Evan-Jensen unstable and very unstable type of intertrochanteric fractures [Table/Fig-1a&b] [4] were enrolled into the study. The age group under the inclusion criteria was 30-70years. Pathological fractures, bones with Singh’s index [11] below IV, patients with associated pathologies hip and knee, patients with other associated fractures of ipsilateral and contralateral femur (shaft or neck fractures) or other ipsilateral and contralateral lower limb injuries and associated spine injuries were excluded from the study. The surgical technique [7] employed a lateral approach to the hip [Table/Fig-2]. Guide wire insertion was done below the centre in the anteroposterior fluoroscopic image and central in the lateral fluoroscopic image. Triple reaming was done and appropriate size lag screw was inserted, side plate was fixed with insertion of only the second screw. Usually a four-hole side plate was used in almost all our cases. Appropriate size TSP was selected after assessing its placement under fluoroscopic guidance and then was placed and fixed with insertion of the remaining screws. Skin closure was done in layers. Postoperative radiographs were taken the same evening in anteroposterior and lateral views [Table/Fig-3a&b]. On postoperative day three full weight bearing mobilization of all cases was begun. The patient was discharged at postoperative day 10 after suture removal and mobilization exercises for the hip were started and hip function was assessed during all the reviews. The patient was reviewed at week 3,6,12,24 weeks. Serial radiographs were taken, active and passive hip mobilization and rehabilitation was continued. The final follow-up was at 24 weeks and radiographs were taken [Table/Fig-4a&b] and the radiographic union of the fracture in this review was scored as per the Radiographic Union Score of the HIP (RUSH score) [12]. Hip function at 24 weeks was assessed and scored as per the Harris hip score [13,14]. The results were tabulated. Analyses were done using frequency and proportions. Chi-square tests were used to assess the test of association.
Anteroposterior and lateral images of the pelvis with both hips showing Evan Jansen very unstable type intertrochanteric fracture of left femur.
Intraoperative image showing lateral exposure to the fracture after positioning of patient on fracture table.
Postoperative anteroposterior and lateral radiographs after fixation of the fracture with DHS and TSP.
Anteroposterior and lateral radiographs of taken at six months post-op showing good callus formation and a uniting left intertrochanteric fracture.
Results
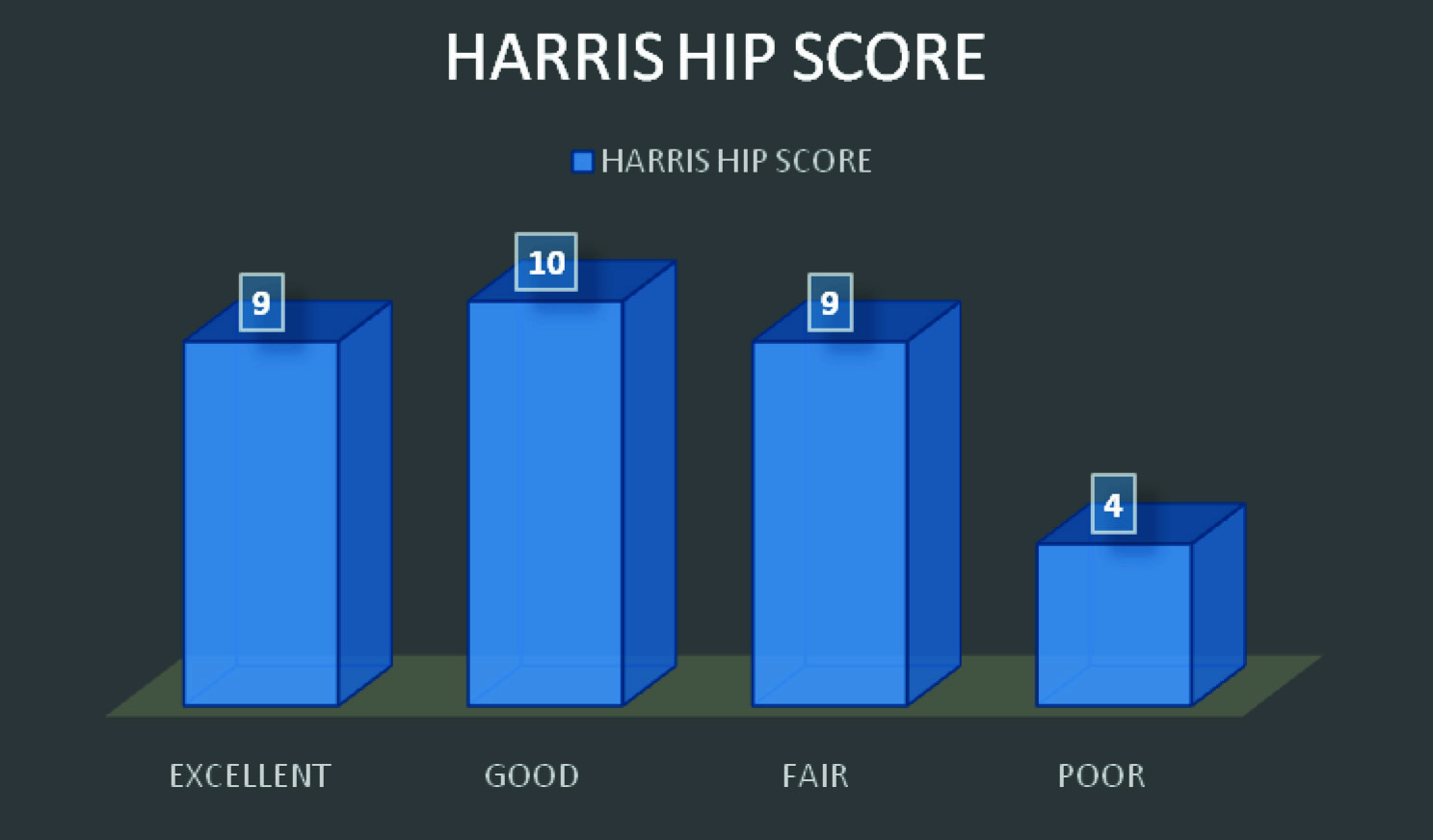
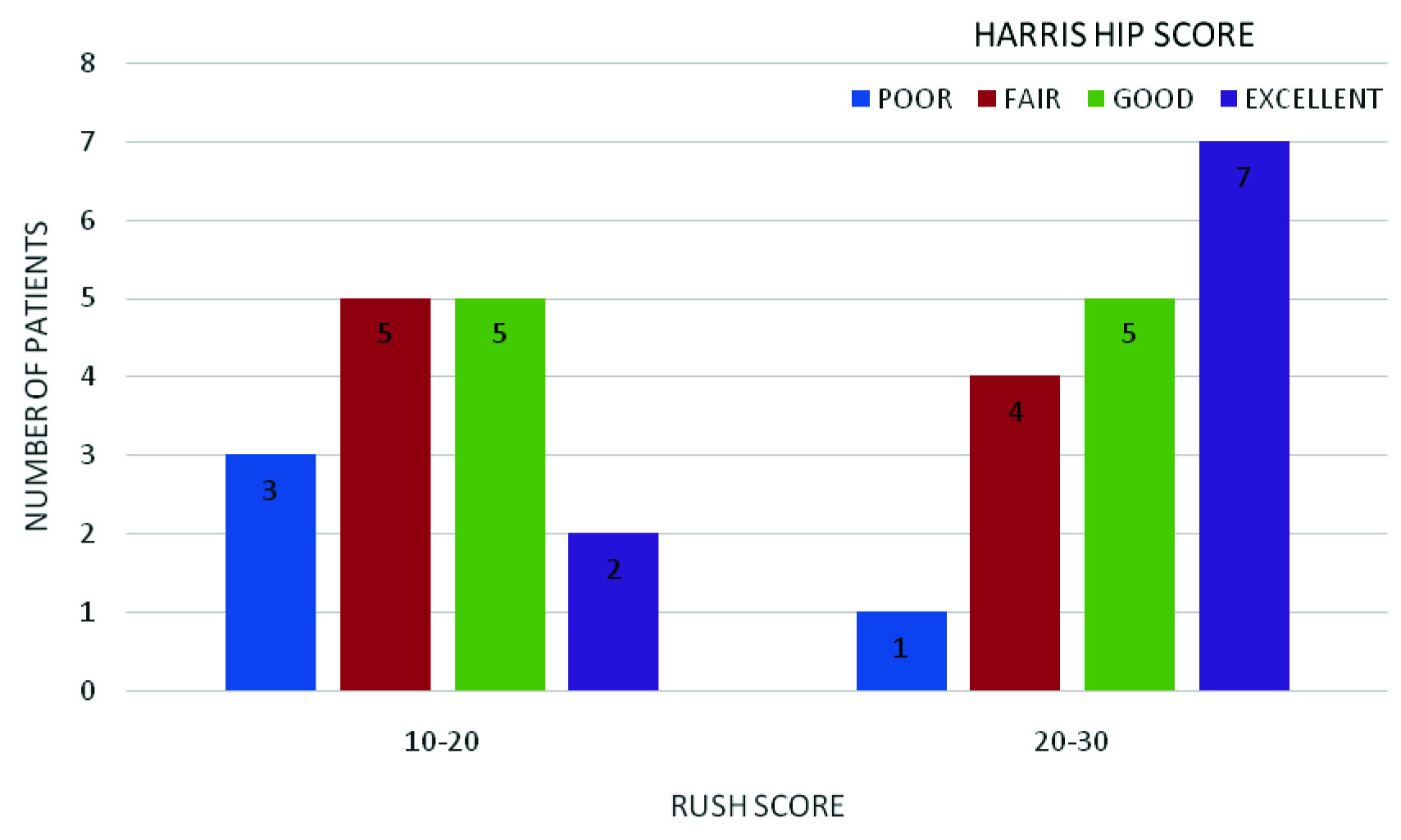
Seven of the 32 patients were under 50years of age and 25 of them were over 50years of age. Fourteen patients of the 32 patients were females and 18 were males. Sixteen patients who presented to us were of Evan Jensen class II type intertrochanteric fractures and 16 were of Evan Jensen class III. Fifteen patients had a RUSH score of 10-20 and 17 patients had a score of 20-30. The RUSH score had a mean of 21.03± 2.132 points. Nine of the 32 patients had excellent results as per the Harris hip score, 10 patients had good results, nine had fair and four had poor results [Table/Fig-5]. On comparison of the Harris hip score with the RUSH score: In the interval between 10-20 points, of the 15 patients; two patients had excellent results, five had good, five had fair and three had poor results. Of the 17 patients in the interval between 20-30 points seven patients had excellent, five had good, four had fair and one patient had poor results [Table/Fig-6]. No postoperative complications such as infection, scar dehiscence, implant failure, re-fracture, mal-union, non-union, requirement of re-surgery etc., were noted in our series.
Bar graph showing the distribution of patients as per the Harris hip score at the end of six months. Nine of the 32 patients (28%) were noted to have excellent results. Ten patients (31%) had good results. Nine patients had fair (28%) and four patients (13%) had poor results.
Bar graph showing the comparison between RUSH score and the Harris hip score. It was noted that in the interval between 10-20 points of the RUSH score two had excellent, five had good, five had fair and three patients had poor results. In the interval between 20-30 points, seven patients had excellent, five had good and four had poor results.
Discussion
The use of intra-medullary devices has increased over the years [15]. There have been many reports which suggest that they do not show better outcomes than the DHS especially in AO/OTA 31A1 (A1) and A2 fractures [6,16]. The advantage of a DHS is a steep learning curve and better exposure of fracture site [15,16], but, failures have been noted in unstable intertrochanteric fractures, which is primarily due to posterolateral wall fractures [17,18]. A biomechanical study reported that the TSP had the ability to resist femoral medialization which was comparable to the abilities of the intramedullary devices [19].
In present study, 83.3% of the patients were over 50 years of age. These results were comparable to Ashok and colleagues [20] who reported 94.2% of their patients were above 50 years of age. Further, 56.25% of patients in the present study were males and 43.75% were females. These results were comparable to Ashok and colleagues [20] who reported 66.7% of their patients were males and 33.3% were females.
Chiavras et al., developed the RUSH scoring system for assessing and grading the radiographic union of hip fractures after fixation [12]. All the patients in the current study had RUSH scores of 10-30 points. Nobody had a score less than 10 points. Majority of the patients (17 of the 32) reported a range between 20-30 points which was indicative that the rate of fracture union was high. The functional outcome of the hip in majority of the patients were noted to have excellent to good results. This was comparable to the series by Gupta et al., who concluded that supplementation of DHS with a TSP brought about overall improvement in functional and radiological outcome of hip with unstable intertrochanteric fractures. They also reported that the TSP provided a stable construct with maintenance of the lever arm with adequate abductor strength [10].
Hsu et al., in their series concluded that the use of TSP reduced the reoperation rate after fixation of unstable intertrochanetric fractures with posterolateral wall fractures. They also concluded that the use of DHS and TSP for fixation of type A2 intertrochanteric fractures reduced incidence of postoperative lateral wall fractures, decreased lag screw sliding distances and re-operation rates [7]. Babst et al., in their series concluded that addition of the TSP to the DHS construct provided additional stability with prevention of rotation of the head-neck fragment. They also concluded that the additional buttressing effect prevents lateralization of the greater trochanter. TSP provided a sound solution for fixation of these unstable intertrochanteric fractures [5].
A biomechanical study by Bong and colleagues reported that the use of TSP had the ability to avoid femoral medialization comparable to those of intramedullary devices [19]. Matre and colleagues concluded that selective use of TSP improved functional outcomes of the hip [21].
Madsen et al., in their study on comparison of DHS with TSP versus Gamma nails for management of unstable intertrochanteric fractures, concluded that use of the TSP avoided medialization of the distal fracture and chances of femoral shaft fractures during Gamma nail insertion was avoided. They also concluded that there was reduced lag screw sliding distance in the cases operated with DHS and TSP [9].
Limitation
The major limitation of the study was that we had to use Singh’s index as a marker for osteoporosis when DEXA scan is the gold standard. As the patients who presented to us were from a poor economic background, they could not afford a DEXA scan; hence, Singh’s index was used as a marker.
Conclusion
DHS with TSP fixation of unstable intertrochanteric fractures of femur is an effective technique and has excellent functional and radiological outcomes with minimal complication and early rehabilitation rates.
[1]. Johnell O, Kanis JA, An estimate of the worldwide prevalence, mortality and disability associated with hip fractureOsteoporos Int 2004 15(11):897-902. [Google Scholar]
[2]. Randell AG, Nguyen TV, Bhalerao N, Silverman SL, Sambrook PN, Eisman JA, Deterioration in quality of life following hip fracture: a prospective studyOsteoporos Int 2000 11:460-66. [Google Scholar]
[3]. Zuckerman JD, Current concepts: hip fractureN Engl J Med 1996 334(23):1519-25. [Google Scholar]
[4]. Kulkarni GS, Limaye R, Kulkarni M, Kulkarni S, Intertrochanteric fracturesIndian J Orthop 2006 40:15-23. [Google Scholar]
[5]. Babst R, Renner N, Biedermann M, Rosso R, Heberer M, Harder F, Clinical results using the trochanter stabilizing plate (TSP): the modular extension of the dynamic hip screw (DHS) for internal fixation of selected unstable intertrochanteric fracturesJ Orthop Trauma 1998 12:392-99. [Google Scholar]
[6]. Parker MJ, Pryor GA, Gamma versus DHS nailing for extracapsular femoral fractures. Meta-analysis of ten randomised trialsInt Orthop 1996 20:163-68. [Google Scholar]
[7]. Hsu CE, Chiu YC, Tsai SH, Lin TC, Lee MH, Huang KC, Trochanter stabilising plate improves treatment outcomes in AO/OTA 31-A2 intertrochanteric fractures with critical thin femoral lateral wallsInjury, Int. J. Care Injured 2015 46:1047-53. [Google Scholar]
[8]. Su ET, DeWal H, Kummer FJ, Koval KJ, The effect of an attachable lateral support plate on the stability of intertrochanteric fracture fixation with a sliding hip screwJ Trauma 2003 55:504-08. [Google Scholar]
[9]. Madsen JE, Naess L, Aune AK, Alho A, Ekeland A, Stromsoe K, Dynamic hip screw with trochanteric stabilizing plate in the treatment of unstable proximal femoral fractures: a comparative study with the Gamma nail and compression hip screwJ Orthop Trauma 1998 12:241-48. [Google Scholar]
[10]. Gupta RK, Sangwan K, Kamboj P, Punia SS, Walecha P, Unstable trochanteric fractures: the role of lateral wall reconstructionInt Orthop 2010 34:125-29. [Google Scholar]
[11]. Koot VCM, Kesselaer SMMJ, Clevers GJ, De Hooge P, Weits T, Werken CVD, Evaluation of the singh index for measuring osteoporosisJ Bone Joint Surg [Br] 1996 78B:831-34. [Google Scholar]
[12]. Chiavras Mary M, Bains S, Choudur H, Parasu N, Jacobson J, Ayeni O, The Radiographic Union Score for Hip (RUSH): the use of a checklist to evaluate hip fracture healing improves agreement between radiologists and orthopaedic surgeonsSkeletal Radiol 2013 42:1079-88. [Google Scholar]
[13]. Harris WH, Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluationJ Bone Joint Surg Am 1969 51(4):737-55. [Google Scholar]
[14]. Marchetti P, Binazzi R, Vaccari V, Girolami M, Morici F, Impallomeni C, Long-term results with cementless Fitek (or Fitmore) cupsJ Arthroplasty 2005 20(6):730-37. [Google Scholar]
[15]. Kokoroghiannis C, Aktselis I, Deligeorgis A, Fragkomichalos E, Papadimas D, Pappadas I, Evolving concepts of stability and intramedullary fixation of intertrochanteric fractures: a reviewInjury 2012 43:686-93. [Google Scholar]
[16]. Barton TM, Gleeson R, Topliss C, Greenwood R, Harries WJ, Chesser TJ, A comparison of the long gamma nail with the sliding hip screw for the treatment of AO/OTA 31-A2 fractures of the proximal part of the femur: a prospective randomized trialJ Bone Joint Surg Am 2010 92:792-98. [Google Scholar]
[17]. Palm H, Jacobsen S, Sonne-Holm S, Gebuhr P, Integrity of the lateral femoral wall in intertrochanteric hip fractures: an important predictor of a reoperationJ Bone Joint Surg Am 2007 89:470-75. [Google Scholar]
[18]. Hsu CE, Shih CM, Wang CC, Huang KC, Lateral femoral wall thickness. A reliable predictor of postoperative lateral wall fracture in intertrochanteric fracturesBone Joint J 2013 95–B:1134-38. [Google Scholar]
[19]. Bong MR, Patel V, Iesaka K, Egol KA, Kummer FJ, Koval KJ, Comparison of a sliding hip screw with a trochanteric lateral support plate to an intramedullary hip screw for fixation of unstable intertrochanteric hip fractures: a cadaver studyJ Trauma 2004 56:791-94. [Google Scholar]
[20]. Ashok TR, Ram GG, Thamodharan B, Perumal S, Survival of Dynamic Hip Screw in Unstable Intertrochanteric FracturesIOSR Journal of Dental and Medical Sciences 2013 9(6):13-16. [Google Scholar]
[21]. Matre K, Havelin LI, Gjertsen JE, Espehaug B, Fevang JM, Intramedullary nails result in more reoperations than sliding hip screws in two-part intertrochanteric fracturesClinic Orthop Relat Res 2013 471:1379-86. [Google Scholar]