Venous cannulation is often performed without any analgesia, even though the pain associated with this procedure is very distressing. Pain and fear associated with this seemingly trivial procedure, assumes disproportionate magnitude sometimes; this may increase the level of stress experienced by patients in the peri-operative setting. A survey of expert anaesthesiologists concluded that discomfort from intravenous catheter insertion ranked fifth among the 33 low morbidity clinical outcomes when both clinical importance and frequency were considered [1].
Various pharmacological and non-pharmacological measures have been studied, with variable results, to minimize venous cannulation pain [2–6]. The analgesic property of volatile anaesthetic agents at various concentrations has been investigated extensively with variable results. In addition, topical application of volatile agents has been found to attenuate the response to a mechanical stimulus [7]. The role of topical application of volatile agents in attenuating venous cannulation pain has not been investigated so far.
We therefore planned this study to evaluate and compare the efficacy of topically administered volatile anaesthetic agents for attenuating venous cannulation pain.
Materials and Methods
This prospective, randomized and double blind clinical study was designed to include 120 adult patients (20-60yrs of age) of either sex and ASA physical status I or II, scheduled for elective surgical procedures and was carried out between November 2015 and January 2016. The study protocol was approved by the institutional ethical committee and written informed consents were obtained from all the patients.
Exclusion criteria was: Subjects allergic to cotton or adhesive dressing, metal or plastic, with acute or chronic pain conditions, consuming analgesics, calcium channel blocker or beta blocker within one month of recruiting, and abnormal skin conditions such as infection at the site of proposed venous cannulation, cold hypersensitivity, scars and eczema, peripheral neuropathy.
Patients were randomly allocated according to a computer generated table of random numbers, into 4 groups of 30 patients each.
Three volatile anaesthetic agents, halothane (Raman and Weil Pvt. Ltd, Bombay, India), isoflurane (Baxter, Puerto Rico, USA) and sevoflurane (Abbott, Kent, UK), at equipotent doses of 1 ml, 1.5 ml and 2.7 ml were evaluated for the attenuation of venous cannulation pain; in the placebo group 2.5 ml of sterile water was used. The volumes of volatile agents were chosen to be equipotent in terms of their Minimal Alveolar Concentration (MAC) as already described [7].
The study drug was applied in the preoperative ward with the patient in a sitting position and forearm placed on a table exposing the volar surface. A suitable vein in the middle of the volar surface of the forearm was identified and marked. This area of the forearm was covered with a cotton band. An independent anaesthesiologist, not taking part in the study, loaded the study drug in 5 ml syringes with the anaesthetic agent or sterile water and labeled it with a code number which was decoded at the end of the study. Another anaesthesiologist, blinded to the study drug, administered it in the space between the volar surface of the forearm and cotton band. This area of the forearm was covered with aluminum foil and wrapped with bandages and plastic film from the wrist to the elbow joint. All layers were fixed with tape around the elbow and wrist, with the elbow joint left free.
After 30 minutes, all the coverings were removed and venous cannulation was performed on the volar surface of the forearm, with 18 G intravenous cannula by an anaesthesiology registrar who was unaware of group distribution. Patients whose veins could not be cannulated successfully on the first attempt were considered as drop outs. After 30 min when the wrappings were removed the skin of the forearm was dry and the amount of administered volatile anaesthetics agents was low to produce any degree of sedation that would have interfered with VAS score.
The primary outcome measure included incidence of pain upon venous cannulation. Secondary outcome measures included VAS score (0-100mm; 0 = no pain and 100 = worst imaginable pain) for the severity of pain upon venous cannulation and skin reactions like blanching, erythema or swelling at the cannulation site. Clinical assessment of patients for these outcome measures was done for the first 24 hours after venous cannulation by an independent investigator, unaware of patient randomization.
Assuming that there would be a 30% reduction in the incidence of venous cannulation pain following therapy one would need to include 25 patients in each group for results to be significant (with α = 0.05 and β = 0.80). We enrolled 30 patients in each group to account for potential dropouts or protocol violations.
Statistical Analysis
Demographic data were analysed by one-way ANOVA for continuous variables and chi square test for categorical variables. The Fisher’s exact test was used to compare incidence of venous cannulation pain and skin reactions between the groups. The VAS pain scores between groups were compared using the Kruskal-Wallis test (non-parametric ANOVA). If Kruskal-Wallis test was significant, Dunn’s multiple comparison tests was used to compare different groups. Statistical analysis was performed using the Graph pad prism 6.0 statistical software. A p-value of <0.05 was considered statistically significant.
Results
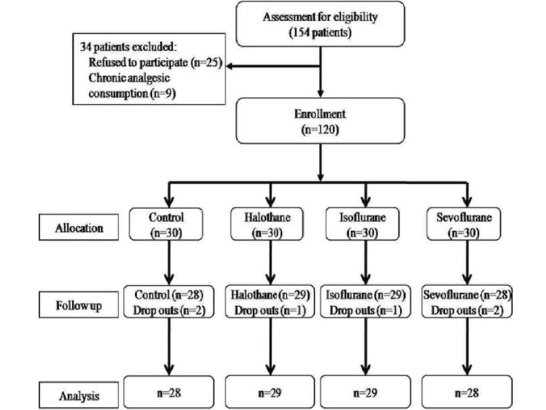
A total of 154 patients were assessed for eligibility, out of which 120 patients were included in the study after randomization and 114 patients (95%) completed the study [Table/Fig-1]. Thirty four patients were not included in this study on account of patient’s refusal (25 patients) and history of chronic analgesic consumption (9 patients). Six patients were excluded from the study following initial randomization on account of cannulation failure in the first attempt; their data has been included in the comparison of demographic profiles, however, they were not subjected to further statistical analysis [Table/Fig-1]. There was no significant difference amongst the groups with regard to demographic variables (p>0.05) [Table/Fig-2].
| Variables | Control | Halothane | Isoflurane | Sevoflurane | p-value |
|---|
| (n=30) | (n=30) | (n=30) | (n=30) |
|---|
| Age (Yrs) | 38.23±11.92 | 42.70±10.18 | 40.87±12.13 | 41.20±9.65 | 0.469 |
| Weight (Kg) | 56.23±9.024 | 55.13±11.65 | 58.93±10.57 | 59.60±11.52 | 0.319 |
| Male/Female | 17/13 | 17/13 | 15/15 | 16/14 | 0.585 |
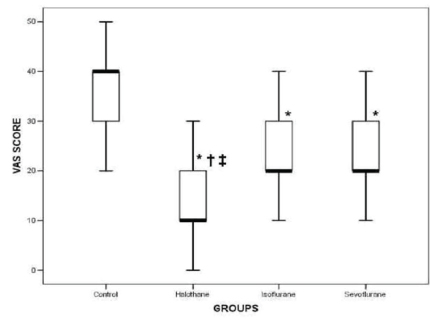
A significant reduction in the incidence of venous cannulation pain was observed in the halothane (79%) group as compared to control (100%; p<0.05), isoflurane (100%; p<0.05) and sevoflurane (100%; p<0.05) groups. The severity of venous cannulation pain as assessed by median (interquartile range, Q1-Q3) VAS scores was reduced in the halothane {10 (10-20); p<0.001}, isoflurane {20 (10-30); p<0.001} and sevoflurane {20 (20-30); p<0.001} groups as compared to the control group {40 (30-40)}; VAS scores in the halothane group were significantly reduced as compared to isoflurane (p<0.05) and sevoflurane (p<0.05) groups [Table/Fig-3]. There was no significant difference of VAS scores in between isoflurane and sevoflurane group (p>0.05). None of the patients in any group developed blanching, erythema or swelling at the site of venous cannulation.
Venous cannulation pain as assessed by VAS. Data are presented as medians with interquartile ranges (Q1-Q3). The boxes extend from the 25th percentile (Q1) to the 75th percentile (Q3) of VAS scores in each group, and the dark line represents the median score. * p<0.05 during intergroup comparison of control with other groups. 𠈂 p<0.05 during intergroup comparison of halothane with isoflurane.
‡ p<0.05 during intergroup comparison of halothane with sevoflurane.
Discussion
We observed that topical application of halothane is effective in reducing both the incidence and severity of venous cannulation pain; however, topical application of isoflurane and sevoflurane only minimized the severity of venous cannulation pain.
The potency of volatile anaesthetics has been defined by the MAC concept [8]; however the MAC concept does not distinguish between the different components of anaesthesia i.e., hypnosis, analgesia and neuromuscular block. Several studies have studied the antinociceptive effect of the volatile anaesthetics with contrasting results. Petersen-Felix et al., reported that isoflurane at high concentrations depresses the nociceptive reflex to repetitive stimuli [9]. However, sub-anaesthetic concentrations of isoflurane had no effect on the responses to heat, cold or mechanical pressure [10]. Nonetheless, a depression of the nociceptive reflex to single electrical stimulation was demonstrated in both these studies [9,10]. Zhang et al., reported that 0.1 MAC of halothane, isoflurane, nitrous oxide or diethyl ether produced hyperalgesia in rats, but at 0.4 to 0.8 MAC produced analgesia to a thermal stimulus [11].
Evaluation of the possible anti-nociceptive properties of general anaesthetics in humans is complex as concurrent central depression may interfere with the assessment of the potential of an analgesic effect. In all the above mentioned clinical trials volatile anaesthetics have been administered via the lungs; hence their analgesic effect is difficult to distinguish from the concomitant sedation which they produce. In order to minimize the influence of central depression and/or sedation on antinociceptive effect, clinical trials have investigated the effects of topically administered volatile anaesthetics; two such clinical trials have reported antinociceptive effects of topically applied volatile anaesthetics following mechanical and/ or electrical stimulus [7,12].
The method adopted in the present study, as described previously [7,12], allows evaluation of possible analgesic effects of volatile anaesthetics with no or minimal involvement of central depression and sedation. We allowed a 30 min period of exposure of the skin to volatile agents, as the maximal rate of percutaneous loss of three volatile anaesthetics (halothane, isoflurane and desflurane) was observed after 30 min of inhalation [13]. It has been proposed that anaesthetic action of volatile agents in a tissue compartment depends on its partial pressure in that compartment [14]. Furthermore the potential of an analgesic effect produced by inhalational anaesthetics is consistent with the findings of Rehberg et al., who reported suppression of central nervous system sodium channels by clinical concentrations of volatile anaesthetics [15]. Suppression of sodium currents should lead to an elevation in neuronal firing threshold [16], and volatile anaesthetics at clinical concentrations have been shown to elevate the threshold potential of neurons [17]. If these results apply to the primary afferent fibers, then an effective partial pressure of the volatile anaesthetic on the skin may suppress the neuronal excitability and/or conductance giving rise to the antinociceptive effect.
Calcium channels may also play a role. Isoflurane and halothane suppress the current of T-calcium channels in the dorsal root ganglion neurons and in the adrenal glomerulosa cells [18]. Excitatory synaptic transmission involves calcium T-channels, which may be suppressed by volatile anaesthetics. Inhalational anaesthetics also activate subunits of voltage dependent potassium channels. The increased conductance of potassium channels results in less excitable neurons and may provoke changes in voltage gated sodium channels [19]. Recently, adenosine triphosphate sensitive potassium channels have been discovered in mammalian primary afferent neurons [20]. The attenuated response to a painful stimulus produced by volatile anaesthetics in this study may involve an action on the sodium, potassium, and/or calcium channels.
In the present study, we observed that topical application of volatile anaesthetics is effective in reducing the severity of venous cannulation pain. Halothane was found to be most efficient in this regard along with its capability of reducing the incidence of venous cannulation pain. A possible explanation for this is the high lipid solubility of halothane, therefore, its better penetration through the tissues. Hence differences in the solubility of the volatile anaesthetics, most likely contributed to a more pronounced effect of halothane as compared to the equipotent volumes of isoflurane and sevoflurane.
The results of the present study differ from those of a previous study [7] in which same volumes of isoflurane and sevoflurane were found to be ineffective in reducing the response to a mechanical stimulus. The possible explanation is the use of median values of VAS in the present study as compared to the mean values of VAS in the previous study along with differences in the nature of stimulus whose response was evaluated in the previous study.
Use of local anaesthetic as infiltration or topical administration have been found to be effective and time tested technique for pain relief to noxious stimuli, though associated with needle prick, blanching of the skin or vasoconstriction and methaemoglobinemia [2,4,6]. The glycerol trinitrate ointment application is associated with hypotension and headache [21]. Our study has demonstrated that pain due to venous cannulation can be effectively blocked by local application of volatile anaesthetics. Similarly the cost incurred for the same is small and varies between 1 $ to 1.5 $. The absence of serious side effects, non-invasiveness and easy availability of volatile anaesthetic agents in operation theatre makes it an attractive alternative choice for this study.
Limitation
A strong possibility exists that volatile anaesthetics are absorbed from the skin into the blood. Since no breath analysis for volatile agents was done, even in the absence of sedation, a combined peripheral and central effect cannot be ruled out. In addition skin might be cooled by evaporation of isoflurane and/or water so contributing to VAS changes. However, the possibility of evaporation was limited as the skin area tested was not exposed to air immediately after isoflurane or water application but isoflurane or water were readily absorbed by cotton. Moreover, 30 min later when the wrappings were removed the skin of the forearm was dry.
Conclusion
It can be concluded that topical application of equipotent volumes of halothane, isoflurane and sevoflurane were effective in reducing the severity of venous cannulation pain; halothane was found to be most proficient in this regard along with a reduction in the incidence of venous cannulation pain.