Bilateral Renal Lymphangiectasia
Vaidehi K Pandya1, Maulin K Shah2, Shruti P Gandhi3, Himanshu V Patel4
1 Assistant Professor, Department of Radio Diagnosis and Imaging, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre (IKDRC) & Dr.H.L. Trivedi Institute of Transplantation Sciences (ITS), Gujarat, India.
2 Resident, Department of Nephrology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre (IKDRC) & Dr.H.L. Trivedi Institute of Transplantation Sciences (ITS), Gujarat, India.
3 Associate Professor and In-Charge, Department of Radio Diagnosis and Imaging, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre (IKDRC) & Dr.H.L. Trivedi Institute of Transplantation Sciences (ITS), Gujarat, India.
4 Professor, Department of Nephrology, G.R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre (IKDRC) & Dr.H.L. Trivedi Institute of Transplantation Sciences (ITS), Gujarat, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Vaidehi K Pandya, Assistant Professor, Department of Radio Diagnosis and Imaging, G. R. Doshi and K.M. Mehta Institute of Kidney Diseases & Research Centre (IKDRC)- Dr. H. L. Trivedi Institute of Transplantation Sciences (ITS), Civil Hospital Campus, Asarwa, Ahmedabad - 380016, Gujarat, India.
E-mail: vaidehi_pandya2002@yahoo.com
Renal Lymphangiectasia (RLM) is very rare benign lymphatic malformation. It can be misdiagnosed for other cystic renal masses, most commonly polycystic kidneys. Though incidentally found in most cases, it may be the cause for hypertension and renal failure in undiagnosed patients. Here, we report a case of an adult asymptomatic male with bilateral RLM which was detected as an incidental finding on ultrasound. Confirmation by CT-scan and laboratory diagnosis of aspirated fluid was done, and patient was managed conservatively.
CT scan, Polycystic kidneys, Ultrasound
Case Report
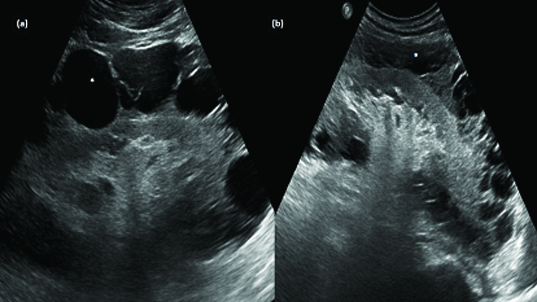
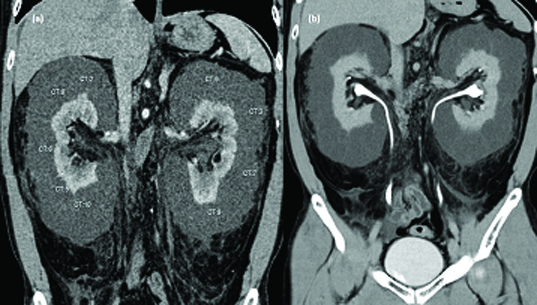
A 34-year-old healthy asymptomatic man was referred to our institute with nonspecific vague complains like heaviness in flanks and occasional low grade flank pains. He was diagnosed as having bilateral polycystic kidneys in other center and was referred to our center for further management. On evaluation at our center, he had no significant medical or family history. There was no positive history of infection or trauma. Clinical and physical examination were within normal limits. Blood pressure was 120/86 mmHg. Urinalysis was normal. Serum creatinine was within normal limits. Ultrasound revealed normal sized kidneys with increased echo texture and preserved cortico-medullary differentiation. Bilateral kidneys showed multi septated anechoic collections in perinephric regions of maximum width of 33mm [Table/Fig-1]. No evidence of calculus or hydronephrosis was seen on either side. Rest of the abdominal ultrasound was unremarkable. Based on imaging findings, provisional diagnosis of bilateral Renal Lymphangiectasia (RLM) was thought of and CT-scan was performed on Siemens Somatom 64 Slice CT scanner with non-iodinated contrast. CT scan revealed multi-septated collections with typical fluid density (0 to 10 HU) in perinephric regions of both kidneys [Table/Fig-2]. No evidence of soft tissue or fat density mass lesion was seen. Both kidneys showed normal parenchymal enhancement and contrast excretion with no evidence of contrast leakage within the perinephric collections. Both ureters were normal in course and caliber. Further, the perinephric fluid collection was aspirated and laboratory investigation showed total leucocyte count of 55/cmm, out of which 85% were lymphocytes; protein level of 550mg/dl, normal glucose level and increased triglycerides and no organism was found on culture and sensitivity test, which confirmed the diagnosis.
Gray scale ultrasound image of right kidney: (a) and left kidney; (b) showing multi septated anechoic collection (asterisk) in perinephric region with increased renal cortical echo texture.
(a) Cortico-medullary phase of CT scan Abdomen in coronal plane showing multi septated non-enhancing Collection with average HU density 0 to 10 HU; (b) MPR reformation of Coronal plane of delayed phase of CT scan abdomen showing normal excretion of contrast.
Discussion
RLM accounts for approximately 1% of all lymphangiomas [1]. It is very rarely reported benign condition of lymphatic malformation where dilated peri-renal lymphatics are seen. The main causative factor is non-communication of peri-renal and peri-pelvic lymphatic channels with the main lymphatics [2]. It has been reported in adults as well as in children of both sexes [3,4]. It may be unilateral or bilateral and focal as well as diffuse [5–7]. Various spectrum of causes may include familial, developmental and acquired causes. Mostly asymptomatic, it may show nonspecific symptoms and is diagnosed by typical imaging findings. It is also known as renal lymphangiomatosis, hygroma renale and polycystic disease of the renal sinus [2,8,9]. Usually, the renal lymphatic ducts drain in to larger retroperitoneal lymphatics. Failure of such drainage leads to dilatation of these ducts and formation of unilocular or multilocular collections in perinephric spaces or pelvic sinuses [9]. Familial predilection is seen in few reported cases [2]. Most commonly the condition is asymptomatic and is diagnosed incidentally. It may have nonspecific presentation like flank pains, abdominal distension, haematuria, fever, hypertension or altered renal functions [8,9]. The symptoms can be aggravated by pregnancy [2].
Two patterns are recognized in the renal sinus. One of them originates into intraparenchymal renal sinus region, known as peripelvic RLM and the other one originates in the medial renal parenchyma and encroach in the renal sinus which are called parapelvic RLM. Both appear same on imaging. If radiological and pathological correlations data are not available; both are commonly described as “cystic lesion of the renal sinus” [10].
In asymptomatic cases also, imaging studies give a striking clue to the diagnosis. Ultrasound studies reveal normal sized or enlarged kidneys with increased parenchymal echo texture and loss of cortico medullary differentiation. Multi septated thin walled fluid collections are seen in perinephric or peri-pelvic regions [7]. On CT-scan, RLM appears as a well-defined fluid attenuation multi septated collections in perinephric or peri-pelvic regions with normal renal parenchymal enhancement. No evidence of invasion of other organs is seen by such collection. Presence of fluid or fluid filled spaces in the retro-peritoneum in close vicinity of great vessels as well as crossing the midline at the level of renal vessels is diagnostic sign of RLM [3]. These are the dilated renal lymphatics which drain in to larger retroperitoneal lymphatics. In addition to typical imaging features, the confirmation of diagnosis is done by fluid aspiration and cytology of aspirated fluid. Thus, we can exclude the presence of urinoma and infective etiology. High levels of renin in the aspirated fluid confirms the origin to be renal.
Most common differential diagnosis are polycystic kidneys and hydronephrosis [11,12]. In polycystic kidneys, the renal cortex shows presence of cysts whereas in RLM, the renal cortex appears normal. Similarly in RLM, the pelvicalyceal system appears normal in contrast to hydronephrosis. Other renal masses like nephroblastomatosis, lymphoma and multilocular cystic nephroma are also included in differentials. If RLM involves small intra renal lymphatics, the lesion appears as a small solid renal lesion or shows slight diffuse kidney enlargement and no internal cystic spaces. In such cases differentiation from nephroblastomatosis and lymphoma appears difficult. They can be differentiated from RLM on CT-scan as all of them involve the renal parenchyma whereas nephroblastomatosis and lymphoma are solid in attenuation in contrast to fluid attenuation of RLM [3,10,13].
The aspirated fluid is sterile, chylous fluid containing majority of lymphocytes (more than 80-90%), small amount of fat. The contents of renal lymphatic aspirates differs from that of thoracic duct contents because it is outside the mesenteric drainage pathway [13,14].
Untreated cases can be complicated by haematuria, ascites, hypertension, renal vein thrombosis or altered renal function [8,14–16]. Pain on account of compression due to presence of collection, is usually relieved by percutaneous aspiration of fluid. However, hypertension and altered renal function improves after conservative treatment [3,8]. Asymptomatic patients receive conservative management but symptomatic large collections are treated by mar-supialisation or nephrostomy [8]. Anti-hypertensive drugs can be used in hypertensive patients for symptomatic relief. Page kidney and renal vein thrombosis are complications where nephrectomy is done as a treatment [10].
Conclusion
Renal Lymphangiectasia is a very rarely seen benign usually asymptomatic condition where imaging studies can play a very important role in differentiation from other conditions. Also, it can help in determining the extension of the fluid collection and reduces the morbidity associated with it. In difficult cases, aspiration of fluid can confirm the diagnosis and can avoid the unnecessary surgical interventions with their associated complications.
[1]. Hauser H, Mischinger HJ, Beham A, Berger A, Cerwenka H, Razmara J, Cystic retroperitoneal lymphangiomas in adultsEur J Surg Oncol 1997 23(4):322-26. [Google Scholar]
[2]. Meredith WT, Levine E, Ahlstrom NG, Grantham JJ, Exacerbation of familial renal lymphangiomatosis during pregnancyAJR Am J Roentgenol 1988 151:965-66. [Google Scholar]
[3]. Ramseyer LT, Case 34: Renal lymphangiectasiaRadiology 2001 219:442-44. [Google Scholar]
[4]. Leder RA, Frederick MG, Hall BP, Renal lymphangiomatosisAJR 1995 165:197-200. [Google Scholar]
[5]. Merguerian PA, Sargent SK, Dunn JL, Unilateral lymphangiectasis of the kidney: an unusual cause of renal enlargement in an infantJ Urol 1995 153(2):447-49. [Google Scholar]
[6]. Gupta R, Sharma R, Gamanagatti S, Dogra PN, Kumar A, Unilateral renal lymphangiectasia: imaging appearance on sonography, CT and MRIInt Urol Nephrol 2007 39(2):361-64. [Google Scholar]
[7]. Varela JR, Bargiela A, Requejo I, Fernandez R, Darriba M, Pombo F, Bilateral renal lymphangiomatosis: US and CT findingsEur Radiol 1998 8(2):230-31. [Google Scholar]
[8]. Schwarz A, Lenz T, Klaen R, Hygroma renale: Pararenal lymphatic cysts associated with rennin-dependent hypertension (Page kidney). Case report on bilateral cysts and successful therapy by marsupializationJ Urol 1993 150:953-57. [Google Scholar]
[9]. Davidson AJ, Hartman DS, Lymphangioma of the retroperitoneum: CT and sonographic characteristicsRad 1990 175:507-10. [Google Scholar]
[10]. Jorge MR, Juan LA, Natalia AS, Melissa UV, Mauricio M, Renal Lymphangiectasia. MDCT and MRI findingsRev Colomb Radiol 2011 22(3):1-8. [Google Scholar]
[11]. Ashraf K, Raza SS, Ashraf O, Memon W, Memon A, Zubairi TA, Renal lymphangiectasiaBr J Radiol 2007 80:e117-18. [Google Scholar]
[12]. Sarikaya B, Akturk Y, Bekar U, Topaloglu S, Bilateral renal lymphangiomatosis mimicking hydronephrosis: Multidetector CT urographic findingsAbdom Imaging 2006 31(6):732-34. [Google Scholar]
[13]. Kim JK, Ahn JH, Kim KR, Cho KS, Renal Lymphangioma manifested as a solid mass on ultrasonography and computed tomographyJ Ultrasound Med 2002 21:203-06. [Google Scholar]
[14]. Amir Ahmad N, Legha L, Mehrdad B, Arda K, Shirin H, IladAlavi D, Renal lymphangiectasia: A curious Cause of Pleural EffusionTanaffos 2015 14(3):213-16. [Google Scholar]
[15]. Riehl J, Schmitt H, Schafer L, Schneider B, Sieberth G, Retroperitoneal lymphangiectasia associated with bilateral renal vein thrombosisNephrol Dial Transplant 1997 12(8):1701-03. [Google Scholar]
[16]. Chang MS, Yang DM, Yoon MH, Kim HS, Jin W, Lee JB, Peripelvic and perirenal lymphangiectasia and bilateral renal vein thrombosis: a case reportJ Korean Radiol Soc 2000 43(1):91-94. [Google Scholar]