A majority of acute infections after compound fractures are due to hospital acquired pathogens in a landmark prospective study by Gustilo and Anderson conducted on 326 open fractures it was reported that most of the infections develop secondarily [1]. A study by Patzakis et al., has reported that barely 18% of acute infections following compound fractures were due to the same pathogen as reported in the prior perioperative cultures [2]. This phenomenon of hospital acquired bacteria and their prominent role in the pathogenesis of infection emphasizes the importance of a strict protocol for in-hospital management. A recent concept review article [3] published by Fletcher N et al., in JBJS reviewed the evidence in favour of do’s and don’ts to control perioperative infections. Studies have focussed on individual measures to prevent infection. These include the use of local antibiotics 4G tobramycin /70 Gm bag of cement beads wherever there is dead space in bones [3], use of first generation cephalosporins as the first choice preoperative antibiotic to be given 1 hour prior to surgery [4], repetition of the dose of antibiotic if duration of surgery exceeds 2 hours or the half-life of the antibiotic [5], avoidance of hair removal [6], scrubbing with chlorhexidine [7], occlusive drapes [8], solution used for irrigation [9], use of surgical drains [10], subcuticular wound closure over skin closure [11], three layered dressing [12] and use of ultraviolet light in operation theatre [13] of preventing infections in compound fractures. However there is no study in literature that has studied the combined effect of individual measures outlined above.
The present management of compound fractures at King George’s Medical University (KGMU), Lucknow-India, represents the conventional practice of managing compound fractures in India and is an appropriate control for trial against a protocol that combines measures that are supported in literature. The aim was to compare the conventional protocol with a protocol that combined evidence based measures (EBP – Evidence Based Protocol) and measure the impact in terms of important measurable outcomes like time taken for the wound culture to become negative and time taken for wound to heal by secondary intention (wound size or days it took to epithelialize).
Materials and Methods
Patients of Gustillo Anderson [14] Grade I and II compound fractures both bone leg, age between 12 years and 70 years of either sex, reporting to OPD or the emergency of Department of Orthopaedics at King George Medical University trauma centre were enrolled in the study, subject to written informed consent. Gustillo Anderson grade III fractures were excluded from the study as they require flap covers quite frequently and we were looking at the natural secondary healing of wound. Factors known or likely to interfere with fracture or soft tissue healing like extremes of age (< 12 years or > 70 years), patients with systemic diseases like – Diabetes, HIV, anaemia, compound fractures with bone loss, polytrauma/shock/injury to other organs, elsewhere managed cases and duration of injury > 3 days were also excluded from the study. All procedures followed were in accordance with the ethical guidelines for biomedical research on human participants published by Indian Council of Medical Research [15].
With the minimum risk of positive culture to be ½ of risk in controls in the experimental group, a 17% infection rate in unexposed (reported in a paper published by D’Souza A et al., [16]), α error of 0.05 and β error of 0.20 we need 113 patients in the experimental group and 113 in the control group. This sample size was obtained using the Epi info software version 3.5.4.
A random number table was generated using the “=RAND ()*226” command in Microsoft XL. This random number table was used to allocate patients fulfilling the inclusion criteria to the conventional and EBP groups. Patients fulfilling inclusion criteria were allocated on the basis of their arrival at the trauma center as per the random number table. Base line characteristics of patients and injury were recorded and compared in groups to test random allocation.
A single blind design was used as the participants were not aware as to the group to which they were allotted.
The conventional group was managed using splint, elevation, conventional antibiotic protocol being used in KGMU, scrubbing by povidone iodine solution, non-occlusive draping, wound debridement, reduction and retention of fracture by external fixator or a plaster cast and dressing the wound by betadine solution. Conventional antibiotic protocol being used at KGMU requires patients to be put on an intravenous first generation cephalosporins and aminoglycosides empirically as first line management followed by a change to an antibiotic reported to be sensitive on pus culture sensitivity report. Subsequent pus culture was repeated every week and antibiotic was decided accordingly. Antibiotics were used till patients had clinical signs of infection (erythema, swelling, discharge and increased local temperature) or erythrocyte sedimentation rate was raised. Part preparation was done using povidone iodine. Hair removal is avoided if essential clippers were used. Wound debridement was done. Deep debridement and primary coverage was attempted. However, if primary coverage was not possible wounds were allowed to heal by secondary intention. Wound was washed by 6 litres of normal saline and dressed with betadine solution. Reduction and retention of fracture was done by external fixation or a plaster cast.
EBP group was managed using – splint, elevation, avoidance of hair removal, wound debridement, reduction and retention of fracture (external fixation or a plaster cast), non-occlusive draping and use of ultraviolet light in operation theatre which were the same as those used in conventional group. The difference in the protocols in the two groups is outlined below:
Antibiotic protocol- Patients were started on an intravenous cephalosporin and an aminoglycoside at arrival. A Grade-A recommendation exists for the administration of a type-I cephalosporin for all open fractures [5]. Despite widespread use, there is currently insufficient evidence to support the use of aminoglycosides in the management of type-II and III open fractures but they were used anyway for ethical reasons as traditional teaching has asserted that coverage against gram-negative organisms is required for all type-III and perhaps some type-II fractures because of the increased contamination and higher-energy mechanism associated with these fractures [3]. Antibiotics were administered within 60 minutes prior to the incision as near to the time of the incision as possible. An additional intra-operative dose of intra venous antibiotics was used if the duration of the procedure exceeded one to two times the half-life of the antibiotic or if there was substantial blood loss during the procedure. Local Antibiotics 4G tobramycin /70 Gm bag of cement beads were used wherever there was dead space in bones. Antibiotic was changed to as per the report of subsequent culture sensitivity. Subsequent pus culture was repeated every week and antibiotic was decided accordingly. Antibiotics were used till patients had clinical signs of infection or erythrocyte sedimentation rate was raised. Chlorhexidine gluconate and alcohol scrub was rubbed on > 8” area surrounding the wound and then in the wound to render it bacteria free. Sequential irrigation using 1 litre each of Castile Soap – Saline – Benzalkonium Chloride- Saline and brush was used for cleaning of wound. No drains were used. Wounds were closed using sub-cuticular monofilament suture. A triple antibiotic ointment (bacitracin zinc, neomycin sulphate and polymixin B sulphate) was applied to the wound and a three layered occlusive dressing (non adherent hydrophilic layer, absorptive layer, and an occlusive layer) was applied. The dressing was repeated at 24 hours if not closed in a plaster cast. Beards and ears were completely covered, wrap around made of synthetic material was used, and doors remained closed and maximum of 4 times opening was permitted during the duration of surgery. Implants were kept in their packing till their time of use. Baseline characteristics recorded were age, sex, preoperative haemoglobin, site of fracture, grade of fracture, type of fracture, size of wound and duration of surgery.
Wound cultures and sensitivity were obtained till the culture became negative. Wounds were measured at weekly intervals after admission till the wound healed. The patients were discharged when the culture became negative and there were no active signs of infection present. Duration of stay at the hospital was also recorded. Thereafter, they were called at 24 weeks after the date of admission to assess for bone union and whether complete range of motion at knee joint was present or not. Range of motion was examined only if the fracture had united radiologically.
Statistical Analysis
Random allocation was tested by comparing baseline characteristics of the two groups. Unpaired t-test was used to compare the mean time to negative culture sensitivity, mean time to wound healing, mean time to radiological union of fracture and mean time to achieve full range of motion at knee joint.
Results
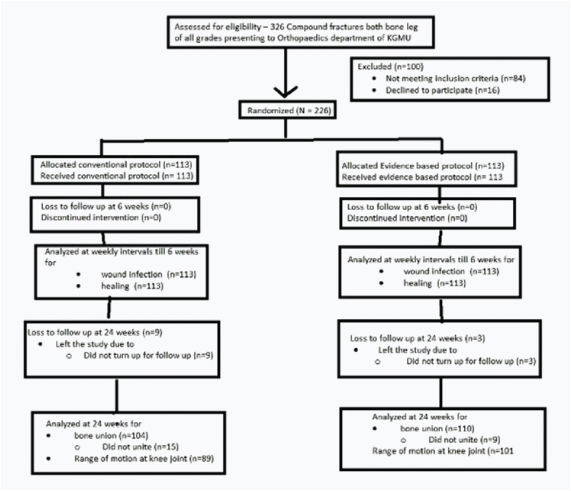
Three hundred twenty six patients of compound fractures of both bone leg presented to department of orthopaedics, KGMU [Table/Fig-1]. These were assessed for eligibility. Eighty four were excluded as they did not match the inclusion criteria of the study. Two hundred forty two patients met the inclusion criteria; of which 16 refused to consent to the study. Thus 226 patients were enrolled in the study. These were randomized to a conventional treatment group and EBP group.
Baseline characteristics of the experimental and control groups were found to be similar for age (p=0.47), grade of fracture (p=0.88), male female ratio (p=0.17), site of fracture (p=0.26), type of fracture (p=0.26), preoperative haemoglobin (p=0.97), duration of surgery (p=0.73), and wound size (p=0.24). This demonstrated the success of randomisation and therefore eliminated the need for controlling confounding during analysis.
Mean time to a negative wound culture was 1.9146 weeks in the EBP group and 4.619 weeks in conventional group. The mean time to healing of wound was 10.45 weeks in EBP group and 14.44 weeks in the conventional group. Time taken to radiological union was 22.81weeks in the EBP group and 23.84 weeks in the conventional group. Mean duration of hospital stay was 4.5 days in the EBP group and 6.5 days in the conventional group. Mean time to achieving complete range of motion was 24.21 weeks in the EBP group and 23.95 weeks in the conventional group.
All patients enrolled in either of the groups were successfully evaluated at weekly intervals for culture sensitivity and healing of wound. The EBP group performed better than the conventional group [Table/Fig-2] as mean time taken to achieve a negative culture (difference in mean: 2.7, p<0.05) and mean time taken for the wound to heal was significantly lower in this group.
Comparing outcome parameters in the conventional group with evidence based group.
| Outcomeparameter | Means in weeks(duration) inConventionalGroup | Means in weeks(duration) inExperimentalGroup | p-value |
|---|
| Time take toa negative culture(duration) | 4.6190(SD ±6.9714) | 1.9146 (SD ±2.4555) | 0.0006 |
| Time take toradiological unionat fracture site(duration) | 23.8427(±1.7379) | 22.8125 (±2.7234) | 0.0027 |
| Time taken forthe wound toheal (duration) | 14.4425(SD ±10.1778) | 10.4513 (SD ±9.9220) | 0.0032 |
| Duration of hospitalstay in days(duration) | 6.5982(SD ±10.9136) | 4.5000 (SD ±5.0171) | 0.0343 |
| Time taken toachieve completerange of movementof joint | 24.2105(SD ±1.2019) | 23.9479(SD ± 1.1274) | 0.1210 |
(Unpaired t-test was used to compare the means)
Nine patients in the conventional group and three patients in the EBP group did not turn up for follow-up at 24 weeks. One hundred four patients in the conventional group turned up for follow-up at 24 weeks. Off these 104 patients, fracture had united in 89 patients. Of the 110 patients in the EBP group that reported at 24 weeks, fracture was found to have united in 93 patients. Fracture did not unite in EBP group in nine patients. Range of motion was recorded in 89 patients in the conventional group and 101 patients in the EBP group [Table/Fig-1].
The EBP group performed better than the conventional group as the mean time taken for complete bone union (difference in mean: 1.03, p=0.0027), and mean duration of hospital stay (difference in mean: 2.09, p=0.034) were significantly lower in the EBP group [Table/Fig-2]. However, there was no statistically significant difference the time taken for achieving complete range of movement (p=0.12) in the two groups. [Table/Fig-3] shows the comparison of reduction in wound sizes at day 1 and week 3 of conventional group and EBP groups.
Comparison of reduction in wound sizes at day 1 and week 3 of conventional group and EBP groups. p- values suggests that there was no statistically significant difference for reduction in size of the wound in the two groups.
| Group | Mean Size ofwound at Day 1 (SD) | Mean Size ofwound at Week 3 | p-value |
|---|
| Conventionalgroup | 14.41 cm (SD ±39.70) | 10.08 cm (SD ±2.89) | 0.07 |
| Experimental(EBP) group | 9.72 cm (SD ±28.28) | 4.51 cm (SD ±18.87 | 0.05 |
Discussion
Till date, many papers individually outlined the benefits of various techniques for controlling perioperative infections in compound fracture. We have reported the impact of adopting EBP based on combining guideline for controlling perioperative infections on important measurable outcomes like time to a negative wound culture and time for the wound to heal. Joel WB studying the effect of occlusive dressing on partial thickness abrasions reported significant benefits of using occlusive dressing over no dressing [17]. Occlusive dressings help in creating an environment that promotes healing as they trap moisture next to the wound bed [18], which may result in enhanced proliferation and migration of fibroblast and keratinocyte [19], as well as the increased inflammatory response and autolytic debridement [20]. Occlusive dressings are reported to stimulate angiogenesis [21] and collagen synthesis [22]. Occlusive dressings protect the wound from contamination and infection and insulate the wound against changes in temperature [23,24]. They are also reported to prevent tissue necrosis and wound desiccation [25]. Decreased pain [23] is also one of the beneficial effects of occlusive dressing. However, the beneficial effects of occlusive dressing may be restricted to wounds that do not show significant exudation [17]. A randomized controlled trial conducted by Ubbink et al., compared the effect of gauze based dressings and occlusive dressings [26]. They reported the median time to wound healing to be lower in the gauze based dressing but the difference was not statistically significant. However, they included a variety of wounds including postoperative surgical wounds, trauma wounds, arterial/venous deficiency wounds, diabetes mellitus wounds and pressure wound. These wounds are known to have a lot of exudate in contrast to wounds seen in Gustilo Anderson grade I and II fractures where there is hardly any exudate.
Osterman PA et al., have reported the benefits of using local antibiotic bone cement beads in conjunction with occlusive dressing in severe compound fractures is reported to significantly decrease infection rates from 12% to 3.7 percent [27].
Many occlusive dressings are far superior to conventional dressings in their barrier capabilities [28]. There is lack of evidence to determine the positive or negative effect of povidone iodine on wound healing. Denning compared dry dressing with povidone iodine dressing on postoperative dressings for nail surgery [29]. They concluded that there was no significant difference in wound healing or infection rates. Saydak et al., compared povidone iodine with an absorbent dressing in pressure ulcers in patients with two wounds and thereby ensured similar co-morbidity [30], nutritional status and age. They reported slower healing rates in ulcers treated with povidone iodine but the difference was not significant statistically probably due to a small sample size.
A significantly faster rate of wound healing as reported by us may be due to the use of occlusive dressing in wounds that hardly showed any exudation; and lower time to a negative culture report as infection is reported to cause wound dehiscence and delayed wound healing [28]. Since we tried to quantify the effect of combining multiple interventions on wound healing, we are unable to comment on the effect of using a single intervention.
Kaiser AB et al., undertook a prospective randomized controlled study (observer-blinded) that compared the ability of preoperative showers with chlorhexidine gluconate, povidone-iodine, and lotion soap to diminish the staphylococcal skin flora in patients scheduled for an elective cardiac operation or coronary artery [31]. The outcomes were compared using cultures obtained from the subclavian and inguinal sites on the evening before the procedure and again the next morning before the operation. They reported that chlorhexidine skin cleanser consistently reduced staphylococcal colony counts at both the subclavian and inguinal sites in contrast to povidone-iodine whose effect was inconsistent.
Numerous studies support the prophylactic application of topical antibiotics to wounds that are clean. A clinical trial conducted by Langford et al., compared the efficacy of a cetrimide, bacitracin zinc and polymyxin B sulfate gel with placebo and povidone iodine cream in preventing infections in 177 minor wounds [32]. They reported the antibiotic gel to be superior to placebo and equivalent to povidone iodine, in that it reduced clinical infections from 12.5% to 1.6%. In an in-vitro study by Anglen et al., reported castile soap to be superior to antibiotic-containing irrigants and normal saline solution when it came to removing bacteria from steel, titanium, muscle and bone [33]. Tarbox et al., compared the effect of benzalkonium chloride with normal saline in an experimental rat model [34]. They reported significant decrease in total number of positive cultures, deep wound cultures and stainless steel cultures with benzalkonium chloride. Conroy BP et al., compared the effect of castile soap, benzalkonium chloride, bacitracin and sequential irrigation (using one litre each of benzalkonium chloride, castile soap and normal saline) for complex contaminated orthopaedic wounds. They reported castile soap and sequential irrigation to significantly lower positive wound pseudomonas cultures when compared with normal saline [35]. Wounds irrigated with benzalkonium chloride alone were reported to have a higher risk of dehiscence and breakdown, a complication which was prevented by using sequential irrigation. However, only benzalkonium chloride was found have to significantly lower positive culture when compared with normal saline.
Lower time to negative culture sensitivity as reported by us may be explained by the combined effects of sequential irrigation, triple antibiotic cream and use of chlorhexidine for preoperative part preparation. However, we are unable to comment on the individual contribution of each of these measures.
Limitation
We have reported a significant advantage of using the EBP with regards to achieving a negative wound culture and early wound healing. However, significant numbers were lost to follow-up (9 in conventional group and 3 in EBP group) when the patients were called up at 24 weeks to assess for fracture union. Another limitation of our study is that only 89 patients in conventional group (15 excluded as fracture did not unite) and 101 patients in the EBP groups (9 excluded as the fracture did not unite) could be examined for range of motion. This loss to follow-up and exclusion from the study limits our ability to comment on effect of the treatment protocol on fracture union and range of motion.
Conclusion
Significantly lesser times to a negative culture, bone healing and wound healing as reported by us in the EBP group compared to conventional group makes a case for adoption of EBP based on guidelines issued in JBJS. However, the decision to adopt or not to adopt EBP by other health care facilities is best left to them as our study was a single centre study and therefore our results may not generalizable to them.
(Unpaired t-test was used to compare the means)