Thyroid disease is the second most common endocrine disorder affecting the women of reproductive age group. Thyroid autoimmunity can alter the progress and the outcome of pregnancy [1–3]. Although the effects of thyroid antibodies in patients with thyroid disorders have been identified, their effect in euthyroid women is still a debatable issue. It was the landmark study by Stagnaro et al., which drew the attention of the researchers to the adverse outcome of anti-thyroid antibodies in euthyroid women [4]. The exact reason for these adverse effects is not known but it has been hypothesised that presence of anti-thyroid antibodies represent a generalized autoimmune imbalance that may be responsible for increased complications despite the euthyroid status. It has also been shown that despite being biochemically euthyroid, women who are positive for thyroid antibodies before pregnancy, may develop subclinical hypothyroidism during pregnancy. It has been reported that the women may have a latent thyroid dysfunction which, due to the increasing demands, may worsen. The other factor is that the presence of antithyroid antibodies potentially leads to infertility and such women get pregnant at a delayed age which per se may be a factor for increased foetal loss [5]. Only a handful of studies are available in the literature that addresses the issue of the effect of anti-thyroid antibodies in the outcome of pregnancy in euthyroid women [6–8]. Furthermore, no substantial Indian data is available on this issue. The objective of our study was to find the prevalence of antithyroid antibodies in the pregnant Indian women. The study also assessed if the euthyroid women who were antithyroid antibody positive had an adverse past obstetrical history or maternal-foetal outcome as compared to those who were negative for antithyroid antibody.
Materials and Methods
A prospective study which was conducted over a period of 12 months from December 2012 to December 2013. One thousand pregnant women, who attended the antenatal outpatient department of our hospital and consented for the study, were screened for the presence of anti-thyroperoxidase (anti-TPO) antibodies in their first half of pregnancy (up to 20 weeks) to assess the prevalence.
Euthyroid women with elevated anti-TPO antibodies were selected from this population which constituted the study group. Women with the history of cervical incompetence or any uterine malformation, those taking drugs which could alter the thyroid levels, those with autoimmune disorders, diabetes mellitus, chronic hypertension, those with known thyroid disorder, those with congenitally malformed foetus and those who are unwilling for follow-up were excluded from the study. The past medical records of the women were screened. The obstetric history (history of infertility, defined as inability to conceive despite one year of unprotected intercourse, recurrent abortions) and the outcome of pregnancy in the anti-TPO positive euthyroid women was evaluated and compared with parity and gestation matched controls (anti-TPO negative). To ensure a comparison within the two groups, the gestational age of the controls (at the time when their blood sample was drawn) was within one week of the matched study subjects. The study group had the assessment of the titres of anti-TPO antibodies and thyroid stimulating hormone (TSH) during the first, second and third trimester and also in the post partum period to assess their trends during the course of pregnancy. The thyroid parameters were measured using electro chemiluminiscence ELISA method.
Following parameters were noted in the study and control group: age, Body Mass Index (BMI), gestational hypertension and pre-eclampsia, anaemia (tested in the first trimester), intrauterine growth restriction, placental abruption, preterm delivery, postpartum haemorrhage, neonatal jaundice and exchange transfusion. The data was statistically analysed with SPSS (version 17.0). For variables, frequency distribution, relative frequencies, their percentages, mean standard deviations were computed. Student’s t-test was used for the comparison of mean between two segments of data.
Ethical approval was obtained from the institutional Ethical committee (“Institutional Ethical Committee, PGIMER, Chandigarh. NK/30/MD/8677, 27/2/2012).
Results
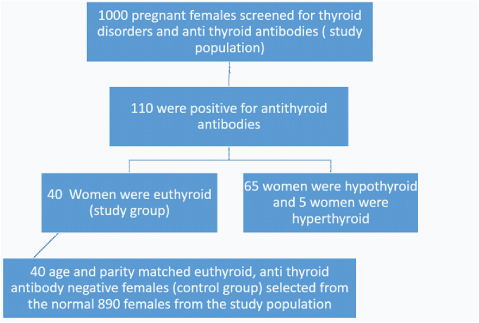
Of the total of 1000 pregnant women who were screened for the presence of anti-TPO antibodies, 110 were found to be anti-TPO positive, hence, the prevalence of anti-TPO positivity was 11%. Sixty-five women in this group who were found to be anti-TPO positive were hypothyroid with the TSH value lying above the normal range (0.2-4.2mIU/ml), while 5 women were hyperthyroid.
Forty women were found to be anti-TPO positive with the TSH being in the euthyroid range (prevalence of 4%). These women constituted the study group and were followed up as per the study protocol. Equal numbers of women in the control group were selected after matching them with the study group on the basis of parity and period of gestation [Table/Fig-1].
The selection of the total population and the study and the control group.
The age ranged from 21-35 (mean 26.95±3.809) years in the study group while that in the controls, it was from 21-32 (mean 26.38 ± 2.826) years. The BMI in the anti-TPO positive subjects was 22.472 (SD ±2.81) while in the controls it was 21.93 (SD ±2.02). The anti-TPO positive group was significantly overweight as compared to the anti-TPO negative group (p=0.0001). On the analysis of subsets of BMI i.e., underweight (BMI<18.5), normal weight (BMI 18.5-25) and over weight (BMI>25), there was no statistical difference between the underweight patients of both the groups (p=0.5483) while the anti-TPO positive patients had significantly higher number of overweight patients with BMI>25 (p=0.0001).
Mean TSH level in the first trimester in anti-TPO positive subjects was 2.67±1.15 mIU/L. As one pregnancy ended up in abortion, only 39 patients got the second trimester TSH done, the mean of which was 2.33±1.16 mIU/L. All these women had their TSH assessed again in the third trimester; the mean value at that time was 2.12±0.92 mIU/L. The postpartum mean TSH value was 7.6±18.23 mIU/L [Table/Fig-2].
Thyroid stimulating hormone (TSH) and anti-thyroperoxidase (anti-TPO) titres in the study group.
| TSH (mIU/ml)(Mean±SD) | Anti-TPO (IU/ml)(Mean±SD) |
|---|
| First trimester | 2.67±1.15 | 209±284.32 |
| Second trimester | 2.33±1.16 | 112.34±126.08 |
| Third trimester | 2.12±0.92 | 76.06±83.44 |
| Post partum | 7.6±18.23 | 84.13±106.32 |
Anti-TPO titres (indicator of the antibody concentration) were estimated in all the women of the study group in the first trimester using the ELISA. Four didn’t have their anti-TPO titres analysed in their second and third trimesters. The mean anti-TPO titre in the first trimester was 209±284.32 IU/ml. The mean anti-TPO titres of the 36 patients in their second and third trimesters were 112.34±126.08 IU/ml and 76.06±83.44 IU/ml respectively. The mean anti-TPO level in postpartum period was 84.13±106.32 IU/ml [Table/Fig-2]. The anti-TPO titres showed a significant decrease in 2nd and 3rd trimester when compared to the titres in the 1st trimester with a p-values of 0.016 and 0.003, respectively (paired t-test).
The women were followed for six weeks after delivery. None of the patients developed symptomatic hypothyroidism in both the groups. Sixteen of the euthyroid, TPO-positive patients developed biochemical hypothyroidism (TSH>5.2) in the postpartum period, prevalence being 40%. These women were referred to the endocrinology department for further management.
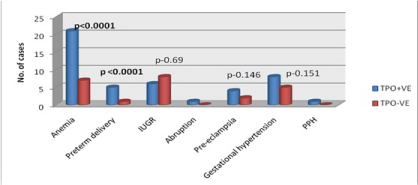
There was no statistical difference between the rates of recurrent abortions (defined as 2 or more consecutive abortions) between the two groups (8 vs. 5 respectively, p-value-0.367). The prevalence of infertility and anaemia was also higher amongst the anti-TPO positive cases. Preterm deliveries in the study group were 12.5% (5 out of 40) while it was only 2.5% in the control group (1 out of 40), which was statistically significant.
Other complications like intrauterine growth restriction, hypertensive disorders of pregnancy, abruptionor postpartum haemorrhage [Table/Fig-3] did not vary in between the groups.
The maternal and foetal complications in the study and the control groups.
 |
| Variable | No. of casesin Anti TPO+ | No. of casesin Anti TPO-ve |
| Anemia | 21 (52.5%) | 7 (17.5%) |
| Preterm delivery | 5 (12.5%) | 1 (2.5%) |
| IUGR | 6 (15%) | 8 (20%) |
| Abruption | 1 (2.5%) | 0 |
| Pre-edampsia | 4 (10%) | 2 (5%) |
| Gestational hypertension | 8 (20%) | 5 (12.5%) |
| PPH | 1 (2.5%) | 0 |
There was no significant difference in the incidence of neonatal jaundice in the two groups. None of the babies in either group required exchange transfusion.
Discussion
Thyroid disorders are common during pregnancy and can affect its outcome. Our study revealed the overall prevalence of anti-TPO positivity to be 11% in the sample population. In a similar study by Negro et al., the overall prevalence was found to be 11.7% while it was 12.5% in a study by Olivieri et al., [5,9]. A few researchers have tried to evaluate the effect of thyroid disorders in pregnant women and during the course of evaluation, have also assessed the rate of anti-thyroid antibody positivity rate in their sample population. The rates of anti-thyroid antibody positivity are varied in these studies and depend upon the sample size as well as the geographical factors of the study group. The prevalence of anti-TPO antibodies of the major Indian studies have been tabulated in [Table/Fig-4] [10–13].
The data from Indian literature that assess the prevalence of anti-thyroid antibodies in euthyroid pregnant women.
| Authors | Year ofpublication | Populationstudied (area) | Prevalence ofanti-thyroid antibodiesin euthyroid pregnant women |
|---|
| Gayathriet al., [10] | 2009 | Tamil Nadu | 7% |
| Nambiaret al., [11] | 2011 | Maharashtra | 5.8% |
| Bhattacharyyaet al., [12] | 2015 | West Bengal | 11.34% |
| Mandalet al., [13] | 2016 | West Bengal | 1.47% |
| Presentstudy | 2016 | Chandigarh | 4% |
There was an association between the Body Mass Index (BMI) and anti-TPO positivity in our study. Majority of the studies have shown a positive correlation between the TSH values and BMI [14,15]. However, there was no such correlation in our study.
The literature suggests that anti-TPO antibodies adversely affect the outcomes of the pregnancy in euthyroid women. The exact mechanism for this is still debateable. The possible reasons that have been suggested are that such women have subclinical deficiency of the thyroid hormone and they are not able to meet the increased requirements of pregnancy. It has also been proposed that the presence of anti-TPO antibodies suggests a generalised autoimmune milieu in the body which adversely affects the foetus and result into spontaneous abortions, preterm delivery, IUGR etc. Regarding the history of recurrent abortions in thyroid autoimmune group, our study did not show any statistically significant association. However, the literature suggests a higher rate of miscarriages in the thyroid autoimmunity positive group [1–3,16,17]. There was a higher prevalence of infertility in anti-TPO positive group (35%) than the controls (2.5%), which was statistically significant. This is in agreement with the other studies [18,19].
A direct co-relation has been found between anti-TPO positivity and the rate of preterm delivery. Glinoer et al., in a study of 120 euthyroid women showed that the rate preterm deliveries in women with thyroid autoimmunity almost doubled as compared to the healthy controls [16]. Negro et al., too reported that anti-TPO positive women were more likely to have premature delivery when compared to normal women (22.4% Vs 8.2%, p-0.003). They also compared the effect of administration of levothyroxine in patients who were anti-TPO positive and found that the rates of premature delivery decreased and were at par with the normal population (7% vs 8.25%) [5]. Our study also showed a significantly higher prevalence of the rate of preterm delivery in the anti-TPO positive subjects.
Very few studies have addressed the co-relation of anaemia and thyroid disorders [6,8]. In our study, a significantly higher prevalence of anaemia in subjects with thyroid autoimmunity was observed. As any other autoimmune disorders, the auto-antibodies may be responsible for the destruction of red blood cells along with the inflammatory process setting in.
There was no difference seen in the IUGR rates in the two groups in our study with the prevalence being 15% in the study group and 20% in the controls. Studies have shown increased rates of low birth weight babies in thyroid autoimmune patient [8,20]. A few attributed the hypertensive disorders of pregnancy to be accountable for the same, indirectly linking the TAI and IUGR. In our study too, one patient had mild IUGR in the setting of severe pre-eclampsia along with thyroid autoimmunity.
Moncef Feki et al., reported that women with positive anti-TPO have a trend toward higher prevalence of gestational hypertension, recurrent pregnancy loss, especially late abortions and foetal death [21]. Our study did not show any statistically significant association between thyroid autoimmunity and pregnancy induced hypertension or recurrent miscarriages.
Limitation
“Our study is not without limitations. Ours is a referral hospital and patients from all over the country come here for treatment. Despite this, we acknowledge that majority of the patients belong to Chandigarh, Haryana and Punjab hence the prevalence of anti-TPO positivity in our study may not be reflective of the entire national population. The samples derived from the hospital population are also subject to Berksonian bias which can also lead to the disparity in the prevalence rates. It is however noteworthy that the matching of study and control group in our study decreases the risk of bias and also addresses the possible confounders to a large extent.
Conclusion
To conclude, thyroid autoimmunity has its effect on obstetric outcomes, like preterm delivery and postpartum thyroiditis even in patients who are euthyroid. Our results indicate that screening of thyroid autoimmunity in pregnant patients may be clinically beneficial as it offers an opportunity for early detection of the population at risk and can help in better management. Our study also encourages further research in evaluating the effect of thyroid autoimmunity in pregnancy in larger, multi institutional settings which could result in formation of a consensus.