Post Partum Haemorrhage (PPH) is a leading cause of maternal death worldwide, it is responsible for 30% of all direct maternal deaths that occurred in 1-5% of pregnancies in developed and developing countries [1,2]. PPH is defined as: blood loss ≥500cc and ≥1000cc after vaginal delivery and cesarean section, respectively [2]. Although 50% of all patients placed in this definition and their blood loss was ≥500cc, but we can estimate only half of blood loss [3]. Severe PPH is determined by decreasing of haematocrit (10%) and need for blood transfusion in post delivery period, i.e. severe bleeding occurred in 4% vaginal labour and 6% of cesarean section [4]. It is estimated that in worldwide 500,000 maternal deaths occurred, of these approximately one forth is caused by PPH [5]. The four main causes of PPH are uterine atony, labour canal laceration, coaglupathy and abnormal adhesion of placenta [2]. The most common cause of PPH is uterine atony, so prevention and treatment atony is the best intervention [6]. Now-a-days, some method performed for PPH including drugs that enforce uterine contractions such as Oxcytocin, Carboproset. Many complication for PPH patients occurs if oxcytocin is administered as intravenous which include (hypotension) tachycardia, low perfusion of coronary arteries, cardiac arrest and high doses, but slow infusion of oxcytocin also have complications such as convulsion due to hyponatraemia and antiduieretics effect [7,8], so there is need for safer administration of oxcytocin. Literature showed that hypoxia is one of the leading cause of uterine atony [7] and increasing of supply O2 to myometer through O2 inhalation could be effective contractions and resulted in prevention of bleeding [9] Ramsey et al., reported a cause of CO poisoning that O2 therapy was resulted in resolution of bleeding and improved mental status [10] also women who experienced dyspnea after cesarean section and uterine atony following it approved this notion that O2 therapy can improve contraction and prevented bleeding [9]. In this case many clinical trials have been performed that showed paradox results [10–12].
Yatawatta et al., in Srilanka, studied the effect of oxygen inhalation immediately after normal delivery on blood loss and concluded that the oxygen inhalation at 3rd stage stage of labor appear to reduce blood loss.
Considering safe delivery and importance of PPH in controlling mother and her child’s life and paradox studies, the present study was conducted to evaluate the effect of O2 inhalation plus oxytocin compared with oxytocin only on PPH.
Materials and Methods
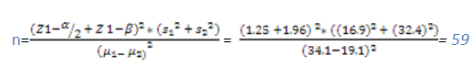
This study was a clinical trial for which the researchers, after receiving a written verification from Ilam (western Iran), Medical University Ethics Committee, as well as a written permission signed by Head of Research Deputy and Head of Treatment Deputy of Ilam University of Medical Sciences, referred to Shahid Mostafa Khomeini (PBUH) Hospital of Ilam and besides observing Helsinki & Belmont statements, studied 120 women who had eligible criteria and were referred between April 2012 to Nov 2013. It should be noted that we calculated the sample size based on the following formula:
Considering the sample size the inclusion and exclusion criteria 120 eligible women were included. There was no dropout after randomization and the data of 120 women were available for analysis. Written consent form was signed by all the sutdy subjects. The inclusion criteria were: 18-35years age group, single-delivery, alive fetus, fetus weight 2500-4000 gram and vaginal delivery. We excluded women who had blood pressure >140/90, placenta previa, placenta abortion, history of bleeding during pregnancy, curettage, cesarean section or uterine scar, PPH, polyhydraminos, uterine anomaly, immunity impairment, instrumental delivery, HB<8g/dl, anticoagulant drugs consumption, prolongation of first stage of labour greater than 15 hours, rapid delivery (less than 3 hours), as well as multiparity.
The cases were randomly divided into two groups of 60 women and both of them received 1000CC Ringer lactate serum and 20 IU Oxytocin for management of third stage of labour. Participants who assigned in intervention group received 8 liters O2 through face mask from fetus delivery to 2 hours later, control group inhaled room air. Then O2 saturation was measured by pulse oxymeter device, blood loss determined by weighting of gauzes.
In both of groups blood pressure, temperature, pulse & respiratory rate were measured and recorded each quarter and each half- hour during 1 and 2 hours after delivery, respectively [Table/Fig-1]. Also, frequency of lactation and its duration by determining sucking by neonate were recorded. PPH were calculated by weighting of used gauzes and Shaun by digital SECA model paediatric balance. Randomization was performed by first pick up of the participant name then the participants were selected as sequential. The data were collected by interview, observations as well as digital balance (sensitivity= 1 gr). The clinical trial registration code is IRCT2012102411253N1.
Comparison Mean ± SD of V/S in two groups during first and second hours after delivery.
| Vital Signs | Intervention Group | Control Group | p-value |
|---|
| Before Intervention | First hour | Second hour | Before Intervention | First hour | Second hour | Before Intervention | First hour | Second hour |
|---|
| BP (Systolic) | 118.3±7.4 | 111.3±9.2 | 110.2±6.7 | 115.7±7.3 | 112.1±8.0 | 113.4.±8.8 | 0.65 | 0.62 | 0.45 |
| BP (Diastolic) | 74.2±1.4 | 71.39±8.1 | 67.3±7.3 | 75±2.3 | 70.7±9.9 | 69.6±9.4 | 0.52 | 0.93 | 0.56 |
| PR | 81.1±2.1 | 82.4±3.4 | 71.1±1.4 | 80.5±2.2 | 83.5±4.2 | 79±5.9 | 0.27 | 0.15 | 0.00 |
| RR | 19.1±0.58 | 18.4±0.45 | 17±0.46 | 19±0.67 | 19±0.2 | 18.5±0.37 | 0.13 | 0.59 | 0.00 |
| T | 37±0.11 | 37.1±1.8 | 37±2.1 | 36.9±0.15 | 37.2±2.1 | 37±2.3 | 0.55 | 0.57 | 0.55 |
Statistical Analysis
Validity and reliability were measured through content and pearson correlation coefficient (r=0.92) besides the balance were checked daily by 500 grams calibration weights. The observed data were analysed using SPSS, version 16 Software using Student-t and Chi-square tests.
Results
The study and the control groups were similar in age, parity, gestational age, first and second stages of labour, lactation period and frequency, fetus gender and weight, education and job status of mother, wanted or unwanted pregnancy, induction rates, episiotomy rate as well as spontaneous lacerations [Table/Fig-2].
Comparison baseline variables in two groups.
| Variable | Intervention Group | Control Group | p-value |
|---|
| Age (year) | Mean+SD | 27.68±5.4 | 29.5±4.8 | 0.57 |
| Weight (gr) | Mean+SD | 3200±258 | 3300±285 | 0.06 |
| Gravidity rate | Mean+SD | 1.78±0.8 | 1.80±0.8 | 0.91 |
| Lactation frequency | Mean+SD | 1.88±0.7 | 1.78±0.8 | 0.46 |
| Lactation duration | Mean+SD | 25.7±10 | 24.2±10 | 0.43 |
| Educational level | Preliminary | 13(21.7%) | 10(16.7%) | 0. 67 |
| Guidance school | 11(18.3%) | 16(26.7%) |
| High school | 27(45%) | 25(41.7%) |
| Higher education | 9(15%) | 9(15%) |
| Location ofresidence | City | 44(47.3%) | 49(52.7%) | 0.27 |
| Village | 16(26.7%) | 11(18.3%) |
| Job status | Employee | 12(20%) | 11(18.3%) | 0.81 |
| House keeper | 48(80%) | 49(81.3%) |
| Race | Kurd | 47(78.3%) | 50(83.3%) | 0.44 |
| Non-Kurd | 13(21.7%) | 10(16.7%) |
| Neonate sex | Boy | 35(58.3%) | 29(48.3%) | 0.27 |
| Girl | 25(41.7%) | 31(51.7%) |
| Pregnancy status | Wanted | 52(86.4%) | 49(81.7%) | 0.35 |
| Unwanted | 8(13.6%) | 11(18.3%) |
The study results indicated that the mean of blood loss were (256.16±97) ml at the two hours after delivery in the control group and (149.5±46.49) ml in the intervention group with p=0.006, the difference was statistically significant [Table/Fig-3].
Comparison Mean+SD of PPH in two groups during 2 hours after delivery.
| Intervention Group | Control Group | p-value |
|---|
| First hour | 101.55±37.15 | 171.76±77.43 | 0.002 |
| Second hour | 47.53±17.6 | 80.41±35.7 | 0.001 |
| Total | 149.5±46.49 | 256.16±97.25 | 0.006 |
Discussion
The amount of bleeding which occurred in first hour after delivery and uterine atony is the most common cause [12]. In many studies hypoxia was an important factor in aetiology of uterine atony [7]. Till now three studies have performed about effect of O2 therapy on PPH [10–12]. The finding of present study is similar with other studies.
Yatawatta et al., evaluated the effect of oxygen inhalation on blood loss among 60 women with normal vaginal delivery [9]. The results of study demonstrated that mean vaginal blood loss during the 1st hour was lower in oxygen group as compared with control group (16.9±19.1mL vs 32.4±34.1mL). This difference was statistically significant (p=0.05). In another study the mean vaginal blood loss 2 hours postpartum was 27.7 ± 5.8 ml in O2 inhalation group and 48.8± 8.4 ml in the controls (p < 0.05) [13].
Above mentioned studies [9,13] showed that PPH in O2 therapy patients is lower than control group and blood loss reduction in these studies is the role of oxygen on improvement of uterine contractions. In present study, we achieved similar findings.
However, in contrast with our finding Güngördük et al., conducted a clinical trial in Istanbul, which aimed to evaluate the role of O2 therapy on PPH. Based on their results, the blood loss during third and fourth stages of labour had no significant differences between the control and oxygen-inhalation groups (294.5 ± 179.7 vs 273.4 ± 146.6 mL, respectively) [11]. It is concluded that these differences between above mentioned study and other study may be due to confounding variables such as bleeding due to canal lacerations, genetics, difference in time of O2 consumption, O2 concentration and various sample sizes.
In case of O2 mechanism on PPH reduction, it has been hypothesized that increasing of supply to myometer through O2 inhalation by mother could be caused to uterine muscles contraction and decreasing blood loss [10].
Also, based on oxy-haemoglobin dissociation curve, when we inhalate air of room PaO2 is 100 mmHg and when we inhalate O2 (40%) by mask, it is anticipated that the PaO2>200 mmHg, this resulted in 2 fold increasing of PaO2 in O2 inhaled group, increasing PaO2 maybe by increasing contraction of myometer muscles caused to reduction in bleeding, besides, it cause to increasing of muscle tone in vascular system and finally decreasing of bleeding [9].
Seidy et al., performed study with the aim to assess the effectiveness of supplementary O2 therapy on severity of nausea and vomiting after cesarean section, they concluded that increasing of O2 caused to serum dopamine reduction, that dopamine through excitation of post synaptic of Dopamin-1 in smooth muscles vessel caused to vasodilatation [14], also this is a probable causes of effectiveness of O2 on blood loss reduction.
In this study, the oxygen that is a safe, nontoxic, inexpensive and available drug, in short term has no side effects, and was seen as an utero-tonic agent.
Limitation
The limitations of this study were relatively small sample size and was not blinded. We suggest studies with large sample sizes, also in addition to study the effect of O2 on prevention of atony after cesarean delivery.
Conclusion
Based on the research finding, we concluded that use of O2 through inhalation immediately after fetus delivery and during third and forth stages of labour with oxytocin infusion helps in reduction of bleeding after delivery. It is effective, safe and inexpensive method that also decreases other utero -tonic drugs consumption for controlling PPH.