Congenital Midline Tongue Base Mass in An Infant: Lingual Hamartoma
Noraziana Fadzilah1, Mawaddah Azman2, Goh Bee See3
1 Medical Officer, Department of Otorhinolaryngology and Head and Neck Surgery, Level 9, Clinical Block, Hospital Canselor Tuanku Mukhriz, Universiti Kebangsaan Malaysia Medical Center, Jalan Yaacob Latiff, Cheras, Kuala Lumpur, Malaysia.
2 Specialist, Department of Otorhinolaryngology and Head and Neck Surgery, Level 9, Clinical Block, Hospital Canselor Tuanku Mukhriz, Universiti Kebangsaan Malaysia Medical Center, Jalan Yaacob Latiff, Cheras, Kuala Lumpur, Malaysia.
3 Consultant, Department of Otorhinolaryngology and Head and Neck Surgery, Level 9, Clinical Block, Hospital Canselor Tuanku Mukhriz, Universiti Kebangsaan Malaysia Medical Center, Jalan Yaacob Latiff, Cheras, Kuala Lumpur, Malaysia.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Noraziana Fadzilah, Medical Officer, Department of Otorhinolaryngology and Head and Neck Surgery, Level 9, Clinical Block, Hospital Canselor Tuanku Mukhriz, Universiti Kebangsaan Malaysia Medical Center, Jalan Yaacob Latiff, 56000 Cheras, Kuala Lumpur, Malaysia. E-mail : ozayana@gmail.com
Lingual hamartoma is a rare finding of congenital midline posterior tongue mass. The lesion may be seen as a single anomaly or maybe associated with syndrome especially the Oral Facial Digital Syndrome (OFDS). Here, we report an otherwise normal and healthy two-month-old boy with a congenital midline base of tongue mass presented with snoring and episodic vomiting since the age of 1 month. Tumour excision from the area of foramen of caecum recovered a pinkish pedunculated tumour. Histopathology examination confirmed the diagnosis of leiomyomatous lingual hamartoma. Differential diagnosis, especially for midline tongue mass and other paediatric tongue lesions are discussed. We also discuss the epidemiology, histopathologic features, treatment and prognosis of lingual hamartoma based on the literature review.
Excision, Oral facial digital syndrome, Pediatric
Case Report
A one and half-month-old boy was referred from outpatient of a private clinic to our medical centre with complaint of snoring and episodic vomiting since 1 month. The mother also observed an intraoral mass since birth. The mother noticed it since day 3 post natal period, but never sought treatment for the problem. The swelling did not increase in size and never caused a problem until the age of 1 month. The mother noted the child to snore especially when he slept in supine position and the sounds were louder when the child had cough and runny nose. Otherwise, the child was tolerating breast feeding and there was no choking, nor cyanotic spells and he was thriving well. There was no history of perinatal insults. The child was born full-term with birth weight of 3.7kg. His birth was uneventful and his immunization was up to age.
When examined in our clinic, the child was comfortable, neither in stridor nor respiratory distress. A flexible scope showed a pinkish, pedunculated mass, originating from the tongue base. No abnormalities were observed over the larynx and the vocal cords were mobile. The results of thyroid function test were within normal limits and ultrasound of neck showed a normal thyroid gland in its usual position in the neck. There were no pre-operative imaging done prior to the surgery.
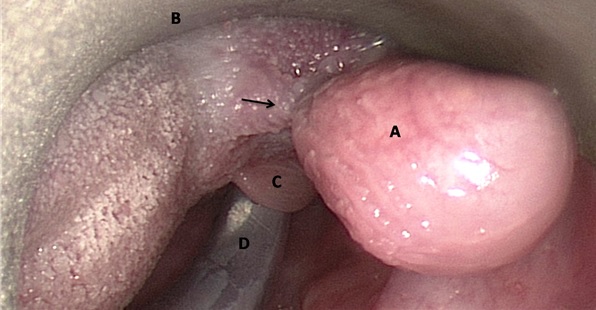
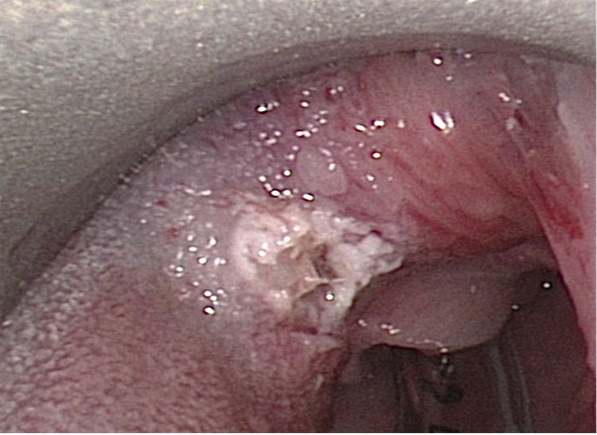
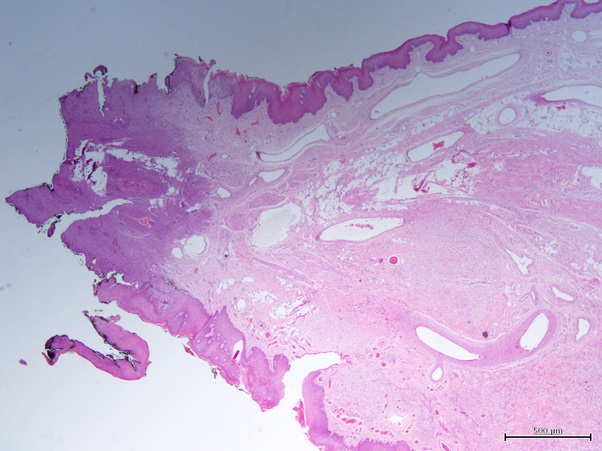
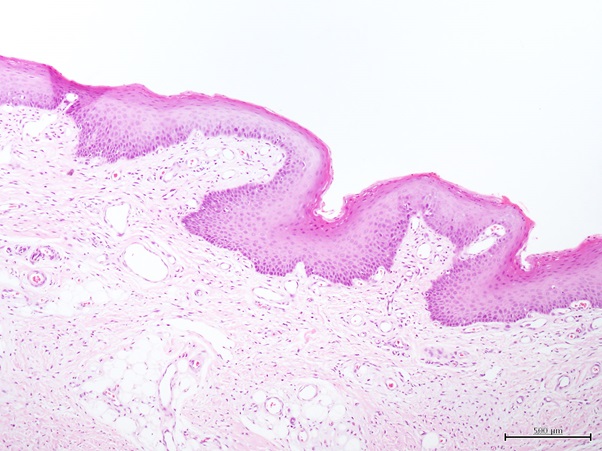
After discussion with the parents, they agreed and consented for the surgery. At 2 months, he underwent transoral tumour excision. Airway was secured with an endotracheal tube by a senior anaesthetist. Examination under anaesthesia using Lindholm laryngoscope (Karl Storz, Germany) showed a pedunculated, firm mass, measuring 1.5x0.6x0.5 cm, arising from midline base of tongue [Table/Fig-1]. The mass was excised using cold instrumentation and surrounding mucosa with a thin layer of tongue musculature was removed without complications [Table/Fig-2]. Histopathology examination confirmed the diagnosis of smooth muscle predominant lingual hamartoma [Table/Fig-3,4]. The patient tolerated the procedure well and was discharged the following day after uneventful airway observation. There was no recurrence of the lesion to date.
A: pedunculated tongue base mass, B :Lindhom laryngoscope C :Lingual surface of epiglotis, D: Endotracheal tube,
Post excision of tongue base lesion.
A section showing a polypoidal lesion with thin stalk lined by stratified squamous epithelium.
A section showing mature stratified squamous epithelium with underlying stroma composes of predominantly unencapsulated smooth muscle fibers intermingle with occasional adipose tissues and vascular channels.
Discussion
Hamartoma is a benign tumour-like overgrowth of mature tissue which is native to the organ of its origin [1]. Lingual hamartoma is a rare tongue mass, primarily diagnosed in childhood and was first described in 1945 by Stamm and Tauber [2]. It is a congenital lesion, which is usually asymptomatic and detected as incidental tongue mass [1]. From literature review by Nava-Villalba et al., they described specific clinical characteristics of hamartoma in the oral cavity which include: 1) small lesion (less than 1.5 cm in largest diameter); 2) pink pedunculated/polypoid lesion; 3) tendency of occurrence in the midline of the palate(anterior region) or the midline of the tongue [3].
Lingual hamartoma may present as an isolated anomaly or as part of syndrome especially Oral Facial Digital Syndrome (OFDS) which is a group of hereditary disorders comprising of oral abnormality, facial dysmorphism and hand/foot malformations [4]. It was described that lingual hamartomas presenting as an isolated anomaly are extremely rare [5]. However, a previous review of 135 cases involving paediatric tongue lesions, reported 14 out of 18 lingual hamartomas to occur in otherwise normal non-syndromic children [1].
Differential diagnosis of midline posterior part of tongue lesion in children often is thought to be of a lingual thyroid gland or a thyroglossal duct cyst, as this lesion most commonly occurs in the area of foramen caecum. The presence of a normal-appearing thyroid in the lower neck also may not exclude lingual thyroid.
Nevertheless, lingual hamartomas may also occur as solitary lesions on the dorsum of the tongue, usually posterior and midline in the area of the foramen cecum [5] and should be considered as one of the differential diagnosis in the present case, although the occurrence is rare. The position of these lesions to occur in the midline posterior part of the tongue may be explained on its location as a fusion region during embryological development [5].
Some other lesions that may be present as congenital midline tongue mass includes choristoma, leiomyoma and benign mesenchymoma. Other causes of paediatric tongue lesions irrespective of the site of occurrence would be vascular or lymphatic lesion (lymphangioma, pyogenic granuloma, capillary haemangioma, vascular malformations), mucus extravasation phenomenon, reactive or traumatic lesions (fibroma and neuroma), cystic lesion, benign and malignant neoplasm [1].
Most of the lingual hamartomas demographically occur in young aged children, less than 2 years [1,3] with female preponderance [1,5]. According to definition, all lesions are present at birth but age of presentation for excision ranges between 1 month to 61 years [1,3]. Summary of the literatures is presented in [Table/Fig-5].
Summary of literature review.
| Authors | Number of case(s) | Gender | Symptoms/presentations | Associated syndrome | Appearance | Site | Age at surgical excision |
|---|
| Kreiger et al., 2007 [1] | 18 | 6 males,12 females | All asymptomatic mass, except one with choking and cyanotic spells | 4 cases associated with OFDS | Range in size of 0.1-2 cm; and nodular, polypoid or pedunculated gross appearance | All at dorsal part of tongue except 1 case at the ventral part of the tongue | Less than 2 years old: 15 cases.3 cases at age 3, 5, 16 years old respective |
| Stamm and Tauber, 1945 [2] | 1 | Female | Feeding difficulties | None | Sessile tumour | Base of tongue, more to the left | Day 9 of life |
| Nava-Villalba et al., 2008 [3] | 1 | Male | Congenital asymptomatic tongue mass | None | 7 mm, polypoidal pedunculated lesion | Posterior third, dorsum of tongue | 5 months old |
| Hsu et al., 2012 [4] | 1 | Female | Incidental finding of granular lesion at the tongue | None | Pedunculated 1.5x0.6x0.5 cm | Base of tongue, more to the left | 1 year 5 months old |
| Goold et al., 2003 [5] | 1 | Male | Congenital asymptomatic tongue mass | None | Lobulated sessile mass 2x 2cm | Base of tongue, near foramen caecum | 5 months old |
| Valdyanathan et al., 2011 [6] | 1 | Female | Congenital asymptomatic tongue mass | None | 1.5 cm sessile lesion | Left lateral border of tongue | 1year 2 months old |
| de Faria et al., 2008 [7] | 1 | Female | Congenital asymptomatic tongue mass, rapid enlargement at 61 years old with dysphagia, dysphonea, dyspnoea for 2 weeks duration | None | “Giant leimyomatous hamartoma” 4 cm bilobulated, pedunculated lesion | Midline, posterior region of the tongue | 61 years old |
| Kuperan et al., 2012 [8] | 1 | Male | Congenital asymptomatic tongue mass | None | 0.5 cm pedunculated mass | Midline posterior part of the tongue | 5 months old |
| Wang et al., 2013 [9] | 1 | Male | Painless slow growing mass on the tongue since childhood | Having bifid tongue with tongue tie, but not associated with OFDS | 2x1.5cm, pedunculated mass | Anterior midline of the tongue, near the apex of the bifid tip | 29 years old |
| Noraziana et al., 2016 | 1 | Male | Congenital tongue mass with snoring and episodic vomiting | None | 1.5 x 0.6 x 0.5 cm, pedunculated mass | midline base of tongue | 2 months old |
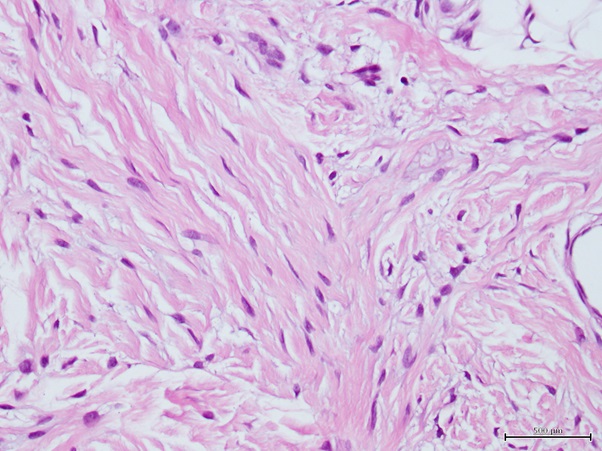
Typically, lingual hamartoma occur in the submucosal connective tissue, superficial to the tongue muscles [1]. The type of hamartoma is classified largely on the predominant cell type in the histological specimen namely, leiomyomatous, rhabdomyomatous, neurovascular, fatty, glial and so forth [5]. In routine histologic Haematoxylin and Eosine (H&E) examination, features of leiomyomatous hamartoma compose of smooth muscles bundles which are unencapsulated in the submucosal region and haphazardly arranged intermingled with variably sized vessels, adipose tissues, nerves tissues or salivary glands. On higher magnification, the presence of spindle shape cells, with elongated and tapered end nuclei can readily be seen [Table/Fig-6]. Immunohistochemistry (IHC) staining may help to confirm leiomyomatous hamartoma by identification of smooth muscle actin, muscle-specific actin, S-100 protein and desmin [3]. The fact that it differs from neoplasm is from the absent of pleomorphism of the nuclei in the tumour [3].
Fusiform eosinophilic cells with elongated tapered end nuclei.
In our case ultrasonography of neck was performed to confirm presence or absence of cervical thyroid tissue as to rule out lingual thyroid or ectopic thyroid tissue. Preoperative CT scan or MRI was not performed prior to operation as the lesion has benign characteristics on the clinical appearance i.e. small lesion with pedunculated stalk. The radiological feature is not well described in literature, as majority of the cases were operated without preoperative imaging. However, from limited reports with pre-operative imaging of CT scan and MRI have shown inconsistent findings with no specific characteristic [4].
Definitive step of management is excision of the tumour. According to literature review, the prognosis is good and there are no cases of recurrence following complete surgical excision of lesion [3–9].
Conclusion
In general although it is rare, lingual hamartoma should be considered as a differential diagnosis of a congenital midline base of tongue lesion in children apart from lingual thyroid and thyroglossal duct cyst. Having a history of OFDS may suggest the possibility of having this lesion. However, we should also consider lingual hamartoma as one of the differential diagnosis, taking into account majority of cases occur in a normal and non syndromic child. Standard histologic H&E confirmed the diagnosis of leiomyomatous hamartoma, and IHC staining may aids in the diagnosis when in doubt. The treatment of choice is complete surgical excision of the lesion. It has a good prognosis, as no recurrence of the lesion after excision is reported in literature, to date.
[1]. Kreiger P, Ernst L, Elden L, Kazahaya K, Alawi F, Russo P, Hamartomatous tongue lesions in childrenThe American Journal of Surgical Pathology 2007 31(8):1186-90. [Google Scholar]
[2]. Stamm C, Tauber R, Hamartoma of tongueThe Laryngoscope 1945 55(3):140-46. [Google Scholar]
[3]. Nava-Villalba M, Ocampo-Acosta F, Seamanduras-Pacheco A, Aldape-Barrios B, Leiomyomatous hamartoma: report of two cases and review of the literatureOral Surgery, Oral Medicine, Oral Pathology, Oral Radiology and Endodontology 2008 105(4):e39-e45. [Google Scholar]
[4]. Hsu Y, Hsu W, Tongue base hamartoma in a childJournal of the Formosan Medical Association 2012 111(7):406-07. [Google Scholar]
[5]. Goold A, Koch B, Willging J, Lingual Hamartoma in an Infant: CT and MR ImagingAmerican Journal of Neuroradiology 2007 28(1):30-31. [Google Scholar]
[6]. Vaidyanathan M, Williams C, Morgan P, Rhabdomyomatous mesenchymal hamartoma of the tongueCase Reports 2011 2011(jun19 1):bcr0820103225-bcr0820103225. [Google Scholar]
[7]. de Faria P, Batista J, Duriguetto A, do Nascimento Souza K, Candelori I, Cardoso S, Giant leiomyomatous hamartoma of the tongueJournal of Oral and Maxillofacial Surgery 2008 66(7):1476-80. [Google Scholar]
[8]. Kuperan A, Mirani N, Qurashi H, Case Report of a Congenital Leiomyomatous Hamartoma: New Epidemiological Findings and a Review of the LiteratureThe Laryngoscope 2011 121(S4):S209-S209. [Google Scholar]
[9]. Wang H, Chiang F, Tai C, Tsai K, Wang L, Lingual leiomyomatous hamartoma with bifid tip and ankyloglossia in a patient without oral-facial-digital syndrome: a case report and literature reviewWorld J Surg Onc 2013 11(1):230 [Google Scholar]