The Cerebrospinal Fluid (CSF) is a layer of fluid surrounding the brain and it provides the brain with a cushion against the bony cranial walls. CSF is produced in the brain and absorbed by the arachnoid villae. Leaks in the duramater with associated bony defects are known to occur due to a variety of reasons from trauma to malignancy to being of congenital origin. CSF leaks are potentially life threatening as the fistulae are conduits for ascending infections to the brain. These leaks are commonly seen from the nose where they present as a clear watery rhinorrhoea and are usually unilateral. CSF leaks into the ear may present as otorrhoea or rarely as a nasal leak via the eustachian tube.
CSF rhinorrhoeas were primarily treated by neurosurgeons using a frontal craniotomy and pericranial flap [1]. These procedures involve significant morbidity including prolonged hospitalisation, post-operative anosmia and possible effects of brain retraction. Open procedures also have a higher risk of meningitis. However, it was in the last quarter of the century that with the advancements in endoscopes and high resolution cameras, a bulk of CSF fistulae could be repaired endoscopically through the nose by surgeons [2,3]. These procedures have less morbidity to the patient with no external facial scars and have success rates comparable to the open neurosurgical procedures. However, open repair still has its place today, especially for large leaks or in cases of failed endoscopic procedures.
This study is a series of cases done primarily by the first author over a period of 10 years between 2003 to 2013 during his tenure as a consultant at two tertiary care hospitals namely; Christian Medical College, Vellore and Jawaharlal Institute of Post-graduate Medical Education and Research, Puducherry, Tamil Nadu, India. Though there has been a learning curve in the procedure, the results have remained constant with a single failure occurring after 10 years of first starting the procedure. Large series of CSF rhinorrhoea are still infrequent, and there is still no consensus with regards to technique, if an underlay technique is superior to an overlay technique and whether a postoperative lumbar drain is required or not.
The aim was to analyse the surgical outcomes of endoscopic CSF rhinorrhea closure.
Materials and Methods
The study was a retrospective case audit, wherein, all cases primarily operated by the first author for CSF rhinorrhoea from the year 2003 to 2013 have been included. The outcome of the surgery was measured by the absence of CSF rhinorhea at the end of six months. Duration of the leak, possible etiology regarding trauma preceding CSF leak and meningitis were recorded from the charts. Pre-operative nasal endoscopy findings, Computed Tomography (CT) scan and Magnetic Resonance Imaging (MRI) details for the side, site and size of the leak were noted down. Intra operative notes regarding the findings, the details of the defect, the technique used, presence or absence of meningocele were noted. Postoperative complications, endoscopy findings and CT scan findings were also documented at the end of six months. Every patient seen in the outpatient department with complaints of unilateral watery rhinorrhoea were given a sterile bottle and asked to collect 2-3ml of the nasal discharge. This sample was tested for glucose levels. At the same time, the patients’ blood glucose levels were also checked. It was presumed the fluid was CSF if the discharge appeared clear, colourless and had a glucose value that was more than 50% of the patients’ blood glucose level. Beta 2 transferrin was not available in both centres where the study was done and hence, not used to confirm CSF in the samples. Those patients with suspected CSF leak by the above procedure underwent a CT of the nose and paranasal sinuses with 0.5 mm coronal cuts through the anterior skull base and a MRI of the brain. A combination of CT and MRI scans made it possible to identify the site of the leak and the presence or absence of meningocele in all cases.
Patients were counselled about the need for surgery, and those willing for surgery underwent routine haematological and radiological investigations for determining fitness for surgery. Patients with meningitis at the time of the first visit were offered surgery after three weeks of antibiotics for acute episode while the rest were offered surgery at the earliest. All patients received one dose of H.influenza vaccine and one dose of the polyvalent pneumococcal vaccine once a diagnosis was made. Patients also underwent a rigid nasal endoscopic examination before admission. No antibiotics were prescribed till the time of admission.
On admission, patients were counselled about the need for a postoperative lumbar drain, surgical scar on the thigh and a need for an in dwelling urinary catheter. Surgery was done under general anaesthesia. An 18” gauge lumbar was inserted by an anaesthesiologist at the beginning of the procedure. The drain was connected to a collecting bag and drain closed. After the bladder was catheterized the contralateral thigh was prepared. Fascia lata was harvested using a 5cm vertical mid-thigh incision along the lateral aspect of the thigh. A 2cm X 5cm piece of fascia lata and 2 to 3 pieces of free fat grafts were harvested and placed in normal saline. The wound was closed in two layers and a tight bandage applied.
The nasal cavities were then prepared by placing cotton pledgets soaked with 1: 100,000 adrenaline saline. A diagnostic nasal endoscopy was first done using a 4mm rigid endoscope. On the site of leak, an uncinectomy and middle meatal antrostomy were first done. Once the basal lamina was fully exposed the middle turbinate was resected keeping a small stump superiorly along skull base and also at its lateral attachment near the sphenopalatine foramen. The mucosa of the middle turbinate was carefully separated from the underlying bone and then flattened onto a dry metallic bowl and allowed to dry. A posterior ethmoidectomy and sphenoidotomy were then done and skull base delineated from posterior till the anterior ethmoid artery. The opening of the frontal sinus was then identified and widened. The ostia of the various sinuses were opened so that they were not accidentally occluded while placing the graft.
Now attention was turned to the site of the leak. In cases where the meningocele was seen the identification of the site of leak was easy but those without a meningocele the area was gently curreted and the site identified. The site of leak was identified in all cases. Meningoceles were cauterised with bipolar cautery till they shrank and the opening in the skull base identified. The area surrounding the defect was made raw with a combination of curettes and bipolar cautery to help the graft adhere to it. Circular defects were plugged with fat graft. All those patients who underwent an overlay procedure had a piece of fascia lata placed over the defect that was in turn covered by the middle turbinate mucosal graft. Fibrin glue when available was used in between layers to stabilize the graft. Care was taken to confirm that the frontal, maxillary and sphenoid sinus ostia were not blocked by the graft. The graft was then stabilized by layers of Surgicel and absorbable gelatine. The nasal cavity was then packed with Bismuth Iodoform Paraffin Pack (BIPP). In the two patients with leaks from the sphenoid sinus, the mucosa of the sphenoid was stripped, and after that the defect closed in layers, the sinus was obliterated with fat pieces wrapped in Surgicel. In the patients with leaks from the frontal sinus, the sinus was approached via a brow incision and the floor of the frontal sinus was opened. The leak was repaired again in layers and after removing all mucosa the sinus was packed with fat pieces wrapped in surgicel. In one patient with a CSF leak it was found that the leak was from the ear (Mondini’s aplasia diagnosed on CT) and CSF was leaking from the nose via the eustachian tube. This patient underwent a tympanotomy, and a defect was noted in the middle of the stapes footplate through which there was a profuse CSF leak. The stapes foot plate was removed, and the labyrinth was plugged with fat wrapped in surgicel and then covered with temporalis fascia.
At the end of the procedure the lumbar drain was opened and the patient was transferred to the ward. The patient was advised complete bed rest for five days after which the lumbar drain was removed. Patients were nursed on pneumatic-beds to decrease the risk of bed sores. All patients received postoperative antibiotic (Ceftriaxone), analgesics and stool softeners. Patients at risk for deep vein thrombosis also received low molecular heparin and compression stockings. The nasal pack was removed at the end of five days and thigh sutures on the seventh day. Patients were discharged on the eighth day and advised follow-up after two weeks, one month, and three months and then once in six months. Diagnostic nasal endoscopy was done at the end of one month to assess the nasal cavity for synechiae, patency and graft take up. Post-operative CT scan was advised at the end of six months.
Results
Thirty-four patients were evaluated and underwent treatment during the ten years between 2003 to 2013. The average duration of follow-up was 14 months ranging between 8 months and 46 months.
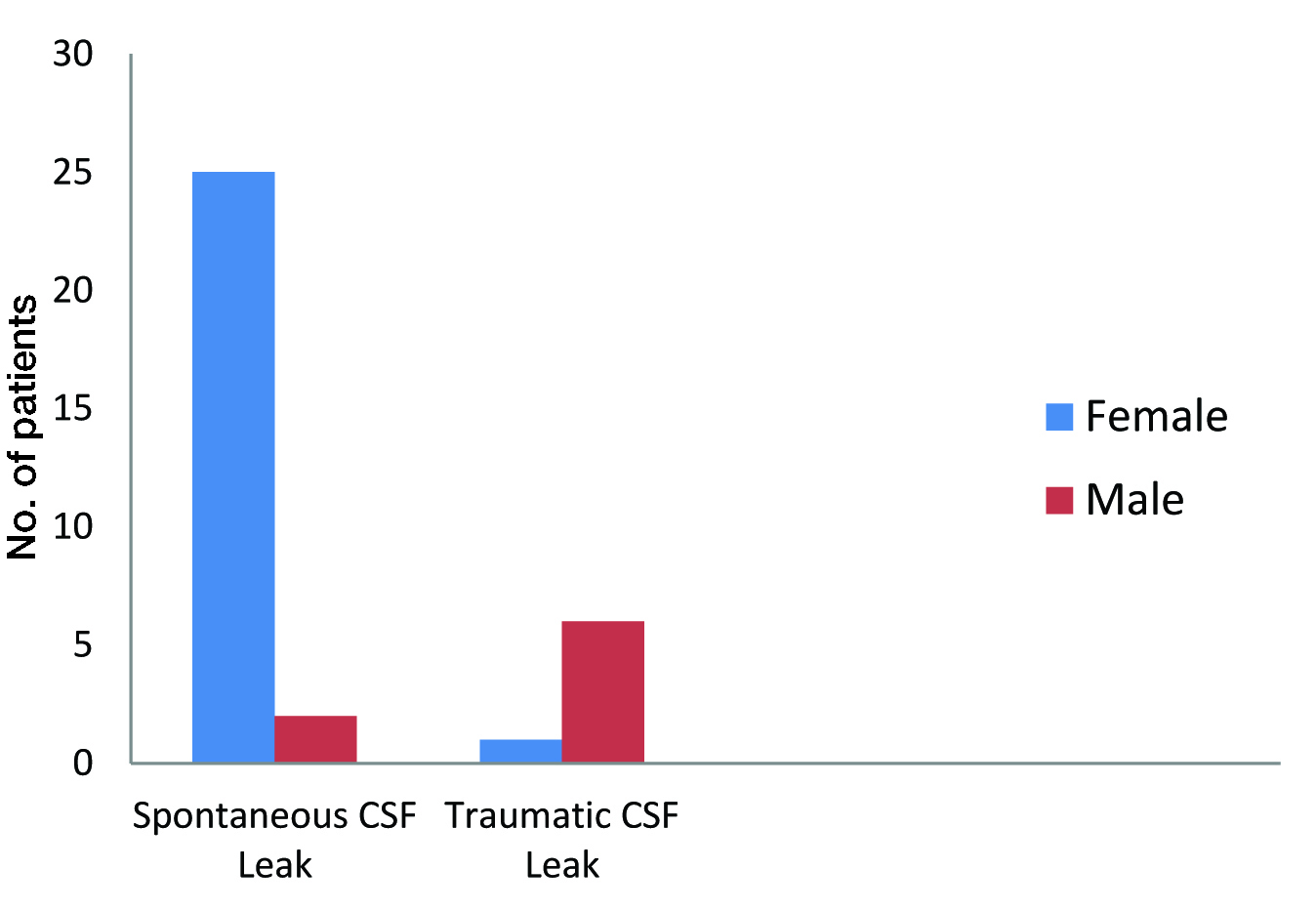
Of the total of 34 patients 26 (76%) were female and 8 (24%) males. A total of 7 (20.6%) patients had a positive history of trauma preceding the CSF leak, of which one was female. Two male patients had a history of endoscopic sinus surgery three months before the onset of the symptoms while the lone female patient with traumatic CSF leak developed one during a medial maxillectomy for a Brown’s tumour of the ethmoid that had led to premature osteoporosis and multiple fractures of long bones. Of the remaining 27 patients with spontaneous CSF leak 25 (92.6%) were female and only two (7.4%) were males [Table/Fig-1].
Incidence in males and females.
Age of the patients ranged from 6 years to 61 years with a mean of 38.9 (±11.57) years. The mean age for males was 31.5 (+12.88) years and 41.2 (±8.49) years for females.
CSF rhinorrhoea is known to lead to bacterial meningitis. Of the 34 patients with CSF rhinorrhoea three patients had a history of meningitis before surgery and was probably the reason for the diagnosis. One patient with CSF oto-rhinorrhoea with Mondini’s aplasia had recurrent episodes of meningitis since childhood, and the last episode led to an extensive search by the physicians to diagnose CSF fistula. A second patient with three episodes of meningitis was a child who had a head injury. This child lost hearing in each ear after the first two episodes and recurrent CT scans missed the leak from the posterior table of a small and developing sinus. A third patient with meningitis developed a possible nosocomial infection following pre-operative nebulisation for brachial asthma after she was admitted for surgery.
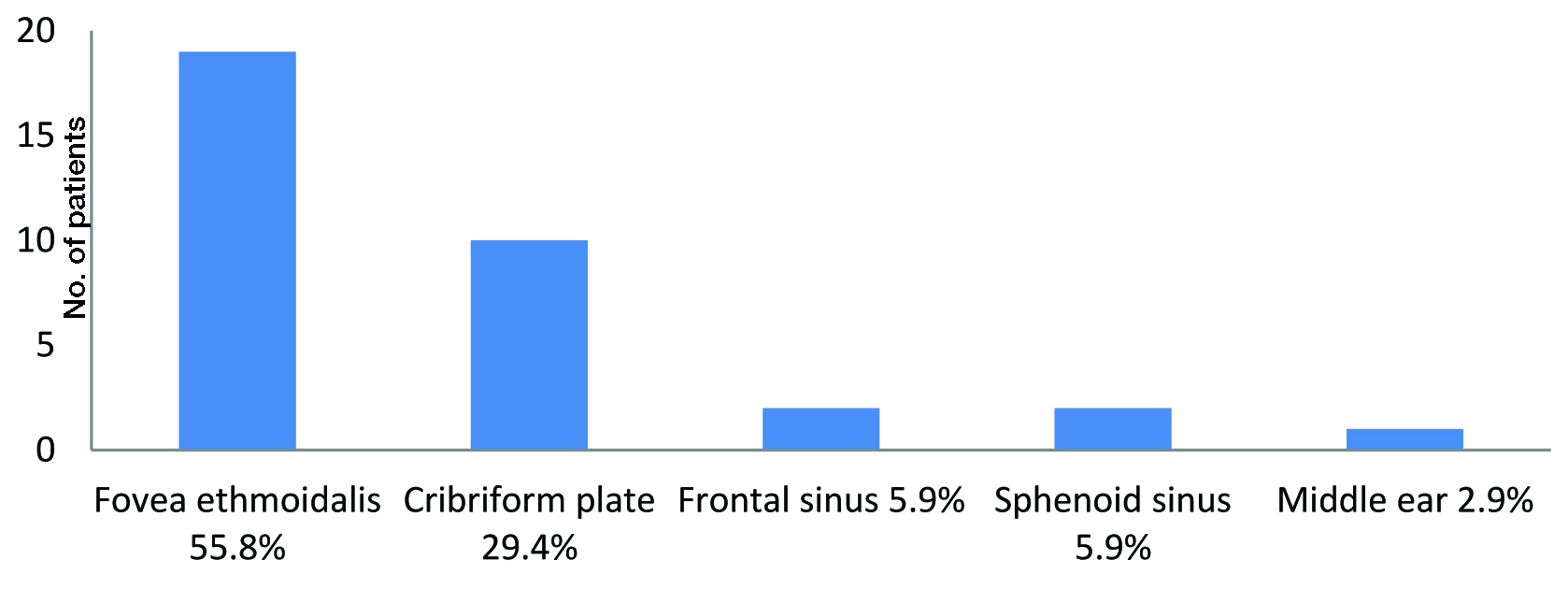
CT scan and MRI scans correlated to the site of the leak with the surgical findings. The commonest site of the leak was in the fovea ethmoidalis in 19 (55.8%) followed by 10 (29.4%) in the cribriform plate, 2 (5.9%) each in frontal and sphenoid sinus and 1(2.9%) from the middle ear [Table/Fig-2].
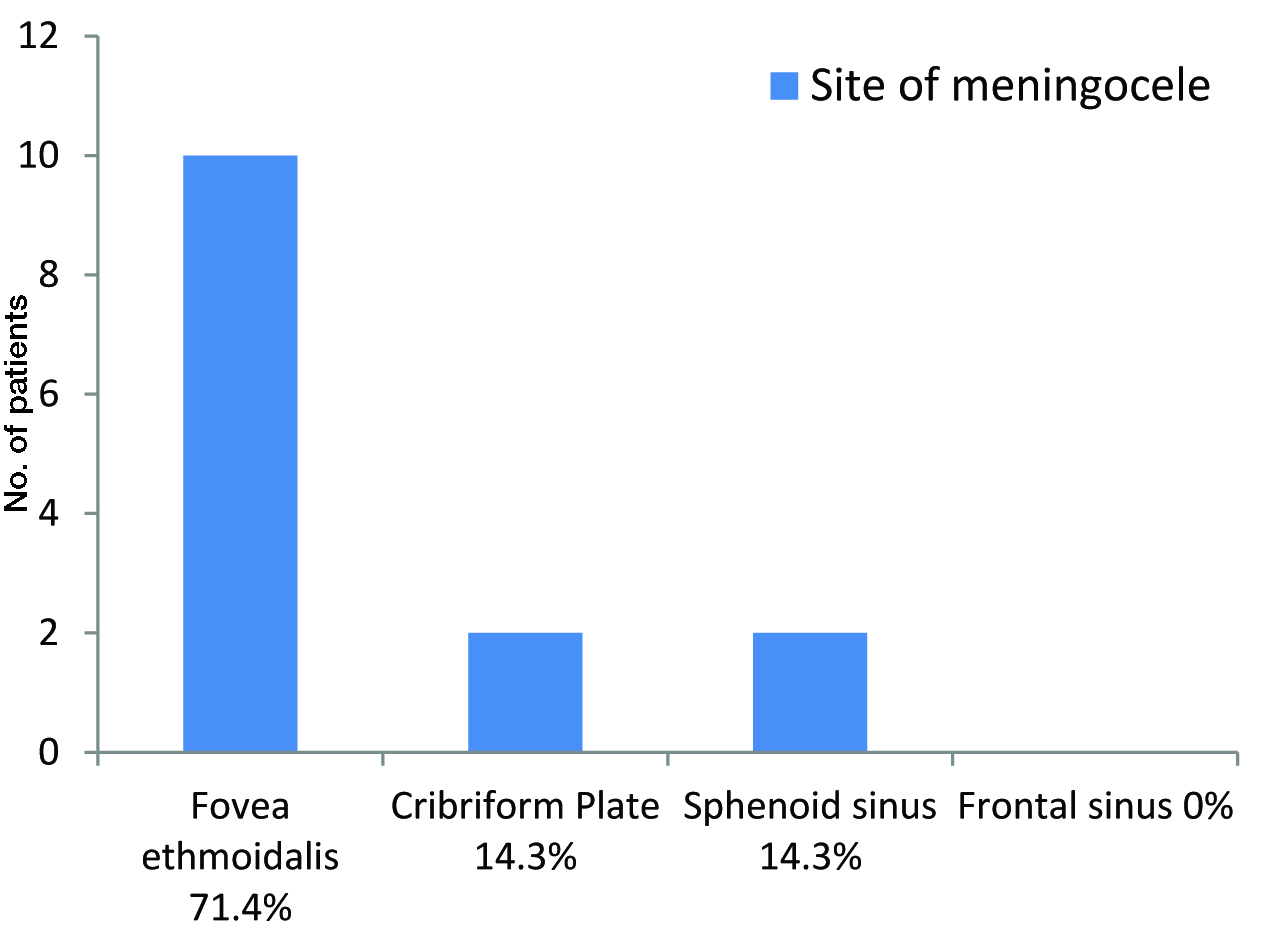
Meningoceles were observed in 14(41.1%) patients and of these meningoceles 10 (71.4%) were from the fovea ethmoidalis, 2 (14.3%) from the cribriform plate and 2 (14.3%) from the sphenoid sinus [Table/Fig-3]. Patients with meningocele, when asked about history of trauma only 2 (14.3%) answered in the affirmative and both of them, were in the Fovea ethmoidalis.
Fibrin glue was used when available due to the high costs involved. A total of 20 (58.8%) patients received fibrin glue while 14 (41.2%) did not. Fibrin glue helped stabilize the graft before packing but did not appear to alter long-term results.
An overlay technique of placing the multiple layers of fascia and mucosa was used in 26 (76.5%) patients and an underlay technique where a layer of fascia was placed between the dura and the cranium was used in the remaining. A plug of fat was used in all cases where there was a definitive circular or oval defect in the bone and also in the frontal sinus, sphenoid sinus and inner ear. Fat graft wrapped in Surgicel was used when large cavities had to be filled like the sphenoid sinus because it helped in handling the fat better.
Of all the 34 patients who underwent the procedure, only one patient had a persistent leak even at the end of three weeks. This patient required a second endoscopic procedure six months later using the same procedure and led to total resolution of symptoms. Analysis of this patient showed that she had a similar leak in the opposite nose which was operated upon by the first author a year earlier, and the patient developed a spontaneous leak on the opposite side a year later. CT scan of this patient revealed a partially empty Sella and signs of raised intracranial tension. Thus, the overall success rate of this series with one surgical procedure was 97 % and 100% with a second procedure. The complications encountered were minor and summarised in [Table/Fig-4].
Complications and management.
| Complication (Number of patients) | Treatment of the complication |
|---|
| Hematoma of the thigh wound (1) | Surgical drainage under local anaesthesia at the bedside |
| Post-operative synechiae in the nasal cavity (3) | Only one required the release of synechiae after six months under local anaesthesia |
| Catheter induced urinary tract infection (1) | Treated with antibiotics |
| Constipation even with stool softeners (6) | Suppositories to help pass stools |
No serious postoperative complications of the procedure like meningitis, brain abscess, bed sores or deep vein thrombosis
Discussion
Endoscopic repair of CSF fistulae is the gold standard for care of patients today. CSF rhinorrhoea is being diagnosed more commonly today when compared to a decade ago because of the increased awareness among ENT surgeons. CSF rhinorrhoea is broadly classified into normal pressure and high-pressure CSF rhinorrhoea. In this series, no attempt was made to measure CSF pressure due to the non-availability of facilities. The normal pressure leaks may follow trauma or may be spontaneous where there is no preceding history of head trauma. Spontaneous CSF leak made up a vast majority of patients (79.4%) in this series of which 92.6% where women. An 11.8% patient had a history of prior head trauma while 8.2% had a history of previous surgery. This is different from series by Saafan ME et al., where 55% patients had spontaneous leaks, 30% following head injury and 15% following iatrogenic injury [4].
The site of the leak was in the fovea ethmoidalis in 55.8% followed by 29.4% in the cribriform plate, 5.9% each in frontal and sphenoid sinus and 2.9% from the middle ear. The most frequent site of the skull-base defect was the cribriform plate (52%), followed by the anterior ethmoid (19%), sphenoid (10%), and posterior ethmoid (3%) in a similar series of 31 patients by Paolo Castelnuovo et al., [5].
Identification of the site of leak pre-operatively is the most important step in the repair process. High-resolution imaging in three dimensional planes helped us in defining the site of the leak. High resolution CT can identify even small defects with high sensitivity. It also provides information regarding anatomical variations and landmarks. Herniation of meninges or brain tissue can be identified better with MRI (T2 weighted). There is a natural contrast plane between CSF and the surrounding tissue that aids in the better identification of the site of the leak [6].
Many studies advocate the use of fluorescein in cases where the site of leaks was difficult to identify [7]. Regarding the intrathecal use of fluorescein, although its efficacy for identification of CSF leaks has been established in the literature, its use remains controversial [6] due to certain complications reported by some authors such seizures, cranial nerve deficits. The time taken for the lumbar puncture and the time taken for diffusion of fluorescein prolongs the duration of surgery. In our series, the use of intrathecal fluorescein was avoided as we could identify the defect in all our cases without the use of fluorescein.
Reduction of CSF pressure and the CSF flow thereby improving graft adhesion in large fistulas can be obtained by post-operative continuous CSF drainage for 1 to 5 days [8,9]. Such continuous CSF diversion has been discouraged by some authors due to the risk of pneumocephalus and reduced closure rates [10,11]. On the other hand, permanent CSF diversion can be used to measure Intracranial pressure (ICP) in select patients. In our series, we used perioperative lumbar drain without any complications as reported by the patients. Better patient outcomes can be seen by proper insertion and removal of drainage catheter and monitoring of CSF volume.
When compared to traditional approaches the rate of post-operative CSF leak reduced to 5% after the introduction of the nasoseptal flap. Pre-operative decision to use this flap should be made so that there is injury to this tissue during surgery thereby reducing its viability. Another disadvantage is the chance of co-existing septal injury in cases of CSF rhinorrhea thereby making this flap less favourable for CSF repair. The same may be said of patients with prior posterior septectomy or sphenoidotomies, procedures interrupt blood supply to the flap, precluding its use [12]. An alternative flap is the Middle Turbinate Mucosal Flap (MTF), which with an average surface area of 5.6 cm2 provides cover for transellar, transplanar and transtubercular defects. The disadvantage of this flap is the presence of bullous turbinates and the highly variable pneumatisation of middle turbinate [13].
We routinely use turbinate flaps for additional support over grafted area. Though the septal mucosa offers an advantage over turbinate flap due to its thickness [14], our results with turbinate mucosa are fair enough that we didn’t have to harvest the septal mucosa thereby leaving behind a raw septum. Either way, each fistula should be treated in a unique way, and there are many different options to seal the fistula.
Fibrin glue promotes wound healing by triggering an inflammatory response [15] and simulating coagulation cascade that has been confirmed by histopathological studies. Even though their primary use is to secure haemostasis, they also act as a sealant for air and fluid leakages. It can also be used as a vehicle for drug delivery. Since, the coagulating mechanism of fibrin glue is independent of body’s clotting mechanism, it is very useful in patients with coagulopathies and patients on anti coagulant treatment [16]. Conservative usage of such tissue adhesives must be followed because thick adhesive layer prevents proper contact of wound bed and graft thereby decreasing graft uptake [17]. Some authors report that there is no specific advantage of using fibrin glue [18].
The success rate in this series was 97% following a single endonasal procedure and 100% following two. No patient needed an open neurosurgical procedure. A similar series by Schoentgen C et al., who looked at a 10 year experience, had 22.5% recurrence of CSF leak and a need for an open surgical procedure in 37.5% patients [19]. In another series by Virk JS, et al., success rate after first surgery was 89% and after second surgery was 100%. [20]. A series by Chaaban MR et al., with a series of 46 patients over five years success following a single endonasal procedure was 93% and 100% with a second procedure [21]. Similar studies worldwide have shown a high rate of success following an endoscopic repair of more than 90% and are today considered the standard of care for CSF rhinorrhoea.
Conclusion
Endoscopic repair of CSF fistulae has become the gold standard of treatment. Meticulous pre-operative evaluation and surgical technique are keys to attaining excellent results. Though large series done around the world have not demonstrated the advantage or disadvantages of a lumbar drain in the post-operative period, our series where the lumbar drain was used in all patients has provided consistent results. No added benefits of the underlay vs. the overlay technique have been demonstrated nor has the use of fibrin glue shown to improve results. The endoscopic repair is a safe procedure and provides consistent results with minimal complications.
No serious postoperative complications of the procedure like meningitis, brain abscess, bed sores or deep vein thrombosis