Congenital Lobar Emphysema: An Approach of Anesthetic Management
Meenakshi Mourya1, Dharam Singh Meena2
1 Senior Resident, Department of Anesthesiology and Critical Care, Safdarjang Hospital and Vardhaman Mahavir Medical College, New Delhi, India.
2 Assistant Professor, Department of Anesthesiology and Critical Care, Safdarjang Hospital and Vardhaman Mahavir Medical College, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Meenakshi Mourya, C-76, South Extension Part-2, NDSE-2, India.
E-mail: drmeenakshi29@gmail.com, tanwar_pranay@yahoo.com
Congenital Lobar Emphysema (CLE) is a medical condition which is quiet rarely seen especially in neonates. The disease is characterized by over inflation of lungs which is produced due to inhibition of escape of inspired air from lungs. This condition usually occurs in infants due to partial obstruction of the bronchus and can be reversed with timely and planned anaesthetic management. Here in, we are presenting a case of an infant who was merely four months of age. CLE was affecting his left upper lobe since birth which was being treated as lobar pneumonia outside at some peripheral health center. The case presented to hospital with the symptoms acute respiratory distress and was taken up for urgent surgical management. Left upper lobectomy was performed which relived his symptoms. Case was discharged from hospital after 10 days of uneventful hospital stay. The case was challenging, as it involved careful and planned anaesthetic management of lung separation as well as prevention of hyperventilation of the un-involved lung.
Lobectomy, Recurrent pneumonia, Respiratory distress
Case Report
A four-month-old infant, weighing 4 kg presented with frequent upper respiratory tract infection and breathlessness. As stated by his mother, the child had recurrent episodes of breathlessness and low grade fever since birth for which she had consulted to a local practitioner. The attendants did not give any history of investigative procedure outside. The child was not diagnosed outside and medical treatment was started based on clinical evaluation only. According to child’s attendant some antibiotics were given, however, no medical records were available. The treatment did not provide any relive to his symptoms. As a result, child was referred to our hospital. On examination, baby was having barrel shaped chest with reduced air entry into both side, however left lung was more compromised. Crepts were present in right upper zone. Chest X- ray [Table/Fig-1a] showed hyper lucent left lung with wide broncho-vascular margin, tracheal shadow was deviated to right side, left upper lobe was herneating into the mediastinal area.
(a): Chest X-ray showing involved right lung with right tracheal shift along with hyperlucent upper lobe of left lung. (b): CT Lung coronal section showing overinflated left upper lobe of lung and compressed right lung. (c): CT Lung axial section showing overinflated left upper lobe (arrow) of lung and compressed right lung.
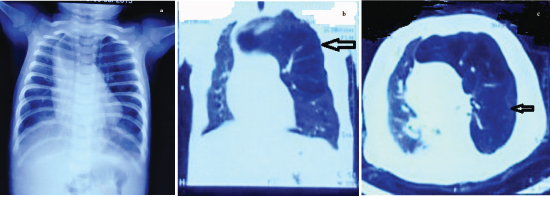
Computed tomography of chest [Table/Fig-1b&c] showed hyper-inflated left upper lobe showing mediastinal shift to right side. In view of above radiological findings and clinical history of symptoms since birth which were not responsive to antibiotics therapy, the diagnosis of Congenital Lobar Emphysema (CLE) was considered. Echocardiography was done to rule out any associated cardiac anomalies, which was within normal limit. Other routine haematological and biochemical parameters were in normal range. In vital parameter, oxygen saturation was 44% in room air. The saturation was 86% in left lateral position in room air and was 98% with oxygen. Arterial blood gas analysis showed pH: 7.34, PCO2: 50.5, PO2: 38.7, HCO3: 26.8.
Resection of the involved lobe of lung.

In view of above clinical symptoms and treatment history, clinical examination and imaging findings diagnosis of CLE was proposed. As there was no history of high grade fever hence diagnosis of lobar pneumonia was ruled out. Normal cardiac shadow and Electrocardiogram (ECG) ruled out any congenital cardiac anomaly. Child was taken up for urgent surgical intervention after informed consent. In operation theatre, child was wrapped in warm cotton and placed on the heated mattress, intravenous access was checked, monitoring was established with pulse oxymetery. Infusion of ringer lactate was started at the rate of 10 ml/kg /h. Rectal paracetamol suppository 80 mg was inserted. Before induction, oxygen supplementation was given and injection glycopyrrolate 0.04 mg given intravenously. General anaesthesia was induced with 4 μg of injection fentanyl with 4% sevoflurane in 100% oxygen via jackson rees circuit. After achieving adequate deep anaesthesia, single lumen without cuff endotracheal tube of internal diameter measuring 3.5 mm was used for intubation. The correct placements of the tube was confirmed by auscultation and fixed at 10 cm from the angle of lip. Gentle assisted ventilation was performed. Child was placed in the right lateral position, anaesthesia was maintained with oxygen and isoflurane 0.2% and was maintaining spontaneous ventilation. Once thoracotomy was done, loading dose of injection vecuronium 0.4 mg (neuromuscular blocker) was given. Further patient was maintained on oxygen, isoflurane and on increasing dose of vecuronium. The peak inspiratory pressure of 21cm was maintained throughout the procedure. Nitrous oxide was added, once left upper lobe was isolated and clamped. Then left bronchus, left pulmonary artery and pulmonary vein were ligated and divided. The involved lobe was overinflated and obstructing airway was surgically removed [Table/Fig-2].
Blood and fluid were monitored and replaced with 120 ml of ringer lactate and 40 ml of whole blood. A left chest drain was placed in situ. After the completion of surgical procedure, all anaesthetic agents were stopped following the reversal by neostigmine 0.2 mg and 0.04 mg glycopyrrolate. The infant was extubated uneventfully. After extubation, child was active with regular and adequate spontaneous respiration, maintaining saturation of 96% on room air. Postoperative chest x-ray showed complete correction of mediastinal shift and compromised right lung return to normal expansion. The infant started breast-feeding on postoperative day-4 was shifted to paediatric ward after 7 days stay of neonatal care unit. The child was discharged on day 10 after uneventful total hospital stay.
Discussion
CLF is defined as a congenital lung abnormality that results in progressive over inflation of lung lobe with contra lateral displacement of the mediastinum and compression of the contra lateral normal lung parenchyma [1]. CLE, a congenital anomaly with prevalence of 1 in 20,000 to 1 in 30,000 [2] usually affects infants and present with symptoms of acute respiratory distress and dyspnea [3], usually associated with cyanosis and asymmetrical breath sounds. The aetiology is usually idiopathic, however, according Doull IJ et al., the ball valve mechanism is produced as a consequence of deficient development of cartilaginous tissue in to the bronchus [4]. This mechanism leads to progressive over-inflation of the affected lung by preventing the escape of inspired air. Most of the cases present in neonatal period with male to female ratio being 3:1 [5,6]. It is most common in the left upper lobe (40-50%) with other sites affected less frequently, right middle lobe (30-40%), right upper lobe (20%) and lower lobes (1%) [7]. CLE has also been reported with other associated anomaly with double superior vena cava and horse shoe kidney [8]. One case is reported with polysplenia, a syndrome characterized by bilateral bi-lobed lungs and bilateral pulmonary atria along with liver which is symmetrically placed in the midline and multiple nodules of spleen [9]. One of the recently reported case series [10] from Belgium found respiratory distress in 100% cases with 40% cases, presented with severe form. This case was not having any other associated congenital anomaly and presented with the symptoms of progressive respiratory distress mimicking that of pneumonia, however, absence of high grade fever and no response to antibiotics was a possible hint which was against pneumonia.
The investigation for diagnostic work up for this condition starts with preliminary chest x-ray which usually shows hyper-inflated lung and mediastinal shift. A CT scan further confirms the finding and localizes the lesion in addition also rules out any other extrinsic cause of airway obstruction. However, Magnetic Resonance Imaging (MRI) might be helpful to access the status of blood supply and vasculature of the affected lobe. In this case, Chest x-ray and CT was done which revealed the CLE of left upper lobe with shifting of mediastinum to right. MRI was not done. Though in our case surgical intervention i.e., lobectomy which is also the operative procedure of choice [11] was done but there are some studies [12] which indicate the medical conservative management for CLE, but there are chances of recurrent chest infection of such cases in future.
Induction of general anaesthesia in infants with congenital lobar emphysema is critical. The over exertional effort in the form of excessive cry especially in infants may lead to progressive increase in amount of trapped gas further worsening the condition of the patient. Even positive pressure ventilation or positive airway pressure by anaesthetist can also increase the severity of emphysema. A smooth inhalational induction such as sevoflurane (florinated halothane) along with oxygen must be used with minimal positive pressure ventilation until the opening of thoracic cavity [13]. Controlled or assisted ventilation may be done if hypoventilation develops may be at the time of intubation [13]. The low airway pressure are especially suitable for such cases, nitrous oxide is usually avoided because it can expand the emphysematous area. The case was a learning experience as it highlighted judicious planning of anaesthetic management and emphasized the use of low pressure manual ventilation to prevent unwarranted diffusion of nitrous oxide in to the emphysematous area as a possible complication.
Conclusion
The successful outcome emphasizes the importance of use of low pressure manual ventilation in management of such cases. The case highlights importance of team approach in the difficult cases like this which yields a rewarding outcome. This case also draws our attention towards the lack of possible screening mechanism during antenatal examination of pregnant female at the community level.
[1]. Cunha Fatureto M, Pinheiro Ferreira D, Amaro Ferraz D, Congenital lobar emphysema: study of a caseRev Port Pneumol 2008 14(6):893-96. [Google Scholar]
[2]. Thakral CL, Maji DC, Sajwani MJ, Congenital lobar emphysema: experience with 21 casesPaediatr Surg Int 2001 17(2-3):88-91. [Google Scholar]
[3]. Chao MC, Karamzadeh AM, Ahuja G, Congenital lobar emphysema: an otolaryngologic perspectiveInt J Paediatr Otorhinolaryngol 2005 69(4):549-54. [Google Scholar]
[4]. Doull IJ, Connett GJ, Wamer JO, Bronchoscopic appearances of congenital lobar emphysemaPaediatr Pulmonol 1996 21:195-97. [Google Scholar]
[5]. Cay A, Sarihan H, Congenital malformations of the lungJ Cardiovasc Sur (Torino) 2000 41:507-10. [Google Scholar]
[6]. Al–Salem AH, Adu-Gyamfi Y, Grant CS, Congenital lobar emphysemaCan J Anaesth 1990 37:377-79. [Google Scholar]
[7]. Monin P, Didier F, Vert P, Giant lobar emphysema--neonatal diagnosisPaediatr Radiol 1979 8(4):259-60. [Google Scholar]
[8]. Ogul H, Sevketbeyoglu H, Ozgokce M, Congenital lobar emphysema association with double superior vena cava and horseshoe kidneyAnn Thorac Surg 2012 94(6):2131 [Google Scholar]
[9]. Choh NA, Choh SA, Jehangir M, Congenital lobar emphysema associated with polysplenia syndromeAnn Saudi Med 2010 30(6):482-84. [Google Scholar]
[10]. Celik M, Dostbil A, Aksoy M, Anaesthetic management in children with congenital lobar emphysemaActa Chir Belg 2015 115(4):279-83. [Google Scholar]
[11]. Mikhailova V, Congenital lobar emphysema in childhoodKhirurgiia (Sofia) 1996 49:8-12. [Google Scholar]
[12]. Bappal B, Ghani SA, Chaudhary R, Congenital lobar emphysema: a review of 10 casesIndian J Paediatr 1996 63:801-08. [Google Scholar]
[13]. Sreevastava DK, Kiran MS, Anaesthetic management of congenital lobar emphysema: a report of two casesMedical Journal Armed Forces India 2005 61:79-81. [Google Scholar]